39 Fascia Iliaca Block
Suggested Technique
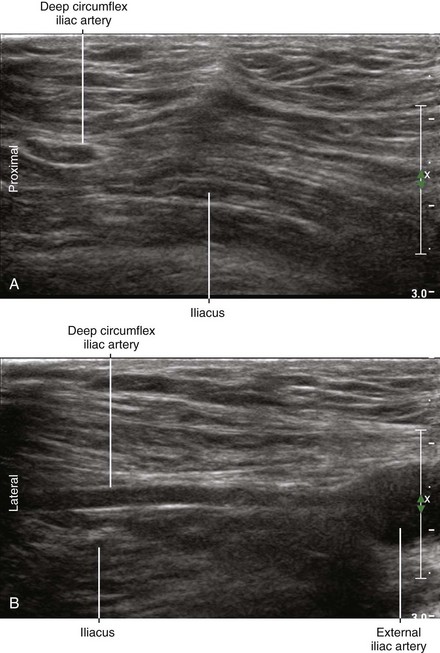
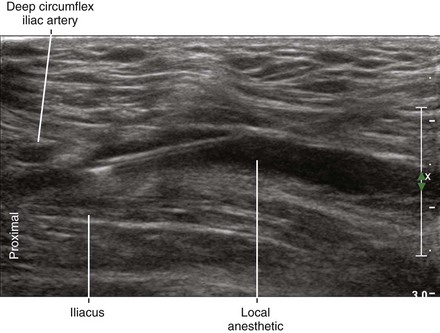
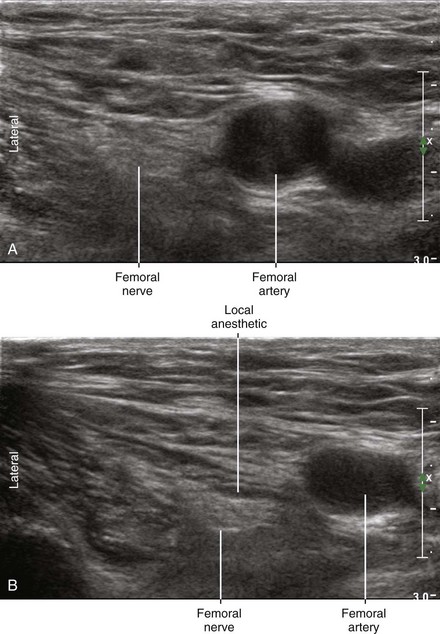
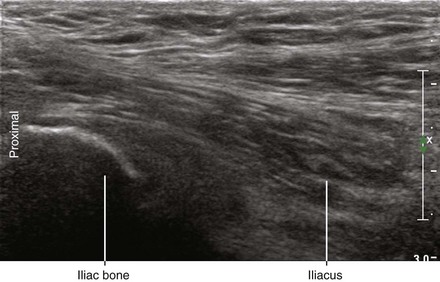
The patient is placed in supine position (flat with slight extension of the hip). Pannus retraction or reverse Trendelenburg position may be necessary in overweight patients. Place the transducer longitudinally to image the iliacus muscle lateral to the femoral nerve. Because of the inclination of the iliacus muscle, this region is slightly more superficial than the femoral nerve. The iliacus muscle forms a ridge because of the underlying bone of the superior pubic ramus. The deep circumflex artery lies superficial to the fascia iliaca 1 to 2 cm proximal to the inguinal ligament. This artery is 2 to 3 mm in diameter and lies on the central side of the iliacus ridge. Tilting the transducer laterally enhances imaging of the fascia iliaca due to its inclination.1
In-plane approach from distal to proximal is used. For this block it is critical that the needle tip be positioned between the fascia iliaca and iliacus muscle,2 just distal to the position of the deep circumflex iliac artery. The needle travels under the inguinal ligament, which lies over the ridge of the iliacus muscle. There is a handedness to this longitudinal approach (right handed for right-sided block, left handed for left-sided block).
Clinical Pearls
• Suprainguinal injection under the fascia iliaca is an effective way to anesthetize the LFCN and femoral nerve. The correct injection has a lens (or spindle) shape.
• The deep circumflex iliac artery is an important landmark for needle tip placement. It can be identified superficial to the fascia iliaca 1 to 2 cm proximal to the inguinal ligament.
• Fascia iliaca block can be performed before sciatic nerve block to reduce patient discomfort during needle insertion.
1 Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66(4):300–305. doi: 10.1111/j.1365–2044.2011.06628.x. Epub 2011, Feb 24
2 Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69(6):705–713. Erratum in: Anesth Analg 1990;70(4):474.