Chapter 59 Femoral Neck Fractures: When Should a Displaced Subcapital Fracture Be Replaced versus Fixed?
WHAT IS THE GLOBAL BURDEN OF HIP FRACTURES?
Hip fractures occur in 280,000 Americans (>5000 per week) and 36,000 (>690 per week) Canadians annually. By the year 2040, the number of people aged 65 or older will increase from 34.8 million to 77.2 million. Demographic projections by Statistics Canada indicate that, by the year 2041, 1 in 4 Canadians will be older than 65 years. The number of hip fractures is likely to exceed 500,000 annually in the United States and 88,000 in Canada over the next 40 years.1–3 By the year 2040, the estimated annual healthcare costs will reach $9.8 billion in the United States and $650 million in Canada.4
Hip fractures are associated with a 30% mortality rate at 1 year and profound temporary, and sometimes permanent, impairment of independence and quality of life. Furthermore, approximately 30% of surgically treated hip fractures require revision surgery.5 These revisions are associated with a large burden of morbidity and mortality. The disability adjusted life-years lost as a result of hip fractures ranks in the top 10 of all causes of disability globally.
WHAT ARE CURRENT MANAGEMENT OPTIONS?
Although there is general consensus regarding the operative management of nondisplaced fractures of the femoral neck,5 the optimal choice for the stabilization of displaced femoral neck fractures remains controversial.5 Operative approaches for displaced femoral neck fractures include prosthetic replacement (arthroplasty) or internal fixation. Approaches to arthroplasty include unipolar hemiarthroplasty, bipolar hemiarthroplasty, and total hip arthroplasty. Options for internal fixation include multiple screws, a compression screw and side plate, or an intramedullary hip screw device.
WHAT IS THE CURRENT OPINION?
Surveys of surgeon opinions in Denmark, Canada, and the United Kingdom6,7 have been limited by lack of generalizability to other countries and a failure to elicit surgeons’ views of the impact of alternative management strategies on patient-important outcomes. As a result of the limitations of prior surveys, knowledge of the opinions of surgeons managing hip fractures remains limited. Knowing the extent of variability in opinions and practice can identify factors that influence surgeons’ preferences for a particular treatment, serve to educate the orthopedic community on issues regarding the treatment of hip fractures, and assist in the planning of future clinical trials addressing issues that remain unresolved among orthopedic traumatologists.
We conducted an international survey of practicing orthopedic surgeons with an interest in fracture care to clarify current opinion in the treatment of displaced femoral neck fractures.5 Of 442 surgeons who received the questionnaire, 298 (68%) responded. The typical respondent was a North American resident older than 40 years and in academic practice who supervised residents, had fellowship training in trauma, worked in a low-volume center (<100 hip fractures per year), and treated an equal proportion of displaced and undisplaced femoral neck fractures. Most surgeons believed that internal fixation was the procedure of choice in younger patients (< 60 years) across displaced fracture types (Garden types III-IV). Among those patients older than 80 years with Garden type III and IV fractures, almost all surgeons preferred arthroplasty (94% and 96%, respectively). Respondents varied widely in their preferences for patients aged 60 to 80 years with displaced fractures (Garden III/IV) or active patients with Garden III fractures. Many surgeons believed there was no difference between arthroplasty and internal fixation when considering mortality (45%), infection rates (30%), and quality of life (37%).
WHAT IS THE EVIDENCE?
In the hierarchy of evidence for questions about a “therapy” (in this case, a surgical intervention), a meta-analysis of randomized, controlled trials is the standard when no single large definitive trial exists. Our search identified 4 meta-analyses and 58 randomized trials that provide information on surgical treatments for femoral neck fractures. Three meta-analyses directly address the question of internal fixation versus arthroplasty in patients with displaced femoral neck fractures.8–10 Their results are consistent. Here, we present the current results of the single meta-analysis of randomized trials.8
Mortality
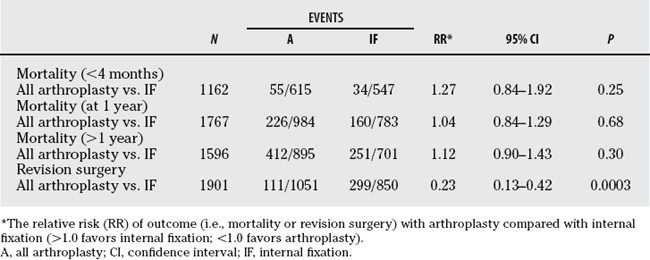
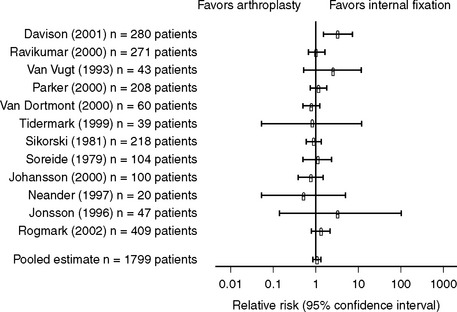
Nine trials (N = 1162 patients) provided postoperative mortality data at 4 months or less. The results of the pooled statistical analyses are listed in Table 59-1. Arthroplasty showed a trend toward increased mortality when compared with internal fixation (relative risk [RR], 1.27; 95% confidence interval [CI], 0.84–1.92; P = 0.25; homogeneity P = 0.45). Twelve trials (N = 1767 patients) provided 1-year mortality data. At 1 year, arthroplasty did not increase the risk for mortality when compared with internal fixation, with wide variability between studies (RR, 1.04; 95% CI, 0.84–1.29; P = 0.68; homogeneity P = 0.03) (Fig. 59-1).
Revision Surgery
All 14 studies (N = 1901) provided information on revision surgery (see Table 59-1). Arthroplasty substantially reduced the risk for revision, and the results were consistent from study to study (RR, 0.23; 95% CI, 0.13–0.42; P = 0.0003; homogeneity P < 0.01). Thus, arthroplasty reduced the RR of revision surgery by 77% when compared with internal fixation. The risk difference of 18% translated into a number needed to treat (NNT) of 5.6, which meant that for every 6 patients treated with arthroplasty, 1 revision surgery could be avoided.
UNCERTAINTY AND FUTURE RESEARCH
What Is the Optimal Choice of Internal Fixation (Multiple Screws or Sliding Hip Screws) for Fixation of Hip Fractures?
Parker and colleagues’11 meta-analysis evaluated 28 trials (N = 5547 patients) and reported no advantage of any internal fixation technique over any other. The trials were small (sample size range, 33–410) and methodologically limited.
What Is the Optimal Choice of Arthroplasty (Total Hip Arthroplasty or Hemiarthroplasty) for Treatment of Hip Fractures?
Current best estimates of treatment effect suggest that total hip arthroplasty reduces hip pain (RR reduction, 24%; 95% CI, 2–41%) and may reduce functional limitations (RR reduction, 10%; 95% CI, 24% to −6%) when compared with hemiarthroplasty. The reduction in pain and improvement in function may come at the cost of an increased risk for hip dislocation (RR, 2.95; 95% CI, 0.40–21.74). Despite the trend toward an increase in hip dislocation, the data (point estimate) shows a trend toward a decreased reoperation rate with hemiarthroplasty, though the sparse data are associated with wide CIs (RR reduction, 14%; 95% CI, 53% to −59%).12,13
Table 59-2 provides a summary of recommendations for the treatment of femoral neck fractures.
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
In patients older than 65 years with displaced femoral neck fractures, evidence suggests:
1 Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: A world-wide projection. Osteoporos Int. 1992;2:285-289.
2 Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;252:163-166.
3 Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897-902.
4 Emmanuel A, Papadimitropoulos BSP, Coyte PC, et al. Current and projected rates of hip fracture in Canada. CMAJ. 1997;157:1357-1363.
5 Bhandari M, Devereaux PJ, Tornetta P3rd, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87:2122-2130.
6 Laursen JO. Treatment of intracapsular fractures of the femoral neck in Denmark: Trends over the past decade. Acta Orthop Belg. 1999;65:478-484.
7 Chua D, Jaglal SB, Schatzker J. An orthopedic surgeon survey on the treatment of displaced femoral neck fracture: Opposing views. Can J Surg. 1997;40:271-277.
8 Bhandari M, Devereaux PJ, Swiontkowski M, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. J Bone Joint Surg Am. 2003;85A:1673-1681.
9 Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck: A meta analysis of 106 published reports. J Bone Joint Surg Am. 1994;76A:15-25.
10 Masson M, Parker MJ, Fleischer S. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev.; 2; 2003; CD001708.
11 Parker MJ, Blundell C. Choice of implants for internal fixation of femoral neck fractures: Meta analysis of 25 randomized trials including 4,925 patients. Acta Orthop Scand. 1998;69:138-143.
12 Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur—13 year results of a prospective randomised study. Injury. 2000;31:793-797.
13 Keating JF, Grant A, Masson M, et al. Displaced intracapsular hip fractures in fit, older people: A randomized comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess. 2005;9:iii-iv. ix-x, 1–65,