Chapter 26 Family Planning
REVERSIBLE CONTRACEPTION, STERILIZATION, AND ABORTION
When birth control methods in sexually active women are grouped into tiers based on their efficacy with typical use (Table 26-1), it becomes obvious that the most efficient methods are those that are long-term, convenient, and do not require any ongoing action from the woman (Tier 1). For example, the intrauterine devices (IUDs) and progestin implants provide the highest level of pregnancy protection, with first-year failure rates in typical use of less than 1% (Table 26-2). Other hormonal methods, such as the once-every-3-months injection, monthly vaginal rings, weekly patches, and daily pills are in tier 2. Each of these hormonal methods has the potential for very low pregnancy rates (1%), but in typical use, they have first-year failure rates of 7% to 8%. Tier 3 contraceptive methods are the barrier and behavioral methods. Here the differential between the potential that the method offers and what is really seen is widest. For example, male condoms have a less than 2% failure rate if used correctly and consistently with every episode of intercourse. However, in real life, the pregnancy rate is 17.4%. Female barrier methods (diaphragms, cervical caps, shields, and female condoms) have higher pregnancy rates. Interestingly, behavioral methods such as coitus interruptus and fertility awareness methods have rates that are almost equivalent to many barrier methods in typical use.
| Tier | Method of Contraception |
|---|---|
| 1: Longer term | Progestin implants and intrauterine devices |
| 2: Combined hormonal | |
| 3: Barrier and behavioral |
TABLE 26-2 CONTRACEPTIVE FAILURE RATES COMPARING TYPICAL USE AND PERFECT USE
| Contraceptive Method | Percent Failure within First Year of Use | |
|---|---|---|
| Perfect Use | Typical Use | |
| No method | 85 | 85 |
| Male sterilization | 0.10 | 0.15 |
| Female sterilization | 0.5 | 0.5 |
| Copper ParaGard T 380A IUD | 0.6 | 0.8 |
| Levonorgestrel-releasing IUD | 0.1 | 0.1 |
| DMPA | 0.3 | 6.7 |
| OC—combined | 0.3 | 8.7 |
| OC—progestin only | 0.5 | 8.7 |
| Diaphragm with spermicide | 6 | 16 |
| Condom—male, latex | 2 | 17.4 |
| Cervical cap—parous | 26 | 32 |
| Cervical cap—nulliparous | 9 | 16 |
| Spermicides | 15 | 29 |
| Fertility awareness | 19 | 25.3 |
| Withdrawal | — | 18.4 |
DMPA, depot medroxyprogesterone acetate; OC, oral contraceptive.
1. Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77(1):10–21
2. Hatcher RA, Trussell J, Nelson AL, Cates W Jr, Stewart FH, Kowal D. Contraceptive Technology, 19th ed. NewYork, Ardent Media, Inc. 2007.
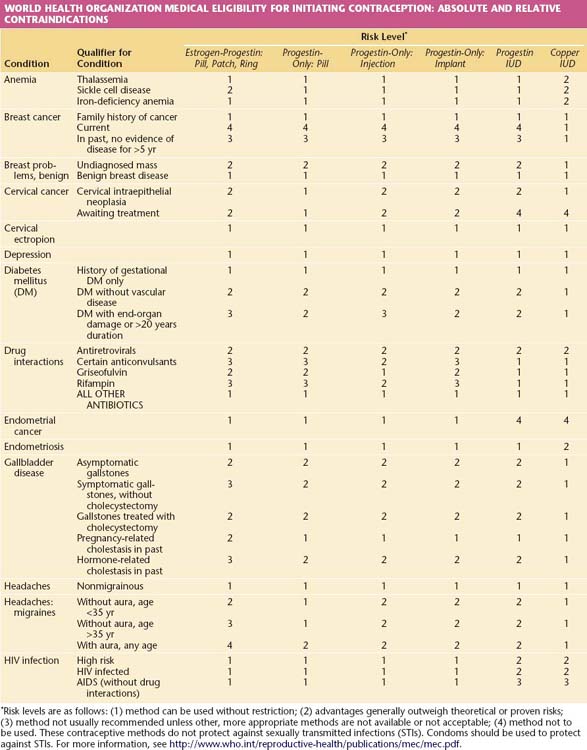
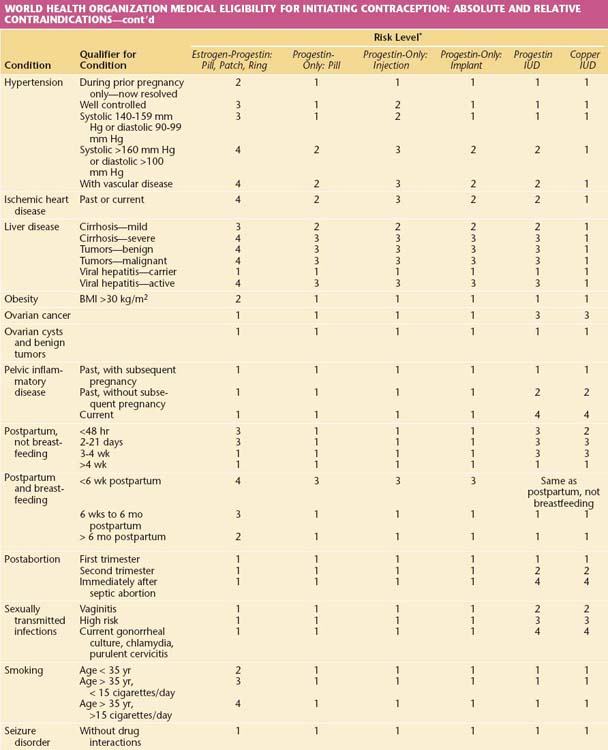
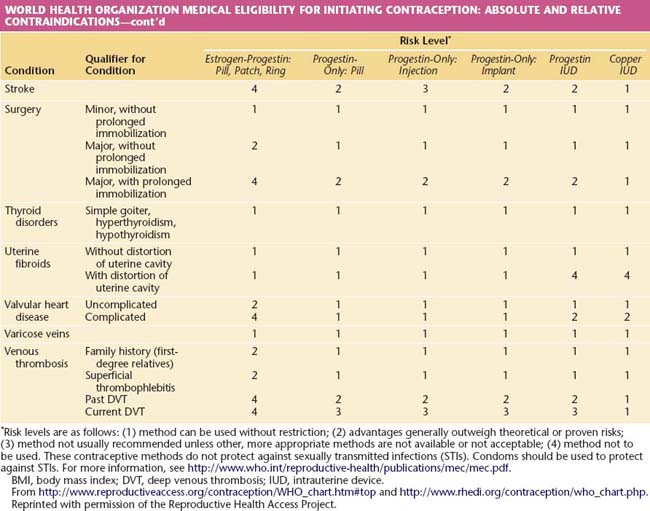
The safety of all methods of family planning is well established. In selecting options for an individual woman, the requirement is that any method offered must be safer to the woman’s health than pregnancy. It is from that perspective that the World Health Organization (WHO) has developed its Medical Eligibility Criteria (MEC; Table 26-3), which rates the appropriateness of each major contraceptive method in a variety of medical circumstances. Recommendations are made on a 1 to 4 scale, in which a rating of 1 indicates approval and 4 represents an absolute contraindication. This rating often differs from the labeling for individual products, which generally reflects theoretical concerns and desires by the manufacturers to protect themselves from product liability. Prescribers should act on evidence-based recommendations such as the WHO MEC.
TABLE 26-3 WORLD HEALTH ORGANIZATION MEDICAL ELIGIBILITY FOR INITIATING CONTRACEPTION: ABSOLUTE AND RELATIVE CONTRAINDICATIONS
 Contraception
Contraception
TIER 1 CONTRACEPTIVE OPTIONS
Intrauterine contraceptives and implants are the most effective, reversible methods available to women at risk for pregnancy. Typical failure rates closely correspond to those seen with correct use (see Table 26-2). Each is also very safe and can be used by women with serious medical conditions for whom pregnancy may be very dangerous.
Intrauterine Contraceptives
The Copper T-380A IUD (Figure 26-1) is approved by the U.S. Food and Drug Administration for 10 years of use, but studies show it remains very effective for at least 20 years. This IUD provides excellent pregnancy protection that is convenient and rapidly reversible. First-year failure rates are 0.7%, and cumulative 10- to 12-year pregnancy rates are 1.4% to 1.9%. Most women are candidates for IUD use, including those with serious medical problems such as hypertension, morbid obesity, diabetes, stroke, myocardial infarction, and cancer. The only absolute contraindications to immediate IUD placement are active infection or cancer in the cervix or uterus, distortion of the uterine cavity, or a uterine cavity that is not the correct size (6 to 9 cm in depth) to accommodate the device.
TIER 2 CONTRACEPTIVES: COMBINED HORMONAL PRODUCTS AND PROGESTIN-ONLY INJECTIONS AND PILLS
Combined Hormonal Products
For healthy reproductive-aged women, combined hormonal contraceptives are very safe. The only measurable risk is the slightly increased incidence of venous thromboembolism (VTE)—deep venous thrombosis and pulmonary embolism. This risk is overshadowed by the risk for VTE during pregnancy. Benign hepatic tumors are an extremely rare problem, and symptomatic cholelithiasis and mild hypertension may be slightly increased. Modern lower-dose hormonal contraceptives do not increase the risk for breast cancer, cholelithiasis, fibroids, or heart attacks in healthy women. Women with preexisting medical problems such as hypertension or diabetes and older women who smoke or are obese face higher risks and require individualized recommendations. The WHO MEC in Table 26-3 provides guidance.
 Sterilization
Sterilization
Permanent sterilization is the most common method of birth control used by U.S. women older than 30 years. Common methods of fallopian tube sterilization are listed and described in Table 26-4.
| Surgical Approach | Technique | Surgical Procedure |
|---|---|---|
| Laparotomy | Pomeroy | Ligature around a “knuckle” (or loop) of tube; excision distally |
| Madlener | Crushing and ligature of loop of tube | |
| Irving | Double ligation, excision between; proximal end buried in myometrium; distal end buried in broad ligament | |
| Uchida | Tubal serosa stripped from muscular coat; tubal segment excised; proximal end ligated and buried in broad ligament | |
| Fimbriectomy | Ligation of distal end of tube and mesosalpinx; excision of fimbriated end | |
| Laparoscopy | Electrocoagulation | Electrical “burn” of two adjacent segments with or without transection |
| Falope ring | Loop of tube drawn into applicator tube; plastic ring placed around both limbs of loop | |
| Hulka clip | Plastic crushing clip placed across tube (not a loop); kept closed by steel spring | |
| Filshie clip | Titanium clip placed across the tube; associated with increased risk for infection | |
| Minilaparotomy | Pomeroy ligation; electrocoagulation | As above |
| Transcervical | Insertion of tubal plug | Placement of plug through a hysteroscopic transcervical approach that causes fibrosis over time |
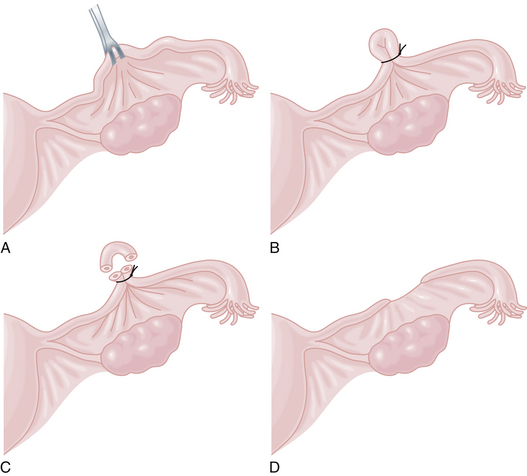
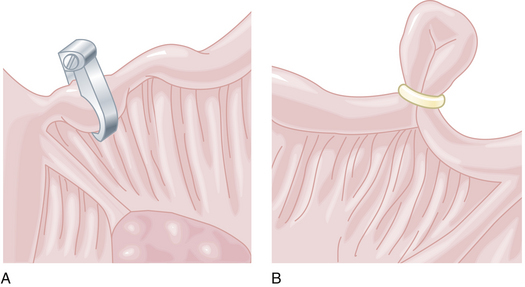
Fallopian tube procedures are most commonly used for female sterilization, although hysterectomy performed for other indications also sterilizes a woman. Tubal interruption can be done through a mini-laparotomy incision, using a laparoscope or hysteroscopically. Usually, mini-laparotomy techniques with suture ligation and interruption of the tube (the Pomeroy technique; Figure 26-2) are performed through a small subumbilical incision immediately postpartum. Laparoscopic approaches are usually performed as interval procedures in nonpregnant women when the woman’s uterus lies in the pelvis. The fallopian tubes can be interrupted with cautery, clips, or rings (Figure 26-3). With the hysteroscope, small plugs can be anchored in the proximal portions of the tube to incite fibrosis and, over time, cause the tube to occlude.
 Abortion
Abortion
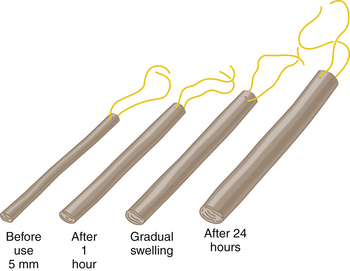
Aspiration with a manual vacuum or suction curettage is more than 99% effective in early pregnancy after cervical dilation has been achieved with misoprostol or laminaria (Figure 26-4). This type of procedure can be performed either under local anesthesia (paracervical block) or under sedation with the patient awake. Complication rates are very low, but the patient must understand that hemorrhage, infection, uterine perforation, retained products of conception, and anesthetic complications are possible. Early pregnancy termination is safer than continuing the pregnancy or undergoing tonsillectomy. There are no long-term adverse effects on women’s reproductive health with uncomplicated procedures.
Abbott J. Transcervical sterilization. Curr Opin Obstet Gynecol. 2007;19:325-330.
Hatcher R.A., Trussell J., Nelson A.L., et al. Contraceptive Technology, 19th ed. New York: Ardent Media; 2007.
Hatcher R.A., Zieman M., Cwiak C. A Pocket Guide to Managing Contraception. Tiger, GA: Bridging the Gap Foundation; 2005.
Speroff L., Darney P.D. A Clinical Guide for Contraception, 4th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005.