CHAPTER 5 Family Context in Developmental-Behavioral Pediatrics
Children’s health and development are a family affair. Whether it involves keeping scheduled appointments for a child’s immunizations, managing feeding difficulties in a child with Down syndrome, or negotiating an adolescent’s desire for autonomy, the daily life of the family is integrally intertwined with the health and well-being of children and adolescents. Family-level factors such as direct and open communication and availability of support have been found to be associated with a host of child health outcomes, including infant mortality,1 lifetime hospitalizations,2 and the likelihood of developing posttraumatic stress symptoms after the diagnosis of a life-threatening illness.3 There are several ways to consider family contributions to children’s development.
First, families are responsible for providing food, shelter, and stability for children. At its most basic level, the provision of basic resources means that the family holds the key to children’s nutritional status and physical comfort. However, families do not always have complete control over available resources; parent’s educational backgrounds, their economic circumstances, and characteristics of the neighborhood also have influences on children’s health.4 Thus, a consideration of family influences on children’s health and development must also include the environments in which families live. Second, families are the holding place for children’s emotional development. Children learn to trust others and regulate their emotions in the safe surroundings of their home before venturing out to school and other social environments. For some children, this is a relatively positive experience, and they come to school well equipped to meet academic and social challenges. For other children, inconsistent and erratic experiences in the home often leave them ill equipped to interact with others, which thus places them at risk for school failure, behavioral problems, and strained peer relationships.5 In all cases, these experiences are mutually influential: Characteristics of the child influence the family, and the family influences the child’s development. Third, family members create practices and hold beliefs that often extend across generations and are influenced by culture. Family life is organized in such a way that it builds on past experiences, which results in predictable routines and imparting of values through recounting personal experience. Many families benefit from their heritages and can use them as guides in meeting the challenges of raising their children. For some families, however, personal histories of neglect, substance abuse, and parental psychopathology interfere with the constructive transfer of generational knowledge and can place children at risk for poor health and development.6–8
The empirical study of family influences on children’s development is complicated at best. Identifying who is in the family; whether to rely on direct observation of family interactions or parent’s report of family climate; how to resolve inconsistencies in reports by mother, father, child, and teacher about child behavior; and adaptation of techniques across cultures9 are just a few of the thorny issues in the scientific study of families. In addition, the changing demography of American families includes increasing numbers of children who are being raised by parents of different ethnic backgrounds, in single-parent households, or in multiple households.10 For the medical clinician, keeping track of all the layers of family life can seem like an overwhelming task, particularly in the short amount of time allocated for patient visits. Rather than ignore the apparent complexity of family life, in this chapter we offer some guidelines for the busy clinician to consider in his or her contact with children and their families. Because the importance of establishing partnerships with families is the cornerstone of pediatric practice,11 a greater understanding of how families operate is in order.
In the past there was a tradition in developmental studies to equate poor child outcomes directly with poor parenting. Such terms as “refrigerator mothers” were coined to suggest that parents (most notably mothers) with cold and harsh parenting techniques were the sole progenitors of their children’s ill health, mentally and physically.12 Childhood schizophrenia was thought to develop from rejecting and harsh parenting styles. Pediatric asthma was thought to arise from overcontrolling and smothering parenting styles.13 At the root of these notions was the assumption that parenting effects were always direct and unidimensional and that neither characteristics of the child nor the surrounding environment had much of an effect on development. Clearly, these notions are outdated because advances in behavior genetics suggest heritability quotients for such conditions as schizophrenia and that symptom severity in asthma is the result of complex interactions among environmental conditions, genetic factors, and family factors.14 The point is that parents do not directly cause their child’s poor health or maladaptive development; rather, children’s health and well-being are embedded in a family context that is subject to a variety of influences, some of which we outline in this chapter.
This chapter is structured in the following ways. First, we provide an overview of a theoretical framework that we believe can be of use for clinicians as they think about the complexities of family life. We first review the social-ecological model originally proposed by Bronfenbrenner.15 This theoretical model is useful in that it allows clinicians to consider not only how the child is situated in the family but also how the family is influenced by the neighborhood in which it lives, the schools that are available to the child, and the culture with which the family most closely identifies. Second, we also consider that children and families change. They do so as part of a process whereby families influence the growth and development of their children and the characteristics of the child also influence how the family functions. This process has been labeled transactional, which suggests that development is characterized by a series of active exchanges between parents and children and that both child and parent contribute to a child’s condition at any given point in time. Thus, we also outline the transactional model as originally proposed by Sameroff and colleagues.16,17 Integrally linked to the social-ecological and transactional perspectives is the role that multiple risk factors play in development. Optimal and poor outcomes are rarely the result of a single factor; rather, the multiple influences of culture, economic resources, family support, and child characteristics cumulatively affect development over time. Thus, we consider the compound effect of environmental risks.
After this strong theoretical grounding in the social-ecological and transactional models and family systems principles, we review some of the literature that illustrates family effects on child health and well-being. Specifically, we examine family factors that promote adjustment in children with a chronic illness, parenting variables that can reduce the risks associated with poverty, and how cultural beliefs and practices enacted in the family context can influence child health and well-being. We conclude with recommendations for clinicians in their clinical decision-making process with families, as well as policy makers responsible for the health and well-being of children. Throughout the chapter, we use vignettes to illustrate our points and to elucidate these complex concepts. Consider the following scenario:
SOCIAL-ECOLOGICAL MODEL
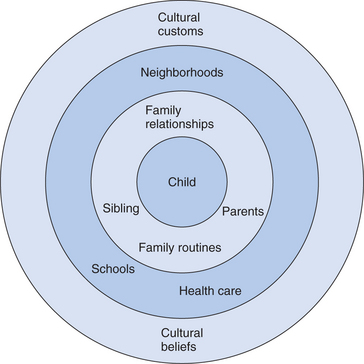
In this brief scenario, we have several elements of Bronfenbrenner’s social-ecological model (Fig. 5-1). The child is at the center of the model. The child’s development is proposed to be influenced by the persons most immediately around him. In this case, Jamie’s development is affected primarily by his mother and siblings. The child’s developmental status is influenced by how responsive his mother is to his needs, as well as by the support and opportunities provided by interactions with his siblings. However, the degree to which the mother is emotionally available to interact with the child in a warm and responsive way may be influenced by her relationship with her ex-husband. We know, for example, that marital conflict can have detrimental effects on children’s development by disrupting effective parenting styles and setting the stage for poor emotion regulation by children.18 Thus, the environment closest to the child’s daily experiences may have a direct influence on his development through exposure to supportive and warm interactions or through a home environment that is characterized by conflict and disruptions. These interactions do not operate in isolation but are influenced by the next level of Bronfenbrenner’s model.
Once we move out of the immediate confines of the family home, we note that there are other influences on child development that can have profound effects on the development of children. This is the level most commonly encountered by pediatricians, inasmuch as how families interact with health care teams also affects how children cope with chronic illnesses.19 In the preceding example, the likelihood that Jamie will develop to his fullest potential will depend not only on his family’s best intentions but also on their ability to gain access to early childhood programs in their neighborhood. Transporting a 4-year-old child five blocks to the home of a babysitter, who must in turn put him on a bus for a long ride for a 3-hour early intervention program, represents a daily challenge. Even under the most optimal home conditions, this would be an added strain to the system that may compromise the child’s developmental progress. Thus, the degree to which the resources available outside the home support, or derail, family investments can have a direct influence on child developmental outcomes.
There is a third level to the social-ecological model that can also influence child development. This layer of the social environment includes such factors as culture, social class, religion, and law. In the preceding example, the legal system has an indirect influence in that public laws guarantee access to public education for all children, regardless of developmental condition. However, as noted previously, gaining access to available education programs can be tempered by resources available in the neighborhood. Culture and religion can also influence child development indirectly. In the case of Jamie, we noted that his mother held strong religious beliefs. Religious beliefs may affect how parents cope with the daily care of children with special needs, so that practices endorsed by mandated programs must also coincide with deeply held doctrines.20
Transactional Model of Development
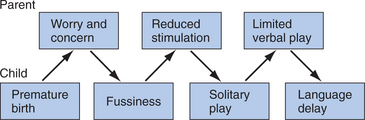
Was the cause of Joanna’s language delay her prematurity and low birth weight? It is known that premature children are at greater risk for developing language delays than are full-term infants.21 Or was the cause of her language delay her fussiness and difficult temperament? Or being less favored than her older brother? Or being left alone? From a transactional perspective, all of these features may come into play when a child’s developmental outcome at any given point in time is considered. In this case, the parents have reasonable concern about their vulnerable infant. Rather than being able to bring their infant directly home, they had to wait and ponder their daughter’s health. Seeking information through the Internet or hospital personnel, they discovered that premature infants are sensitive to light and sound. In this case, Joanna’s fussiness was interpreted by her parents as further indication of her need to have reduced exposure to stimulation, and thus they put her down in the crib frequently. There were fewer opportunities for social interaction and verbal play. This was interpreted as a temperamental difference or perhaps a gender difference in comparison to her brother. Without adequate opportunities for verbal play, Joanna did not develop an age-appropriate vocabulary; thus, her overall language abilities were delayed. This process is outlined in Figure 5-2.
The transactional model as proposed by Sameroff and colleagues16,17,22 emphasizes the mutual effects of parent and caregiver, embedded and regulated by cultural mores. In this model, child outcome is predictable by neither the state of the child alone nor the environment in which he or she is being raised. Rather, it is a result of a series of transactions that evolve over time, with the child responding to and altering the environment. For pediatricians, this model is important because it gives due recognition to the child’s effect on the environment, as well as to the environment’s effect on the child. Pediatricians are frequently faced with situations in which parents feel ill equipped to deal with the challenges of parenting, assuming that childrearing is a one-dimensional task that should conform to a set of prescribed principles easily accessible through a book or the Internet. Typically, this naive view is quickly cast aside with the birth of a second child and parents realize that a one-size-fits-all approach to parenting is rarely successful. Thus, to be able to predict how families influence children, the investigator must also ask how children influence families and how this process develops over time. In addition to recognizing that parents and children mutually influence each other, the transactional model is also important in highlighting the multiply determined nature of risk in family environments.
Multiply Determined Nature of Risk in Family Environments
ADOLESCENT ACADEMIC ACHIEVEMENT AND PSYCHOLOGICAL ADJUSTMENT
In a large study of adolescents in Philadelphia, the relation between exposure to a variety of risk factors and both academic achievement and psychological adjustment was examined.5 Using an ecological framework, the researchers identified six domains of risk: family process, parent characteristics, family structure, management of community (e.g., social networks), peers, and community (e.g., neighborhood). Adolescents were assigned risk scores for each domain. Lack of autonomy, low-level parent education, single marital status of parents, lack of informal networks, few prosocial peers, and low census tract socioeconomic status are examples of high risk in each of the domains. Increasing numbers of risk factors was associated with large declines in academic performance and psychological adjustment. Using an odds-ratio analysis, the authors compared the likelihood of poor outcomes in high-risk environments with those in low-risk environments. For academic performance, they found that a poor outcome increased from 7% in the low-risk group (three or fewer risk factors) to 45% in the high-risk group (eight or more risk factors)—an odds ratio of 6.7 to 1.
Two factors that are repeatedly identified as contributors to children’s well-being are parental income and marital status. Research on multiple risk factors highlights, in part, how income and marital status are embedded in larger social ecologies that act in concert with other risk and protective factors. This is important in consideration of family effects on child health and development, inasmuch as marital status and economic stability are commonly viewed as structural family variables essential for children’s well-being. Whether a parent is married or holds a prestigious job is not the litmus test for positive family influence on child outcomes. In isolation, these structural variables are not informative about the larger social environment in which the child is being raised or the nature of family process in the home. For example, it is known that there are many types of single-parent families and that children of divorced parents do not necessarily develop mental health problems.23
How children fare during and after divorce is a topic of considerable concern to pediatricians. During the 1990s, more than 1 million children were involved in divorce every year.24 In a meta-analysis of 67 studies conducted between 1990 and 1999, Amato25 found that children of divorced parents scored significantly lower than did children with married parents on measures related to academic achievement, conduct, psychological adjustment, self-concept, and social relations. These differences were less pronounced in African-American children than in white children.26 Marital discord appears to play an important role in how children are affected by parental divorce. Not only the presence or absence of discord but also how conflict unfolds during the dissolution of the marital relationship is important. When children have not been exposed to discord before the divorce, there are more long-term difficulties in adjustment, which suggests that there is an increase in conflict and stress after the divorce.25 In contrast, when there are relatively high levels of conflict before the divorce, dissolution of the marriage can actually be a relief for the child, and there are fewer long-term effects on child adjustment. Thus, what results in poor adjustment in children is not divorce per se but exposure to marital conflict. Experimental studies have also documented that children’s exposure to unresolved marital conflict, in particular, is more likely to result in emotional and behavioral disturbances than are marital disagreements that children witness as reaching some resolution.18
MULTIPLE RISK FACTORS AND POVERTY
Children growing up in poverty are disproportionately affected by chronic health conditions, including asthma, obesity, and diabetes. Children growing up in poverty also show early signs of allostatic load and higher resting blood pressure, which suggests that they are at increased risk for developing other serious chronic health conditions.27 In 2003, the poverty rate was highest for younger children; 20% of children between birth and the age of 5 years of age were being raised in households below the poverty line.28 There are concerns that children exposed to poverty over long periods may be at increased risks for poor physical and social-emotional outcomes. Limited economic resources can have crushing effects on family life, not only through its effects on the provision of basic needs but also by its effects on relationships and parenting. For example, in studies of rural farm families in Iowa, it was found that the downward turn of economic circumstances preceded marital distress and led to increases in hostile and coercive interactions between parents and adolescents.29 As noted previously, the compound effects of risk may influence child outcome; a similar picture holds true with regard to the effects of poverty on child health and well-being.
Evans30 considered the physical and mental health of children raised in poor rural communities and the multiple environmental risks they were exposed to, including crowding, noise, housing problems, family separation, family turmoil, violence, single-parent status, and parent education level. In accordance with the previous reports on multiple risk factors in less economically disadvantaged families, increasing numbers of risk factors were associated with more child psychological distress and feelings of less self-worth. Furthermore, children exposed to more environmental risk factors also evidenced higher systolic blood pressure and elevated neuroendocrine stress reactivity. As Evans stated, “As childhood exposure to cumulative risk increased, overall wear and tear on the body was elevated.” (p. 928).
Risk conditions are often compounded in nature and difficult to unravel. For example, the effects of family poverty on children’s health depend on how long the poverty lasts and the child’s age when the family is poor.31 Single-parent status also cannot be viewed in isolation, because the number of adults in the household has been identified as a marker of socioeconomic status known to be associated with some child outcomes.32 Perhaps one of the multiple-risk contexts that is most difficult to disentangle is that of the overlapping effects of economic conditions and ethnic background. In many empirically based studies of family effects on child development, poverty is confounded with minority status.33 One exception is a study employing the National Longitudinal Survey of Youth. Bradley and colleagues examined nearly 30,000 home observations of young children diverse in economic and ethnic backgrounds.34 Because of the relatively large sample size, the researchers were able to distinguish between poor and nonpoor European-American, African-American, and Hispanic-American families. In general, they found that poverty accounted for most, but not all, of the differences between the groups with regard to less stimulating home environments (availability of books, having parents read to the child, parent responsiveness). There were some differences, however, that were attributed to ethnic background when poverty status was controlled. For example, European-American mothers were more likely to display overt physical affection during the home observation than were African-American mothers. There were no ethnic group differences in the likelihood that mothers would talk to their infants or answer questions prompted by their elementary school–aged children. Thus, the distinguishing characteristics most often associated with poor outcomes for children, such as the lack of enriching home environments, were more closely associated with low income status than with ethnic background. Further efforts are warranted to separate the effects of poverty from the influence of ethnicity on child outcomes. The long-term effects of coping with discrimination may also affect parenting practices, particularly because these practices are evaluated by researchers within the dominant culture.35 In this regard, it is also important to be cognizant of factors, such as race and economic background of the observer, that can influence evaluations of family process. We return to this point when we discuss family assessment.
FAMILIES AS ORGANIZED SYSTEMS
This is not an unlikely scenario that on the surface appears fairly mundane but may include several elements of healthy family functioning. Families are charged with a host of tasks to insure the health and well-being of their children. Families are responsible for providing structure and care in at least six domains: (1) physical development and health; (2) emotional development and well-being; (3) social development; (4) cognitive development; (5) moral and spiritual development; and (6) cultural and aesthetic development.36 Each of these tasks can be considered as building on the other in a hierarchical manner; however, in day-to-day family life, they often overlap and are not clearly differentiated. In the example just provided, while the family is grabbing a quick breakfast before heading out the door for the day (and, it is hoped, fulfilling the nutritional needs of the children), they are also attending to their cultural and aesthetic development through the arrangement of after-school lessons. Families structure care and meet the developmental needs of their children through organized daily practices, as well as through beliefs that they carry about relationships. We now examine how daily practices, as reflected in family routines, and beliefs, as reflected in family narratives, are related to the health and well-being of developing children.
Family Routines and Healthy Development
In accordance with our focus on the multiply determined nature of child development, children’s health is also considered part of a larger system of family functioning. When we think about family health, we think about what the family, as a group, must do to maintain the well-being of all its members, including establishing waking and sleeping cycles, establishing eating habits, responding to acute illness, coping with chronic illness, preventing disease, and communicating with health professionals. These activities, or practices, are often folded into the family’s daily routines. Pediatricians are poignantly aware that for some chronic health conditions, family involvement in daily care is essential to good health but, at the same time, these management behaviors can be “tedious, repetitive, and invasive” (Fisher and Weihs,37 p. 562). This repetitive nature of management activities sets the stage for creating routines that provide predictability and order to family life. Conversely, the repetitive demands associated with good health care may also disrupt routines already in place and threaten family stability. We first define what we mean by family routines and then examine their relation to child health and well-being.
DEFINING ROUTINES
There is a personalized nature to family routines that makes it somewhat difficult to provide a standard definition. What may be a routine for one family may be absent in another. For example, some families hold very high expectations for when everyone is to be home for dinner and have set rules for the expression of emotional displays, whereas other families have a more laissez faire attitude toward mealtime attendance and rarely remark when someone makes an angry outburst at the table.38 Family routines tend to include some form of instrumental communication so that tasks get done, involve a momentary time commitment, and are repeated over time.39 In terms of normative development, family routines such as dinnertime, weekend activities, and annual celebrations (e.g., birthday celebrations) tend to become more organized and predictable after the early stages of parenting an infant and into preschool and elementary school years.40 The regularity of family routine events such as mealtimes have been found to be associated with reduced risk taking and good mental health in adolescents.41,42 The sense of belonging created during these gatherings has been found to be associated with self-esteem and relational well-being in adolescents and young adults.40,43
HABITS
Habits are repetitive behaviors that individuals perform, often without conscious thought. Behavioral habits are automatic and typically involve a restricted range of behaviors. For example, some children may have developed a habit of snacking while sitting in front of the television set after school. A routine, on the other hand, involves a sequence of steps that are highly ordered.44 For example, a child’s morning routine may include a sequence of having breakfast, brushing teeth, checking the contents of a backpack, and playing catch with the dog before going to school. Healthy (or unhealthy) habits are often embedded in routines. Being in the habit of eating a nutritionally balanced meal may rely, in part, on shopping and cooking routines. For the most part, habits are rarely thought about, and pediatricians must ask repeatedly about parents’ and children’s daily routines to gather accurate information about healthy and unhealthy habits. It is not sufficient to ask whether a child eats a healthy diet, but it may be important to consider whether the diet is offered as part of a regularly organized routine.
Organized family routines may be part of good nutritional habits. For example, parents’ report of the importance of family routines has been found to be associated with children’s milk intake and likelihood of taking vitamins in low-income rural families.45 During the preschool and early school years, if mealtime routines are rushed and interactions are marked by discouragements and conflict, then children are at greater risk for developing obesity.46,47 Furthermore, if mealtime routines are regularly accompanied by television viewing rather than conversation, children consume 5% more of their calories from pizza, salty snacks, and soda and 5% less of their energy intake from fruits, vegetables, and juices than children from families with little or no television use during mealtimes.48 Qualitative studies have noted that individual members can disrupt diabetes management by routinely eating late, regularly serving desserts, and making daily shopping trips to grocery stores that have few choices in the way of fresh fruits and vegetables.49 Grocery shopping routines may also be affected by larger ecologies as lower income neighborhoods are often noted for grocery stores that do not have a full array of fresh produce. Thus, family routines may contribute to children’s health through establishing good nutritional habits and providing regular rather than erratic opportunities to be fed.
ADHERENCE
Adherence to pediatric medical regimens is notoriously poor. According to most surveys, families fail to follow medical advice more than half the time.50 It is unlikely that all cases of medical nonadherence are caused by lack of knowledge or a failure to fully understand doctor’s orders.51 Patients often remark that they fail to follow prescribed orders not because they want to but because they just could not find the time or because other responsibilities got in the way. There is no question that family life is busy and there are multiple demands on everyone’s time. Whether it is juggling home and work, squeezing in one more extracurricular activity, or just trying to get everyone fed during the week, the addition of a medical regimen to family responsibilities can seem overwhelming. One way that some families can adapt to the challenges of medical management is through the organization of their daily routines.
Many treatment guidelines for chronic health conditions suggest folding disease management into daily routines. The management of pediatric asthma is one such condition. Current practice guidelines14 emphasize the importance of daily and regular monitoring of asthma symptoms and detailed action plans in the event of an attack. Many of the recommendations are framed as part of the family’s daily or weekly routines such as vacuuming the house once a week, monthly cleaning of duct systems, and daily monitoring of peak flows. Accordingly, asthma management becomes part of ongoing family life, and families who are more capable of the organization of family routines are expected to have more effective management strategies.
In a survey of 133 families with a child who had asthma, it was found that parents who identified regular routines associated with taking and filling prescriptions had children who took their medications on a more regular basis, both according to parents’ report and according to computerized readings taken on the children’s inhalers.52 Furthermore, when there were regular medication routines in the home, parents had less trouble reminding their children to take their medications, and overall their children rarely or never forgot to take their medications. Because nonadherence to pediatric regimens is quite high53 and parents find themselves in the role of perpetual nagger, the establishment of regular routines may be one way to alleviate distress and promote health in children with chronic conditions. Future research appears warranted in order to consider whether interventions aimed at structuring family routines may positively affect disease management and increase medical adherence.
PARENTAL COMPETENCE
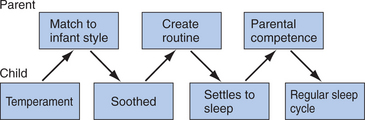
Family routines may also be important in promoting parental competence and establishing caregiving practices associated with children’s health and well-being. There is some evidence to suggest that experience with childcare routines before the birth of the first child is positively related to feelings of parental competence.54 However, in addition to parent skill set, the child contributes to these feelings, as was identified in the transactional model. Infant rhythmicity (e.g., regularity with which infants go to sleep at night) has been found to be associated with regularity of family routines, which, in turn, were associated with parental competence.55 The relation between caregiving competence and family routines during the early stages of parenting is probably the result of a series of transactions. When there is a good match between infant and parent behavioral style, it may be easier to engage the child in family routines. Routines become relatively stable, and the infant is easier to soothe, more amenable to scheduled naps, and less likely to wake in the night. This predictability, in turn, may reduce parental uncertainty and concern and increase feelings of competence. As parents engage in more rewarding daily caregiving activities, they become more confident in their abilities, and the routines themselves become more familiar and easier to carry out; for example, the difference between diapering an infant for the first versus the thousandth time is remarkable. The transactional process of one evolving caregiving routine is presented in Figure 5-3.
BELONGING VERSUS BURDEN
As the family practices its routines over time, individual members come to expect certain events to happen on a regular basis and form memories about these collective gatherings. For some, family is seen as a group that is a source of support, and repeat gatherings are eagerly anticipated. For others, family is seen as a group unworthy of trust, and collective gatherings are avoided. We have found that families who ascribe positive meaning to repeated routine gatherings such as dinnertime, weekends, and special celebrations feel more connected as a group and consider these events as special times rather than times to be endured.39 These feelings of belonging created during family routine gatherings are also associated with the health and well-being of children and adolescents. For example, children with chronic health conditions who report more connections during their family routines are less likely to report anxiety-related symptoms such as worry and somatic complaints.56 Furthermore, adolescents raised in caregiving environments with high-risk characteristics such as parental alcoholism are less likely to develop substance abuse problems and mental health problems when they report a sense of belonging created during family routines.57
In contrast to eagerly anticipating family events are feelings of being burdened and overwhelmed by the daily demands of family life. Feelings of burden can be particularly poignant in caring for a child with a chronic illness. Chronic illnesses can affect family life in notable ways, including added financial burden,58 and can place strains on marital relationships.59
Burden of care specifically associated with daily routine management may be related to quality of life for caregiver and child. In the previously mentioned study of 133 families with asthma, an element of daily care labeled routine burden was identified.52 Routine burden was defined as daily care seen as a chore with little emotional investment in caring for the child with the chronic illness. For both the caregiver and the child, when daily routines were considered more of a burden, quality of life was compromised. Caregivers reported that they were more emotionally bothered by their child’s health condition and their daily activities were affected more when there was more routine burden. Likewise, children reported that they were bothered more by their health symptoms, worried more, and were more frustrated by their health symptoms when their caregivers reported more routine burden. Routine burden was associated with functional disease severity, so that parents of children who required more care also believed that management was a chore. However, even when investigators controlled for disease severity, parents who perceived asthma care as a burden also reported poorer quality of life, as did their children.
CHAOS
It is possible to consider that the absence of routines is expressed as chaos. Chaotic home environments can be characterized by unpredictability, overcrowding, and noisy conditions.60 These types of conditions are more likely to exist in low-income environments and in neighborhoods perceived as dangerous and isolated. Research has indicated that the presence of chaos in the home, rather than poverty alone, mediates the effects of poverty on childhood psychological distress.61 Furthermore, children raised in chaotic environments have more difficulties reading social cues, and their parents use less effective discipline strategies.62 Thus, children exposed to chaotic environments lacking in predictable routines may also be exposed to other risks known to be associated with poor outcomes such as poverty, overcrowding, and dangerous neighborhoods. Again, we emphasize that family factors rarely, if ever, operate in isolation.
SUMMARY
One way to consider families as organized systems is to examine their daily practices. Families are faced with multiple challenges in keeping the group together; they must balance the needs of individuals who differ in age and personality, connect the family to institutions outside the home, and provide some regularity and predictability to daily life. At its most basic level, individuals create daily habits that become parts of the family’s routine practices. These routines are associated with family health in areas such as nutrition, establishment of wake and sleep cycles, and exercise. The establishment and maintenance of routines may enhance adherence to medical regimens. Families who have had experience generating such practices should be better equipped to fold disease management into their daily lives. We return to this point when we discuss models of family intervention useful for pediatricians. The repetition of family routines over time may lead to feelings of efficacy and competence, particularly for parents. Success in caregiving routines may reduce the stresses and uncertainties that accompany being a new parent, which, in turn, may affect children’s well-being in a transactional manner by increasing parents’ sense of personal efficacy. Parents who feel more efficacious are also more likely to interact in positive and sensitive ways that promote child well-being.63
When family routines are repeated over time and family gatherings are anticipated as welcomed events, individual members create memories that include a sense of belonging. This connectedness to the family, as a group, is associated with general health and relational well-being for adolescents and young adults and may reduce some of the mental health risks associated with chronic illness. The converse is also true: If the repetition of family routines over time results in feelings of dread and distance from the group, then there are concomitant effects on the health and well-being of child and parent.
Family Stories of Health and Well-Being
Family stories deal with how the family makes sense of its world, expresses rules of interaction, and creates beliefs about relationships.64 When family members are asked to talk about a personal experience, they must interpret what happened to them in a way that reflects how they work together (or do not), how they ascribe meaning to difficult and challenging situations, and how they relate to the social world. Pediatricians are quite familiar with family narratives, inasmuch as each patient visit presents an opportunity to listen to stories of health as well as illness.65
For families, stories are used to impart values and to socialize children into the mores of the culture. For example, the thematic content of family stories told to children has been found to differ according to whether they are told to girls or boys and whether they are told by mothers or fathers.66 This is important to pediatricians because mothers and fathers recount experiences of illnesses and trauma in different ways, as do boys and girls. For example, after treatment in the emergency department, mothers and daughters are more likely to recall details of the accident in a cohesive and integrated manner than are fathers or sons.67 Thus, pediatricians must consider the source of the narrative, not only the content.
Family stories intersect in the social-ecological model by reflecting cultural values and mores in such a way that the types of stories told differ across societies. For example, European-American and Chinese parents reminisce and tell stories about the past in different ways. European-American parents are more likely to focus on everyday events and to highlight practical problem solving, whereas Chinese parents are more likely to use stories to solve interpersonal conflicts and promote social harmony.68 The point is that the family environment is rich with narratives of personal experience that guide behavior and is influenced by larger social ecologies. We now discuss the key elements of family narratives that may be related to children’s health and well-being.
NARRATIVE COHERENCE
Coherence refers to how well an individual is able to construct and organize a story. Coherence is seen as an integration of different aspects of an experience that provides a sense of unity and purpose and is essential in constructing a personal life story.69 The elements of coherence include being able to tell a story that is succinct and yet including enough details to make it intelligible to the listener, having a logical flow, matching affect with content, and in some instances providing multiple perspectives.70 There has been increasing interest in using personal narratives, or stories, as a means to educate physicians, as well as to connect patients to physicians in the healing process.71,72 Stories that are coherent and well organized are likely to be better understood and easier to incorporate into a therapeutic context than are ones that are disjointed and lack a clear sense of order. The small but burgeoning literature discussed next links the study of family narratives, specifically that of coherence, and health and well-being.
If the coherence of family narratives is to be associated with child outcomes, it must be demonstrated that it varies systematically under high-risk conditions and that it is related to markers of family functioning. There is preliminary evidence that this is the case. Dickstein and colleagues found that parents with major affective disorders such as depression recount family experiences in a less coherent manner and that current depressive symptoms exacerbate this effect.73 There is also evidence to suggest that families who recount experiences associated with chronic illness less coherently also report poorer family functioning overall.74 Furthermore, when the narratives were less coherent, families had more difficulty engaging with the interviewer. Why might these findings be important for children and for pediatricians? First, consider their potential link to children’s outcomes.
There is a relatively strong empirical base linking coherence of narratives told about attachment relationships and the mental health and well-being of children, adolescents, and young adults.75,76 When parents and children are able to create coherent accounts of their caregiving relationships, they tend to be secure in their attachments and mentally healthy in the long run. A similar pattern is emerging in the case of family relationships. When individuals talk about family relationships in a coherent manner, family functioning appears to be more well regulated, providing a potentially more supportive environment for children. Why might these findings be important for pediatricians? During the course of a routine patient visit, families present a wealth of information, often in narrative, or story form. Families who have difficulties getting their points across to the pediatrician and creating a coherent account of personal events may be presenting similar images to their children. We have been particularly struck by the relation between coherence and family problem solving. Families who have difficulties engaging with interviewers and creating coherent accounts of chronic illness also express difficulties in family problem solving and communication.74 This combination may present added risks for children, who rely on their parents for clear and direct communication and effective problem solving. A cautionary note: This is a nascent line of research, and we also recognize that a transactional process is probably in place in which health care professionals probably influence the types and forms of information that families are willing to communicate.77 We also recognize that reliably detecting the relative coherence of a family narrative is beyond the reach of routine pediatric practice. Most systems for evaluating narrative coherence are fairly complex and involve lengthy training.78,79 Furthermore, it is not clear whether the stresses associated with a doctor’s visit may affect coherence in ways unrelated to psychological functioning.
RELATIONSHIP BELIEFS
Families create beliefs about relationships that vary along the dimension of trust, reliability, and safety.70 Relationships can be seen as sources of reward and worthy of trust or viewed as potential sources of harm and unreliable. Family narratives frequently depict the degree to which relationships are seen as something that can be mastered and rewarding or as overwhelming and confusing. In the case of the latter, statements are often made that reflect dissatisfaction and disappointment in relationships. Also, statements are made whereby relationships are seen as opportunities for experiencing appreciation and pleasure. As families are built around mutuality in relationships, the degree to which they are satisfactory and rewarding should bear concordance with children’s health and well-being.
Just as there are different conditions in which narrative coherence systematically varied, there are distinctions among family narratives about relationships in relation to children’s outcomes. Two types of outcomes are particularly pertinent for pediatricians: children’s behavior problems and health care utilization. There have been a few studies that have linked depictions of family relationships in stories to children’s behavior problems. Parents who recount family experiences as including rejecting and unrewarding relationships tend to have children with more problematic behaviors according to self-report measures.80 Furthermore, when parents tell stories that include depictions of family relationships that are unreliable and unsatisfactory, there are increased levels of negative affect when the family is gathered as a whole during routine mealtimes.73,80 Children’s stories of family experiences reflect a similar pattern. Children who have experienced abuse and neglect depict family relationships as less rewarding in stories about family events.81,82 Interestingly, children enrolled in an attachment-based therapeutic intervention changed their representations of family relationships, depicting caregivers as more trustworthy in the narratives after intervention than did children in the comparison group.82 Thus, the portrayal of relationships in family narratives reflects parents and children’s interpretation of the trustworthiness of others, which, in turn, may be related to social interaction and the regulation of behavior.75 There is also some evidence that narratives hold promise in understanding how families utilize health care services.
When asked to talk about the effects of an illness on daily life, family members typically have little trouble generating a story. However, there is no single way in which families meet the challenge of organizing their lives or responding to normative or nonnormative events, as already noted. The same holds true in considering how families recount strategies of care revealed in narratives. Families can rally around the care of an individual in a variety of ways.83 For some families, everyone is involved, and there is a team-based strategy so that multiple members of the family are “on the lookout” for the identified patient. This may mean being available to pick up prescriptions from the pharmacist, translating doctor’s orders into a native language, or reading a book out loud when a sibling does not feel well. For other families, there is one expert in the family who takes charge whenever someone is ill or whenever there is a chronic health condition. Sometimes this person takes on the role across generations, so that he or she is responsible for the care not only of offspring but also of older parents. In a third type of family management style, few roles are assigned, and there is little planning around emergencies and crises. Typically in these families, anxiety calls the family to action. These management strategies can be depicted in narratives and reflect beliefs about family relationships. In the first case, team-based strategies revolve around assumptions that family relationships are reliable and multiple members of the family can be called on at a moment’s notice. In the second case, relationships in general may be rewarding, but roles are assigned in such a way that there is a clear leader and authority in the family. In the third case, either relationships are seen as a bother and unreliable, or worry and anxiety predominate to the extent that relationships are precarious. When interviews about coping with a chronic illness were categorized by these management strategies, it was found that families that use either the family partnership or the expert-based approach were more likely to adhere to the prescribed medical regimen than were those who used more anxiety-based coping strategies.83 Furthermore, families that depicted their management strategies in the interviews as more reactive and relationships as less satisfactory were more likely to use the emergency room for care 1 year after the interview.
SUMMARY
Thus far, we have considered the family as an organized system that maintains itself as a group through organized routines and reaffirms its beliefs about the importance of relationships through accounts of personal experiences. These are family-level processes that come to form the family code. The family code is created to regulate child development, extending across generations, and involves the coordinated efforts of two or more people.17 Embedded within the family code are parent-child interaction patterns that can facilitate the smooth operation of daily life, as well as foster achievement of developmental tasks. We now briefly review some of the essential ingredients of family interaction that serve to support healthy development.
Family Interaction and Healthy Development
Family interaction can be evaluated along a variety of dimensions. Some of the more common domains are warmth, control, support, communication, problem solving, criticism, and affect.84 In this snippet of a mealtime observation, the family balances the need to maintain the group as a whole with expressions of independence. For most families, this balance is struck relatively effortlessly with good humor and warmth. A chorus of “Happy Birthday to You” to the grandmother, even in her absence, does not disrupt the flow of the meal, and individual desires are respected. In other families, however, expressions of autonomy may be met with harsh control, and negative affect predominates. Considerable effort has been directed toward identifying patterns of interaction associated with more optimal outcomes for children with chronic illness and children at risk for developing health problems.
Children with a chronic illness are at greater risk than children without a chronic illness for developing behavior problems or a psychiatric disorder, such as depression or anxiety. In fact, epidemiological surveys have revealed that children with a chronic illness are twice as likely to develop a diagnosable behavioral or psychiatric disorder.85 The causal mechanism for why children with a chronic illness are more at risk than their healthy counterparts is not known. Early speculations suggested that certain patterns of family interaction were more prevalent in families with a chronic illness and that these interaction patterns led to and sustained the disease state.86 On the basis primarily of clinical observations, the most common pattern was considered to consist of parental overinvolvement, overprotection, poor conflict resolution, and a primary focus on the child with the illness to the neglect of the marriage and other family members’ needs. This pattern has not been borne out in the empirical literature and fails to take into account the shifting nature of illness and its effect on family dynamics.87
Researchers have begun to examine how family interaction patterns may be part of a transactional process between characteristics of the child, health status, and caregiving. Researchers theorize that children may have a limited range of cognitive or emotional skills for coping with their disease or that the increase of environmental stressors, such as medication regimens and missed school days, may contribute to adjustment difficulties.88,89 The increase of disease-specific responsibilities places greater burden on the family as a whole, with the potential risk for increased conflict among family members and impaired levels of family functioning. A child may resent such conflict or family changes and externalize his or her resentment in the form of behavioral problems.89
Family conflict, observed either directly or through self-report, appears to disrupt effective disease management strategies and to adversely affect child health and well-being. Highly conflict-ridden family relationships can compromise communication, supervision, and division of responsibilities.90 It is likely that family conflict affects child outcomes through alterations in daily health practices, inasmuch as poor adherence to medical regimens has been found to be associated with family conflict.91,92 Furthermore, family conflict has been associated with poor glycemic control in children with diabetes.93 Family conflict may also be an indicator that the family as a group has not been able to adjust to the child’s illness, which in turn can lead to emotional distress for parent and child alike.94 Whereas the research linking family conflict and children’s health under chronic conditions appears to be mediated by disruptions in medical adherence, other investigators have examined how exposure to family conflict may result in compromised health by reducing children’s ability to respond to stress.
In summarizing the literature on high-risk family environments, Repetti and colleagues27 reported that family conflict is associated with higher rates of reported physical symptoms and lower attainment of developmentally expected weights and heights. They suggested that family conflict may lead to increased stress reactivity and allostatic load in children in high-risk environments. This argument is consistent with the research that we reviewed on multiple risk factor effects under poverty conditions. Indeed, the profile of extensive conflict, poor emotional and social support, and children’s heightened stress reactivity is consonant with the multidetermined model outlined previously. Thus, lower levels of family conflict may be one more element in the larger picture of family health.
Family conflict has received the most attention in the empirical literature perhaps because it is relatively easy to identify from video recordings. It may also be the case that negative interactions have a more toxic effect and that a modest amount of negativity can lead to poorer outcomes. According to family systems principles, there are other aspects of family interaction that should also contribute to healthy family functioning. These include direct and clear forms of communication, effective problem solving, responding to the emotional needs of others, showing genuine concern about the activities and interests of others, and supporting autonomy.95 To date, most researchers have reported on the overall general functioning of the family as it relates to child and family adjustment to such conditions as pediatric cancer,96 maternal depression,7 cystic fibrosis,97 and asthma.98 There is some evidence to suggest, however, that effective problem solving and direct forms of communication are associated with healthier outcomes for children with chronic illnesses. For example, adherence to dietary restrictions for children with cystic fibrosis is related to more positive forms of communication and problem solving observed directly during mealtime interactions and during structured laboratory interaction tasks.99,100 A similar pattern has been noted for families and children with diabetes.101,102
CULTURAL VARIATIONS IN FAMILY CONTEXT
Cultures, in general, are organized around a set of principles that guide individuals’ behavior in such a way that they are consistent with the mores of the larger society. Cultures vary in terms of the relative values given to individual strivings for autonomy and independence versus placing the needs of the group before the needs of the individual.103 In relation to these values of individualism and collectivism, there are variations in terms of deference to authority and what “counts” as a personal transgression. In some cultures, for example, a child is more likely to get into trouble or be disciplined for something that would cause shame to the family; in other cultures, punishment is doled out for not understanding how personal actions reflect flaws in an individual’s character.104 This point is important for pediatricians, because issues of discipline and parental control are embedded in both a cultural and a family context.
These values are transmitted, in part, through the organization of daily family life. The study of everyday tasks and situations is not only embedded in culture but is also at the very heart of how behavior is shaped by society.105,106 By focusing on how families in different cultures carry out daily routines such as household chores, investigators are able to get a glimpse at what is culturally relevant and how roles are assigned to facilitate socialization. Thus, we consider how the practice of family routines in different cultural contexts is related to children’s health and well-being.
When investigators consider cultural variations, they are also interested in situations in which there is a mismatch between the predominant society and families or between parents and children. A mismatch in values presents an added tension for individuals and family members, potentially compromising health and well-being. One such situation is a mismatch of values between generations during the process of immigration. A breakdown or deterioration of routines and rituals may indicate difficulties making the transition from one culture to another. Replacing old rituals with new ones, on the other hand, may also be an indication of adaptation to a new cultural environment. This is not an “either-or” process, inasmuch as current conceptualizations of the acculturation process suggest that there are family-level advantages to retaining connections to the country of origin, as well as incorporating aspects, such as language, of the newly adopted country into everyday practices.107,108
Recent census data document that 20% of children in the United States have immigrant parents and that 25% of children in low-income families are of immigrant status (www.census.gov). With immigration comes a blending of beliefs that regulates family interactions with health care professionals, as well as with each other. Therefore, we also consider briefly how cultural beliefs interface with family process and influence children’s health and well-being. It is beyond the scope of this chapter to cover the multitude of ways that culture and family processes transact to affect children’s development. Thus, we structure our discussion around three topics: family routine practices in Latino families, beliefs about autonomy in immigrant Chinese families, and disease management strategies in African American families. Although these may appear as disjointed topics, we have selected them to highlight how cultural values intersect with domains of family life that we have previously discussed.
Variations in Family Practices: Mealtime Routines in Latino Families
Here we see two approaches to feeding a toddler that may be rooted in cultural values of what is considered good conduct. Latino and Anglo individuals have been described as differing in the extent to which they hold values and meaning systems that are congruent with sociocentrism or individualism.109–111 Sociocentrism refers to an emphasis on the relationship between the individual and the group and subordination of ones personal interest to that of the group, resulting in a construction of the self as fundamentally linked to others. Latino cultures have typically been identified in the research literature as sociocentric.103 Within many Latino cultures, sociocentrism may be made evident through the importance placed on respect (respeto) and dignity (dignidad) in personal conduct. Both qualities are essential in the development of proper demeanor: knowing the level of decorum and courtesy that is required in a given situation.112 With regard to child rearing, this does not necessarily mean that Latino parents want their children to always do what is best for the group at the expense of their own happiness; rather, it is through genuine care and not malcriado (being poorly brought up) that a person can bring respect and happiness to the family and to himself or herself. Traditional Puerto Rican culture, for example, has been described as emphasizing interpersonal obligations, personal dignity, and respect for others.113 Puerto Rican mothers may believe that qualities such as malcriado and a lack of dignidad and respeto will give rise to a lack of acceptance from others in the community, which will reflect poorly on the family and the child, eventually leading to unhappiness for the child. In sum, the goal in traditional Latino cultures is to raise a child to become una persona de provecho—a person who is worthy of trust and is useful to the community.112
Harwood and Miller110 found that Anglo mothers were more likely than Puerto Rican mothers to stress the importance of an infant’s ability to cope autonomously with the stress of being left alone. In a series of studies, Harwood and Miller examined Anglo and Puerto Rican mothers’ preferences for behavior in their children. Puerto Rican mothers were more concerned about their children’s ability to maintain proper respect and dignity and were more likely to focus on their children’s ability to remain calm and good-natured, and to be physically close with their mothers, whereas Anglo mothers reported that they preferred infants who were able to manage autonomously.110 In a follow-up study, Harwood109 interviewed mothers about what they valued in children and found evidence that Anglo mothers placed greater importance on personal development and self-control. Harwood’s studies provide evidence for the existence of culturally defined values in the meanings that mothers may give to child behavior. Specifically, Anglo mothers placed more importance on personal competencies, and Puerto Rican mothers placed more importance on whether the infants were able to maintain proper demeanor and physical closeness.109
These beliefs and values may be expressed in the practice of mealtime routines. Latina (specifically Puerto Rican) mothers were less likely then Anglo mothers to encourage their children to feed themselves.111 In addition, the strategies that parents used to teach their children to feed themselves differed. Latina mothers were more likely to guide their children in getting food from the plate into the mouth and/or holding their children in their lap while they ate, rather than seat them in a high chair. Although these are relatively simple examples, they highlight how repetitive socialization practices are embedded in cultural values. How might pediatricians encounter the effects of these cultural practices and belief systems? One way is through the parents’ tolerance for and understanding of disruptive behaviors.
Families socialize their children in accordance with the values held by the culture as to what is acceptable and unacceptable behavior. As noted, in some Latino cultures, there are values held for self-control and personal demeanor that reflect the family’s stature. In interviews of Latina mothers whose children were seen by professionals for disruptive behaviors, three personality characteristics of the children were identified as salient: inteligente, malcriado, and de carácter fuerte.114 Children who were referred for disruptive behaviors by their teachers were seen as intelligent (inteligente) by their mothers, which suggests that misbehavior must be the result of giftedness or clever mischief. One half of the mothers interviewed mentioned their children’s bad manners (malcriado); however, of those who alluded to their children’s rude conduct, some did so as a means to disconfirm the trait and expressed concern that others would think of their child as spoiled. Mothers also described their children as possessing a willful temperament (de carácter fuerte). In contrast to malcriado, de carácter fuerte is seen as something that can be ultimately controlled, although not permanently altered. Together, this triad of characteristics provides the parents with an explanatory set of beliefs to account for disruptive behaviors that are inconsistent with the cultural values of good conduct.
Just as a cultural perspective may affect how misbehavior is understood, it can also affect how developmental milestones are interpreted. In consideration of whether a child is disabled or capable of performing the routine activities of daily living, it is also important to consider the degree to which the family and culture supports independence and autonomy. There may be significant cultural variations in the expected norms of activities of daily living for children with disabilities. For example, Latino parents, caregivers, teachers, and therapists expect children with disabilities to be dependent on their parents for many daily skills until much later than would be expected on tests with norms for white U.S. mainland residents.115 This pattern holds true for their nondisabled peers and is attributed to the interdependence between parents and children and cultural values of anonar (pampering or nurturing) and sobre protective (overprotectiveness). Thus, parents may report the achievement of developmental milestones at a rate that would be cause for concern by the pediatrician and yet are within a range considered normative in a given culture.
Immigration and the Balance of Family Obligations
The unanswered question to this scenario is whether Susan is relatively happy or distressed by not spending time with her peers. For native-born American teenagers, spending time with peers is considered part of the natural progression of moving out of the home and becoming more autonomous. For some adolescents of immigrant families, however, staying close to home is considered part of being a good son or daughter. Whether this causes distress may depend on the relationship between parent and adolescent and beliefs that the adolescent holds about family obligations. Chinese adolescents report, on average, two family obligation activities per day and spend slightly more than one hour each day assisting and being with their families.116 Overall, girls spend more time and carry out more family obligations than do boys. Socializing with peers is negatively related to family obligations on any given day. However, the amount of time spent in family obligations does not necessarily lead to greater conflict or personal distress for these adolescents. These youths appear to expect to balance family and social obligations and make deliberate decisions to spend time with their families. Rather than leading to a sense of alienation from peers, these daily practices may reinforce cultural beliefs and provide a sense of identity. “Family obligations may provide the children from immigrant families with a sense of identity and purpose in an American society that, at times, has been accused of emphasizing individualism at the cost of heightened adolescent alienation” (Fuligini et al,116 p. 311). Thus, obligation to the family is balanced with spending time with peers and does not necessarily create personal distress. Yet to be answered, however, is whether this balanced perspective weakens with subsequent generations as extended engagement with popular culture may create increased opportunities to weigh obligations to peers over those to parents.
Ethnic Variations in Family Management Practices
A first step in considering how parents transfer responsibility of management practices is to identify beliefs that the family may hold about the condition that may act as a barrier to good health. In interviews with African-American parents of children with asthma, it was found that a more holistic approach to managing asthma that included both the child’s mental and physical well-being was desirable.117 Many parents reported that they modified the physician’s treatment plan to include nonmedicinal alternatives for their children’s symptoms and held strong personal beliefs against the use of medications. Thus, when it is time to transfer the responsibility of disease management to children, clinicians must consider how beliefs about medication are also being parlayed.
An additional point to consider is that transfer of responsibility may not necessarily be from one caregiver to the child, inasmuch as two or more caregivers are frequently involved in disease management in urban and African-American families.118 Having multiple family members involved in asthma care extends into the patient’s adolescent years.119 Multiple family members and extended kin networks can serve as sources of support. It is also important, however, to carefully consider whether availability of support translates into clear assignment of responsibility. In interviews with adolescents and their parents, Walders and colleagues found that African-American parents overestimated the amount of responsibility that adolescents were taking for their asthma care.119 As the authors pointed out, the wide array of family structures can be simultaneously a source of support and a source of confusion when it comes to assigning responsibility. Pediatricians are in the unique position to address transfer of responsibility with their patients over time while being sensitive to how variations in family structure and cultural beliefs may regulate this process.
Summary
Although there is little disagreement that changes in population demographics mandates broader conceptualizations of cultural influences on health,120 the empirical base linking cultural variations in family practices and children’s health is somewhat limited. There is a growing literature that documents cultural and ethnic variations in family routines and beliefs associated with child outcomes. It is important to emphasize that there is considerable heterogeneity within a given culture and that we have made only generalizations. Furthermore, the effects of economic stability and resources on immigration cannot be ignored and in all likelihood play a significant role in the understanding of how cultural variations in family context contribute to children’s health.121,122
FAMILY-BASED INTERVENTIONS
It is beyond the scope of this chapter to provide a comprehensive review of all the intervention programs available to families. The interested reader is referred to reviews and collected volumes for more thorough discussions of the topic.123–127 There is growing empirical evidence that targeting the whole family as a method of treatment for disease-specific issues is effective. For example, in intervention studies aimed at improving disease management in insulin-dependent diabetes, families who participated in Behavioral Family Systems Therapy, in comparison with families who received educational forms of intervention, showed higher rates of improvement in parent-adolescent relations and lower rates of diabetes-specific conflict.128 In a review of interventions for survivors of childhood cancer and their families, Kazak and associates129 summarized empirical evidence for interventions from four categories specific to pediatric oncology: understanding procedural pain, realizing long-term consequences, appreciating distress at diagnosis and over time, and recognizing the importance of social relationships. Kazak and associates pointed to the importance of developing interventions that target families on the basis of a particular set of risk factors, of designing more empirical interventions for families experiencing disease relapse, and of striving to develop interventions that are effective for ethnically diverse families. Current thinking in family-based interventions for pediatric conditions is that a one-size-fits-all strategy is unlikely to be effective.130 Because families are developmentally complex systems that routinely undergo change, as we have outlined, it is unreasonable to expect that a uniform strategy aimed at altering family level behaviors would be advantageous across all families and all situations. Thus, in this section, we consider several approaches that may be appropriate for families at a given time. We place these strategies in the transactional model previously discussed. Using a decision tree, we outline different strategies that can be implemented by drawing on the existing strengths and resources of the family and tied into previously established forms of intervention such as interaction guidance, behavior management, and relationship building techniques.
Transactional Model of Intervention
In this scenario, we see a transaction unfolding in which the child’s symptoms have disrupted the daily routines of family life. According to the principles of the transactional model, behavior can change at multiple points, whereby the child’s condition affects the organization of the family and the family’s behavior affects the well-being of the child. Interventions that capitalize on the strengths of the system at a given time and minimize the need to alter the system as a whole—a timely and expensive endeavor—can be targeted. Sameroff131 proposed that there are at least three categories of intervention that can be implemented to effect change in either the child or parent: remediation, redefinition, and reeducation. Remediation efforts are aimed at changing the way the child behaves toward the parent. For example, providing Louisa with a controller medication should reduce her symptoms, which, in turn, should reduce her mother’s worry about her condition. Redefinition changes the way the parent interprets the child’s behavior. In Louisa’s case, interventions aimed at helping her family understand her respiratory symptoms as part of a chronic illness rather than a recurring cold may change the ways in which they respond to her symptoms. Reeducation efforts are aimed at changing the way the parent acts with the child through increased knowledge. In the case of Louisa, education efforts aimed at following an action plan and reducing exposure to environmental toxins would reduce Louisa’s symptoms. To these three Rs of intervention, Fiese and Wamboldt132 added a fourth type of intervention often warranted in health care settings: realignment. Realignment is called for when family members disagree about a course of action and daily practices have been disrupted to the extent that the health and well-being of the child are compromised. In Louisa’s case, if the parents disagreed on her diagnosis of asthma, then there would be serious consequences as to whether they would agree on a plan of action if she had another asthma attack. These four Rs of intervention are now examined in the framework of family routines and a clinical decision-making process that is accessible to pediatricians.
CLINICAL DECISION MAKING APPLIED TO MEDICAL ADHERENCE
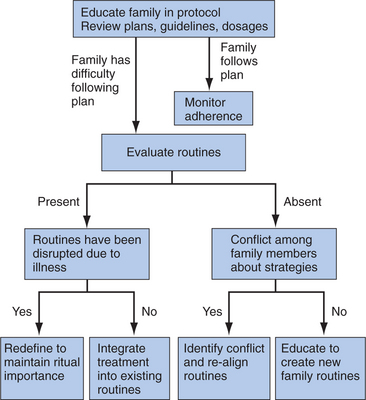
We have already discussed the roles that family routines and daily practices may play in the health and well-being of children. We now incorporate these practices into the clinical decision-making process as a guide for pediatricians when working with families who are expected to follow a daily treatment protocol to maintain the health and well-being of their children. We chart this process as part of a decision tree, although we also recognize that there are instances in which family circumstances warrant more than one type of intervention (Fig. 5-4).
The second alternative in evaluating routines is cases in which families do not have routines in place. In these situations, it is important to consider whether there is conflict among family members about strategies for implementing treatment recommendations. As previously noted, conflict can have a detrimental effect on children’s health. Family members can also disagree about the relative value of particular disease management routines and the relative importance of attending to specific aspects of an individual’s prescribed protocol. We noted, for example, in families with a diabetic member that routinely eating late or serving sweet desserts can counteract the individual’s good intentions. It is important to identify the source of conflict around implementing the routine. Sometimes these conflicts can be rooted in myths and misperceptions about the prescribed protocol: for example, not wanting to take daily prescribed medications for fear that the child will become “hooked on other drugs.” There are other instances in which there are disagreements that are rooted in marital conflicts. Under these circumstances, it is important to separate marital conflict and discord from managing daily routines. This is particularly germane in the case of divorced and separated families in which children are living in two households and there may be two sets of rules and routines. It is important to come to an agreement about consistency in routines (e.g., bedtime, mealtime, medication use) so that the child is protected from the harmful effects of conflictive households.
There are also developmental characteristics to take into consideration in evaluating family conflict about routines. Adolescence is a time of transition for the entire family. For adolescents with a chronic health condition, this is a time when responsibility of disease management is transferred from the parent to the adolescent. This is a prime opportunity to identify healthy routines that can be under the adolescent’s control. Indeed, astute clinicians have taken this transfer-of-responsibility notion as a central aspect of family-based interventions with adolescents. Anderson and her colleagues developed a brief intervention aimed at reducing conflict between adolescents and their parents over diabetes management.133 Pediatricians may find it useful to discuss transfer of responsibility with adolescents and their parents in the context of other transitions that are occurring in the routine life of the family, such as curfews, after-school activities, and part-time employment.
The last form of routine intervention is reeducation. This type of intervention is called for when the family has been provided the basic information about the treatment protocol, there is an absence of conflict about how to carry out the protocol, but there is no previous experience in creating or sustaining regular routines. This type of intervention may be the most challenging to implement and maintain. For these families, it is important to first identify the physical settings in which the routines can occur and the time at which they can occur and then apply principles of parent management training.134 Although there is a long tradition in implementing home-based interventions,135 we want to emphasize the sensitive nature of creating family routines where there were previously none. The question that needs to be addressed concerns what led to the impoverishment of family routines. For some families, a history of abuse and neglect provides little in the way of comfort when members are gathered together as a group. For other families, a chaotic home environment may have been the result of parental psychopathology and unstable economic resources, which led to unpredictable daily patterns of caregiving. Again, we highlight that family life is determined by multiple factors and that the presence or absence of family routines is likewise determined. We present these four forms of intervention as a heuristic for the busy pediatrician. Future research efforts are warranted to determine whether this approach to clinical decision making and the concomitant interventions qualify as empirically supported forms of intervention. However, the four Rs of intervention are theoretically grounded and based on preexisting forms of intervention that have been proved effective in other domains such as home-based educational interventions.135 What is unique to this format is a systematic consideration of family-level functioning in determining which form of intervention may be more appropriate at a given time.
We have used adherence to medical regimens as an example for this decision-making process and implementing routine-based interventions. Home- and routine-based interventions are also used frequently to address problem behaviors in children with developmental disabilities. Folding an intervention into everyday family household practices such as mealtime, playtime, and bedtime may be positively viewed by family members because they are less likely to be viewed as “one more thing” to be added on to an already busy day and may thus promote stronger family investment in the treatment protocol.136 Interventions such as positive behavioral support137 and routine-based intervention138 are examples of programs that encourage families to identify specific daily routines as settings for behavioral interventions. These interventions enlist parents as the therapist and are tailored to fit the rhythms of a particular family. Results from these programs are promising in reducing problematic and disruptive child behaviors and are positively viewed by parents.
Family-Based Coping Interventions
The transactional model of interventions is useful for identifying points of entry to effect change with the aim to get the child and family back on track toward healthy development. There are other instances, however, in which the family may require assistance in coping with traumatic events and warrant interventions aimed not so much at changing the family’s routines as at addressing the family’s belief systems. One area that has received some attention in this regard is aiding families in coping with childhood cancer.
Most survivors of childhood cancer and their families do well after treatment; however there is a significant proportion of adolescents and their parents who report reexperiencing aspects of the illness that can be considered traumatic and stressful.139 To address these symptoms, a family-based treatment program has been developed to assist adolescents and their families in coping with surviving cancer.140,141 Families participate in a day-long discussion with other families who have been similarly affected by childhood cancer. The group discussion focuses on beliefs that survivors and their family members have about cancer with the ultimate aims of reducing stress and altering misperceptions. Findings from these interventions suggest that the intervention is successful in reducing adolescents’ symptoms of posttraumatic stress and that there are positive benefits to family members. Although there is some evidence that the most stressed of family members may not be willing to participate in an all-day discussion format, Kazak and associates developed video formats that may be more accessible and show promising results in relieving stress in families with newly diagnosed cancer.129
Other examples of brief family-based interventions include targeting how parents and children interact with each other to promote better outcomes. As previously noted, family conflict can have detrimental effects on a variety of child health and behavioral outcomes. Some of these family-based interventions focus specifically on increasing positive forms of social interaction such as responsiveness, sensitivity, and warmth.142,143 These interventions are often employed with families with young infants and toddlers, who are at risk for developing developmental and behavioral problems as a result of birth complications or environmental stress.
Other family-based interventions also attend to interaction patterns as part of the larger multisystemic influences on child and adolescent health. Most notably, Henggeler developed a multisystemic therapy model that includes an intensive home-based family therapy component to improve adherence to diabetic regimens.144 Therapists’ focuses include improving problem-solving skills, reducing conflict, and identifying monitoring strategies. Although labor intensive, this form of intervention has been shown effective in reducing health care costs.145
Summary
In view of the complexity of family effects on child development, family-based interventions are likewise multifaceted. Too often, when considering how best to assist families in distress, clinicians become overwhelmed with the complexity of the situation and are left with little guidance as to how to begin addressing the problem. We have provided a set of decision rules that may assist pediatricians in working their way through the web of family influence on changing child behavior. It is unlikely that all forms of effective family-based interventions will fit neatly into a managed care environment or conform to common notions of what constitutes psychological interventions. Because families are composed of different numbers of members, who play different roles and are changing with time, it is unreasonable to expect that a one-size-fits-all approach to helping families will be effective.130 In some cases, interventions must be implemented in the family’s home at a time that is convenient for the family. In other cases, a videotape of other family members’ experience with a particular condition may be as effective as gathering together a support group. In other instances, pediatricians and psychologists may need to work directly with a family who has been unresponsive to other forms of intervention.146 Pediatricians are often in the position to refer families for evaluations conducted by social workers, psychologists, and psychiatrists. Although it is beyond the scope of this chapter to provide a comprehensive review of how families are likely to be assessed by these professionals, we provide a brief overview of some of the more commonly used instruments to familiarize the busy practitioner.
FAMILY ASSESSMENT
Direct Observation
Skilled family clinicians make use of the power of observation to detect problematic patterns of interaction. Oftentimes aligned with different schools of family therapy, observation of how the family interacts as a group informs the clinician about such factors as balance of power in the family, expression of rules, gender roles, and tolerance for autonomy.147 In clinical settings, these observations are usually conducted in conjunction with a family interview. In research settings, semistructured tasks are frequently used. A common strategy is to use a “revealed differences” task with couples or parent and child. In these instances, the individuals independently complete a questionnaire or checklist about family life. The researcher identifies one or two points over which the individuals disagree the most and then reveals the differences and ask the dyad to come to some resolution within a given period of time. The rationale behind such a task is that, by forcing the dyad to discuss an area of disagreement, the observer can detect problem solving and conflict resolution skills. An alternative to this approach is to select issues identified by the family as conflictive and instruct them to discuss the issue for 10 minutes.148 Direct observation of whole family functioning has also been applied to group interactions such as mealtimes. The McMaster Mealtime Interaction Coding System149 was devised to capture how family members interact during a routine mealtime. It includes seven scales (task accomplishment, communication, affect management, interpersonal involvement, behavior control, roles, and overall family functioning) that have been found to distinguish families who are functioning well from those who evidence problems in a variety of conditions, including parental psychiatric disturbances,7 cystic fibrosis,100 and asthma.150 These coding systems are valuable research tools that allow for a careful examination of the types of family behaviors that are associated with more optimal functioning for children being raised under a variety of risk conditions. However, because of the dependence on video recordings and time involved in learning how to use these systems, they are unwieldy for pediatric practice. Another cautionary note is warranted because family interaction patterns may vary systematically by ethnic background.9,35 Thus, it is important to consider the cultural context in which the observations are being conducted and in which the observers are operating.
Structured Interviews
Structured family interviews are used primarily for diagnostic purposes and typically last 1 to several hours. The McMaster Structured Interview of Family Functioning95 focuses on six domains of family functioning: problem solving, communication, roles, affective responsiveness, affective involvement, and behavior control. Family members are asked to respond to a series of questions about daily life, such as how they solve problems around finances, leisure time, and relationships with in-laws. The interviews are rated along the McMaster Clinical Rating Scale,95 in which a clinical cutoff score is used to distinguish families who are considered healthy from those experiencing psychological distress. The McMaster Clinical Rating Scale has proved reliable in distinguishing parents with a psychiatric disorder from those not currently experiencing symptoms7 and useful in assessing relative strengths in families who have a child who has experienced traumatic brain injury.151
Disease-specific interviews have also been developed. The Diabetes Social Support Interview152 assesses children’s perceived support from family and friends as it pertains specifically to diabetes care. Children are asked about how much help they receive from their family in such areas as insulin shots, as well as emotional support. Interrater reliability is reported to be acceptable,153 and interview scores have been found to be related to concurrent disease states.152 These types of interviews may be useful for pediatricians in assessing the degree to which family members support children’s disease management activities.
Self-Report Questionnaires
Although it is unlikely that the busy pediatrician will have time to administer lengthy questionnaires to family members, there are some questionnaires that can be adapted for use in daily practice. The Family Adaptation, Partnership Growth, Affection, and Resolve Scale (Family APGAR)154 is a brief five-item questionnaire that identifies a family member’s level of satisfaction with family functioning. Examples of items include “I am satisfied that I can turn to my family for help when something is troubling me” and “I am satisfied with the way my family and I share time together.” The Family APGAR has been found to have reasonable content validity and adequate test-retest reliability and useful in primary care settings.155 Although the Family APGAR is not a direct measure of family functioning, its results indicate how satisfied the individual is with the way the family is working.156
The McMaster Family Assessment Device (FAD)157 is a 60-item self-report questionnaire administered to adults. The FAD includes six subscales: Problem Solving, Communication, Roles, Affective Responsiveness, Affective Involvement, and Behavior Control. A General Functioning Score may also be derived. Test-retest reliability over a 1-week period ranged from 0.66 to 0.76. The FAD has been found to distinguish between clinical and nonclinical groups and is not related to measures of social desirability. Specifically for children, elevated scores (indicating poorer functioning) on the FAD have been associated with medication nonadherence in cases of asthma.91 Higher FAD scores were also found in children with recurrent abdominal pain and with frequent headaches than in a healthy control group of children.158
We have highlighted a few of the more commonly used family assessment techniques. Our listing is not in any way exhaustive. However, it should provide the pediatrician with a flavor of what types of assessment are available when the pediatrician makes a referral or considers a more extensive evaluation of a particular family.
FUTURE DIRECTIONS IN FAMILY RESEARCH AND INTERVENTIONS
There has been a growing appreciation for the pivotal role that families play in the health and well-being of their children. Although this appreciation is somewhat intuitive, methodological and clinical interventions have not kept pace with theoretical advances. We have outlined some of the reasons for the relatively slow pace in advancing family research, including but not limited to the complexity of family systems, the multiply determined nature of risk, and the cultural influences on individual development. Future efforts are warranted to take this complexity into consideration when researchers tackle the thorny issues of how families come to affect children’s development. This will call for a sophisticated research agenda that cuts across traditional disciplinary lines and incorporates multiple levels of analysis. The authors of the white paper report on early childhood development, From Neurons to Neighborhoods, persuasively argued that development can be understood only through an integration of knowledge gleaned from the behavioral, brain, social, economic, and political sciences.159 A similar effort is warranted when investigators consider future directions in understanding the role that families play in promoting children’s health. This will call for multiple levels of analysis, including the effects of physiology on social interactions and the manner in which family beliefs may alter disease status, for example. Multiple levels of analysis calls for strategies in which researchers consider variability within families across different classes of variables (e.g., physiology, mental health, physical health symptoms, cognitive functioning, family process), as well as variability across time.160 For example, future efforts may be directed at asking questions such as how changes in the physical health of the child affect family beliefs about their own ability to change daily health habits. The shifting cultural landscape of contemporary families mandate sensitivity to variability rooted in traditions and beliefs that may extend across generations and geographic boundaries. Likewise, family-based interventions must also take into account family-level variability, including but not limited to availability of economic resources, ages of children, and ethnic background. These parameters are not just census markers but may be important moderators and mediators of treatment effectiveness. A family strength-based resilience approach may provide pediatricians with the opportunity to identify which family-level factors are more likely to promote adjustment and reduce risk in their patients.161 In this regard, interventions are aimed at restoring overall family health, not just addressing symptoms in the individual patient. The challenge for pediatricians is to effectively identify strategies and modalities that will fit for a particular family within a given developmental period. These decisions do not operate in a vacuum; they are also affected by the policies that are in place that support child and family health. We close with a brief note about public policy in the interest of child and family health.
CHILD AND FAMILY HEALTH: POLICY PRIORITIES
Clearly, it is beyond the charge or scope of this chapter to address how public policy affects children’s health. However, we firmly believe that families make significant contributions to the health and well-being of children and that public policy should support and not get in the way of the best intentions of parents. Addressing policy issues is necessarily a question of costs, benefits, and how to effect change for the common good.162 How might our understanding of the multifaceted role of the family inform public policy? First, there are many types of family structures, and family form does not dictate child health and well-being. Thus, policies that favor one family structure over another will probably not benefit children in any appreciable way and will probably harm a significant portion of children. Second, families need time to be together in order to foster more optimal outcomes for their children. It not desirable to implement heavy-handed policies that dictate the amount of time families should spend together. Again, we emphasize the personal nature of family time. However, when inflexible work policies make it difficult for families to adjust to the needs of their children, their children’s health is often compromised. Parents often have to make the difficult choice between staying home with an ill child and going to work. These are not decisions that are in the best interest of the family. Third, the maintenance of children’s health is more than just having access to care: It is also the family’s ability to garner resources for transportation and following medical advice. Better support in terms of education, transportation, and support aimed at the entire family will probably reduce health care costs in the cases of chronic childhood illnesses.
Families are remarkably resilient. They are faced with multiple challenges every day, such as organizing daily life, making sure the emotional needs of each member are met, keeping conflict in check, and doing so within the boundaries of cultural mores. When a family walks into a pediatrician’s office, the members bring a set of beliefs and catalog of practices that will influence how they respond to the simple question “How are you feeling today?” We hope that this brief tour of the family context of child health and well-being provides the pediatrician with an appreciation of how densely packed the answer to this question may be.
1 Heaton TB, Forste R, Hoffman JP, et al. Cross-national variation in family influences in child health. Social Science Med. 2005;60:97-108.
2 Chen E, Bloomberg GR, Fisher EB, et al. Predictors of repeat hospitalization in children with asthma: The role of psychosocial and socioenvironmental factors. Health Psychol. 2003;22:12-18.
3 Kazak AE, Barakat LP, Meeske K, et al. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol. 1997;65:120-129.
4 Case A, Lubotsky D, Paxson C. Economic status and health in childhood: The origins of the gradient. Am Econ Rev. 2002;92:1308-1334.
5 Furstenberg FF, Cook TD, Eccles J, et al. Managing to Make It: Urban Families and Adolescent Success. Chicago: University of Chicago Press, 1999.
6 Cowan PA, Cohn DA, Cowan CP, et al. Parents’ attachment histories and children’s externalizing and internalizing behaviors: Exploring family systems models of linkages. J Consult Clin Psychol. 1996;64:53-63.
7 Dickstein S, Seifer R, Hayden LC, et al. Levels of family assessment: II. Impact of maternal psychopathology on family functioning. J Fam Psychol. 1998;12:23-40.
8 Main M, Goldwyn R. Predicting rejection of her infant from mother’s representation of her own experience: Implications for the abused-abusing inter-generational cycle. Child Abuse Negl. 1984;8:203-217.
9 Gonzales NA, Cauce AM, Mason CA. Interobserver agreement in the assessment of parental behavior and parent-adolescent conflict: African A merican mothers, daughters, and independent observers. Child Dev. 1996;67:1483-1498.
10 Teachman JD, Tedrow LM, Crowder KD. The changing demography of America’s families. J Marriage Fam. 2000;62:1234-1246.
11 Schor EL. American Academy of Pediatrics Task Force on the Family: Family pediatrics: Report of the Task Force on the Family. Pediatrics. 2003;111(suppl):1541-1571.
12 Lidz T, Cornelison A, Fleck S, et al. The intrafamilial environment of schizophrenic patients: II. Marital schism and marital skew. Am J Psychiatry. 1957;114:241-248.
13 Purcell K, Brady K, Chai H, et al. The effect on asthma in children of experimental separation from the family. Psychosom Med. 1969;31:144-164.
14 National Institutes of Health. Guidelines for the Diagnosis and Management of Asthma (NIH Publication No. 97–4051). Washington, DC: National Institutes of Health, 1997.
15 Bronfenbrenner U. The Ecology of Human Development. Cambridge, MA: Harvard University Press, 1979.
16 Sameroff AJ, Chandler MJ. Reproductive risk and the continuum of caretaking causality. Horowitz FD, Hetherington M, Scarr-Salapetek S, et al, editors. Review of Child Development Research. Chicago: Chicago University Press; 1975;4:187-244.
17 Sameroff AJ, Fiese BH. Transactional regulation: The developmental ecology of early intervention. In: Meisels SJ, Shonkoff JP, editors. Early Intervention: A Handbook of Theory, Practice, and Analysis. New York: Cambridge University Press; 2000:3-19.
18 Cummings EM, Davies PT, Campbell SB. Developmental Psychopathology and Family Process. New York: Guilford, 2000.
19 Kazak AE, Rourke MT, Crump TA. Families and other systems in pediatric psychology. In: Roberts MC, editor. Handbook of Pediatric Psychology. New York: Guilford; 2003:159-175.
20 Marks LD, Dollahite DC. Religion, relationships, and responsible fathering in Latter-Day Saint families of children with special needs. J Soc Pers Relat. 2001;18:625-650.
21 Brooks-Gunn J, Klebanov P, Liaw F, et al. Enhancing the development of low birth weight, premature infants: Changes in cognition and behavior over the first three years. Child Dev. 1993;64:736-753.
22 Sameroff AJ. General systems theories and developmental psychopathology. Cicchetti D, Cohen D, editors. Handbook of Developmental Psychopathology. New York: Wiley; 1995;1:659-695.
23 Hetherington EM, Kelly J. For Better or for Worse: Divorce Reconsidered. New York: Norton, 2002.
24 U.S. Bureau of the Census. Statistical Abstract of the United States 1999. Washington, DC: U.S. Government Printing Office, 1999.
25 Amato PR. Children of divorce in the 1990s: An update of the Amato and Keith (1991) meta-analysis. J Fam Psychol. 2001;15:355-370.
26 Hetherington EM, Stanley-Hagan M. The adjustment of children with divorced parents: A risk and resiliency perspective. J Child Psychol Psychiatry. 1999;40:129-140.
27 Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128:330-366.
28 U.S. Bureau of the Census. Current Population Survey, 1981 to 2004 Annual Social and Economic Supplements. Washington, DC: U.S. Government Printing Office, 2004.
29 Conger RD, Ge X, Elder GH, et al. Economic stress, coercive family process, and developmental problems of adolescents. Child Dev. 1994;65:541-561.
30 Evans GW. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol. 2003;39:924-933.
31 Duncan GJ, Brooks-Gunn J. Consequences of Growing up Poor. New York: Russell Sage Foundation, 1997.
32 Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371-399.
33 Huston AC, McLoyd VC, Garcia Coll C. Children and poverty: Issues in contemporary research. Child Dev. 1994;65:275-282.
34 Bradley RH, Corwyn RF, McAdoo HP, et al. The home environments of children in the United States part I: Variations by age, ethnicity, and poverty status. Child Dev. 2001;72:1844-1867.
35 McAdoo HP. Ethnic Families: Strength in Diversity. Newbury Park, CA: Sage Publications, 1993.
36 Landesman S, Jaccard J, Gunderson V. The family environment: The combined influence of family behavior, goals, strategies, resources, and individual experiences. In: Lewis M, Feinman S, editors. Social Influences and Socialization in Infancy. New York: Plenum Press; 1991:63-96.
37 Fisher L, Weihs KL. Can addressing family relationships improve outcomes in chronic disease? J Fam Pract. 2000;49:561-566.
38 Fiese BH, Foley KP, Spagnola M: Routine and ritual elements in family mealtimes: Contexts for child well-being and family identity. New Dir Child Adolesc Dev Spring. (111): 67-89.
39 Fiese BH, Tomcho T, Douglas M, et al. Fifty years of research on naturally occurring rituals: Cause for celebration? J Fam Psychol. 2002;16:381-390.
40 Fiese BH, Hooker KA, Kotary L, et al. Family rituals in the early stages of parenthood. J Marriage Fam. 1993;57:633-642.
41 Compan E, Moreno J, Ruiz MT, et al. Doing things together: Adolescent health and family rituals. J Epidemiol Community Health. 2002;56:89-94.
42 Eisenberg ME, Olson RE, Neumark-Sztainer D, et al. Correlations between family meals and psychosocial well-being among adolescents. Arch Pediatr Adolesc Med. 2004;158:792-796.
43 Fiese BH. Dimensions of family rituals across two generations: Relation to adolescent identity. Fam Process. 1992;31:151-162.
44 Clark FA. The concept of habit and routine: A preliminary theoretical synthesis. Occup Ther J Res. 2000;20:123S-137S.
45 Lee EJ, Murry VM, Brody G, et al. Maternal resources, parenting, and dietary patterns among rural African American children in single-parent families. Public Health Nurs. 2002;19:104-111.
46 Drucker RR, Hammer LD, Agras WS, et al. Can mothers influence their child’s eating behavior? Dev Behav Pediatr. 1999;20:88-92.
47 Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653-661.
48 Coon KA, Goldberg J, Rogers BL, et al. Relationships between use of television during meals and children’s food consumption patterns. Pediatrics. 2001;107(1):E7.
49 Gerstle JF, Varenne H, Contento I. Post-diagnosis family adaptation influences glycemic control in women with type 2 diabetes mellitus. J Am Diet Assoc. 2001;101:918-922.
50 Rapoff MA. Adherence to Pediatric Medical Regimens. New York: Kluwer Academic, 1999.
51 Drotar D. Promoting Adherence to Medical Treatment in Childhood Chronic Illness: Concepts, Methods, and Interventions. Mahwah, NJ: Erlbaum, 2000.
52 Fiese BH, Wamboldt FS, Anbar RD. Family asthma management routines: Connections to medical adherence and quality of life. J Pediatr. 2005;146:171-176.
53 Bender B, Milgrom H, Rand C. Nonadherence in asthmatic patients: Is there a solution to the problem? Ann Allergy Asthma Immunol. 1997;79:177-186.
54 Porter CL, Hsu H. First-time mothers’ perceptions of efficacy during the transition to motherhood: Links to infant temperament. J Fam Psychol. 2003;17:54-64.
55 Sprunger LW, Boyce WT, Gaines JA. Family-infant congruence: Routines and rhythmicity in family adaptations to a young infant. Child Dev. 1985;56:564-572.
56 Markson S, Fiese BH. Family rituals as a protective factor against anxiety for children with asthma. J Pediatr Psychol. 2000;25:471-479.
57 Fiese BH. Family rituals in alcoholic and nonalcoholic households: Relation to adolescent health symptomatology and problematic drinking. Fam Relat. 1993;42:187-192.
58 Stein REK, Jessop DJ. The Impact on Family Scale revisited: Further psychometric data. J Dev Behav Pediatr. 2003;24:9-16.
59 Quittner AL, Espelage DL, Opipari LC, et al. Role strain in couples with and without a child with a chronic illness: Associations with marital satisfaction, intimacy, and daily mood. Health Psychol. 1998;17:112-124.
60 Evans GW. The environment of childhood poverty. Am Psychol. 2004;59:77-92.
61 Evans GW, Gonnella C, Marcynyszyn LA, et al. The role of chaos and poverty and children’s socioemotional adjustment. Psychol Sci. 2005;16:560-565.
62 Dumas JE, Nissley J, Nordstrom A, et al. Home chaos: Sociodemographic, parenting, interactional, and child correlates. J Clin Child Adolesc Psychol. 2005;34:93-104.
63 Brody GH, Flor DL. Maternal psychological functioning, family processes, and child adjustment in rural, single-parent, African American families. Dev Psychol. 1997;33:1000-1011.
64 Fiese BH, Sameroff AJ, Grotevant HD, et al. The Stories that Families Tell: Narrative Coherence, Narrative Interaction, and Relationship Beliefs. Monographs of the Society for Research in Child Development. Malden, MA: Blackwell Publishers; 1999;64:1-36. (2), serial no. 257
65 Brody H. Stories of Sickness. New Haven, CT: Yale University Press, 1987.
66 Fiese BH, Bickham NL. Pincurling grandpa’s hair in the comfy chair: Parents’ stories of growing up and potential links to socialization in the preschool years. In: Pratt MW, Fiese BH, editors. Family Stories across Time and Generations. Mahwah, NJ: Erlbaum; 2004:259-278.
67 Peterson JL, Peterson M. The Sleep Fairy. Omaha, NE: Behave’n Kids Press, 2003.
68 Wang Q. The cultural context of parent-child reminiscing: A functional analysis. In: Pratt MW, Fiese BH, editors. Family Stories and the Life Course: Across Time and Generations. Mahwah, NJ: Erlbaum; 2004:279-301.
69 McAdams DP. The psychology of life stories. Rev Gen Psychol. 2001;5:100-122.
70 Fiese BH, Sameroff AJ. The family narrative consortium: A multidimensional approach to narratives. Fiese BH, Sameroff AJ, Grotevant HD, et al, editors. The Stories that Families Tell: Narrative Coherence, Narrative Interaction, and Relationship Beliefs. Monographs of the Society for Research in Child Development. Malden, MA: Blackwell Publishers; 1999;64:1-36. (2), serial no. 257
71 Coles R. The Call of Stories. Boston: Houghton Mifflin, 1989.
72 Remen RN. Kitchen Table Wisdom. New York: River-head Books, 1996.
73 Dickstein S, St. Andre M, Sameroff AJ, et al. Maternal depression, family functioning, and child outcomes: A narrative assessment. Fiese BH, Sameroff AJ, Grotevant HD, et al, editors. The Stories that Families Tell: Narrative Coherence, Narrative Interaction, and Relationship Beliefs. Monographs of the Society for Research in Child Development. Malden, MA: Blackwell Publishers; 1999;64:84-104. (2), serial no. 257
74 Fiese BH, Wamboldt FS. Coherent accounts of coping with a chronic illness: Convergences and divergences in family measurement using a narrative analysis. Fam Process. 2003;42:3-15.
75 Carlson EA, Sroufe LA, Egeland B. The construction of experience: A longitudinal study of representation and behavior. Child Dev. 2004;75:66-83.
76 van Ijzendoorn MH, Bakersmans-Kranenburg MJ. Attachment representations in mothers, fathers, adolescents and clinical groups: A meta-analytic search for normative data. J Consult Clin Psychol. 1996;64:8-21.
77 DiMatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Couns. 2004;55:339-344.
78 Fiese BH, Spagnola M. Narratives in and about family relationships: An examination of coding schemes and guide for family researchers. J Fam Psychol. 2005;19:51-61.
79 Pratt MW, Fiese BH. Families, stories and the life course: An ecological context. In: Pratt MW, Fiese BH, editors. Family Stories across Time and Generations. Mahwah, NJ: Erlbaum; 2004:1-26.
80 Fiese BH, Marjinsky KAT. Dinnertime stories: Connecting relationship beliefs and child behavior. Fiese BH, Sameroff AJ, Grotevant HD, et al, editors. The Stories that Families Tell: Narrative Coherence, Narrative Interaction, and Relationship Beliefs. Monographs of the Society for Research in Child Development. Malden, MA: Blackwell Publishers; 1999;64:52-68. (2), serial no. 257
81 Toth SL, Cicchetti D, Macfie J, et al. Representations of self and other in the narratives of neglected, physically abused, and sexually abused preschoolers. Dev Psychopathol. 1997;9:781-796.
82 Toth SL, Cicchetti D, Macfie J, et al. Narrative representations of caregivers and self in maltreated preschoolers. Attach Hum Dev. 2000;2:271-305.
83 Fiese BH, Wamboldt FS. Tales of pediatric asthma management: Family based strategies related to medical adherence and health care utilization. J Pediatr. 2003;143:457-462.
84 Markman HJ, Notarious CI. Coding marital and family interaction: Current status. In: Jacob T, editor. Family Interaction and Psychopathology. New York: Plenum Press; 1987:329-390.
85 Cohen MS. Families coping with childhood chronic illness: A research review. Fam Syst Health. 1999;17:149-164.
86 Minuchin S. Families and Family Therapy. Cambridge, MA: Harvard University Press, 1974.
87 Wood BL. Beyond the “psychosomatic family”: A biobehavioral family model of pediatric illness. Fam Process. 1993;32:261-278.
88 Kaugars AS, Klinnert MD, Bender BG. Family influences on pediatric asthma. J Pediatr Psychol. 2004;29:475-491.
89 McQuaid EL. Behavioral adjustment in children with asthma: A meta-analysis. J Dev Behav Pediatr. 2001;22:430-439.
90 Schobinger R, Florin I, Reichbauer M, et al. Childhood asthma: Mothers’ affective attitude, mother-child interaction, and children’s compliance with medical requirements. J Psychosom Res. 1993;37:697-707.
91 Bender BG, Milgrom H, Rand C, et al. Psychological factors associated with medication nonadherence in asthmatic children. J Asthma. 1998;35:347-353.
92 Christiannse ME, Lavigne JC, Lerner CV. Psychosocial aspects of compliance in children and adolescents with asthma. Dev Behav Pediatr. 1989;10:75-80.
93 Jacobson AM, Hauser ST, Lavori P, et al. Family environment and glycemic control: A four-year prospective study of children and adolescents with insulin dependent diabetes mellitus. Psychosom Med. 1994;56:401-409.
94 Drotar D. Relating parent and family to the psychological adjustment of children with chronic health conditions: What have we learned? What do we need to know? J Pediatr Psychol. 1997;22:149-165.
95 Epstein NB, Ryan CE, Bishop DS, et al. The McMaster model: A view of healthy family functioning. In: Walsh F, editor. Normal Family Processes. 3rd ed. New York: Guilford; 2003:581-607.
96 Kazak AE, McClure KS, Alderfer MA, et al. Cancer-related parental beliefs: The Family Illness Beliefs Inventory (FIBI). J Pediatr Psychol. 2004;29:531-542.
97 Stark LJ, Jelalian E, Powers SW, et al. Parent and child mealtime behavior in families of children with cystic fibrosis. J Pediatr. 2000;136:195-200.
98 Bihun JT, Wamboldt MZ, Gavin LA, et al. Can the Family Assessment Device (FAD) be used with children? Fam Process. 2002;41:723-731.
99 DeLambo KE, Ievers-Landis CE, Drotar D, et al. The association of observed family relationship quality and problem-solving skills with treatment adherence in older children and adolescents with cystic fibrosis. J Pediatr Psychol. 2004;29:343-354.
100 Speith LE, Stark LJ, Mitchell MJ, et al. Observational assessment of family functioning at mealtime in preschool children with cystic fibrosis. J Fam Psychol. 2001;26:215-224.
101 Hauser ST, Jacobson AM, Lavori P, et al. Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up: II. Immediate and long-term linkages with the family milieu. J Pediatr Psychol. 1990;15:527-542.
102 Wysocki T, Miller KM, Greco P, et al. Behav ior t her apy for families of adolescents with diabetes: Effects on directly observed family interactions. Behav Ther. 1999;30:507-525.
103 Markus HR, Kitayama S. A collective fear of the collective: Implications for selves and theories of selves. Pers Soc Psychol Bull. 1994;20:568-579.
104 Miller PJ, Wiley AR, Fung H, et al. Personal storytelling as a medium of socialization in Chinese and American families. Child Dev. 1997;68:557-568.
105 Goodnow J. Adding culture to studies of development: Toward changes in procedure and theory. Hum Dev. 2002;45:237-245.
106 Weisner TS. Ecocultural understanding of children’s developmental pathways. Hum Dev. 2002;45:275-281.
107 Falicov CJ. Immigrant family processes. In: Walsh F, editor. Normal Family Processes. 3rd ed. New York: Guilford; 2003:280-300.
108 Gonzales NA, Knight GP, Birman D, et al. Acculturation and enculturation among Latino youth. In: Maton KI, Schellenbach CJ, Leadbeater BJ, et al, editors. Investing in Children, Youth, Families, and Communities: Strengths-Based Research and Policy. Washington, DC: American Psychological Association; 2004:285-302.
109 Harwood RL. The influence of culturally derived values of Anglo and Puerto Rican mothers’ perceptions of attachment behaviors. Child Dev. 1992;63:822-839.
110 Harwood RL, Miller JG. Perceptions of attachment behavior: A comparison of Anglo and Puerto Rican mothers. Merrill Palmer Q. 1991;37:583-599.
111 Schultze PA, Harwood RL, Schoelmerich A. Feeding practices and expectations among middle-class Anglo and Puerto Rican mothers of 12-month old infants. J Cross Cult Psychol. 2001;32:397-406.
112 Harwood RL, Miller JG, Irizarry NL. Culture and Attachment: Perceptions of the Child in Context. New York: Guilford, 1995.
113 Triandis HC, Marin G, Lisansky J, et al. Simpatia as a cultural script of Hispanics. J Pers Soc Psychol. 1984;47:1363-1375.
114 Arcia E, Fernandez MC, Jaquez M. Latina mothers’ characterizations of their young children with disruptive behaviors. J Child Fam Stud. 2005;14:111-125.
115 Gannotti ME, Handwerker WP. Puerto Rican understanding of child disability: Methods for the cultural validation of standardized measures of child health. Soc Sci Med. 2002;55:2093-2105.
116 Fuligini AJ, Yip T, Tseng V. The impact of family obligation on the daily activities and psychological well-being of Chinese American adolescents. Child Dev. 2002;73:302-314.
117 Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: Parent perspectives. Pediatrics. 2000;106:512-519.
118 Wade SL, Islam S, Holden G, et al. Division of responsibility for asthma management tasks between caregivers and children in the inner city. Dev Behav Pediatr. 1999;20:93-98.
119 Walders N, Drotar D, Kercsmar C. The allocation of family responsibility for asthma management tasks in African-American adolescents. J Asthma. 2000;37:89-99.
120 Yali AM, Revenson TA. How changes in population demographics will impact health psychology: Incorporating a broader notion of cultural competence in the field. Health Psychol. 2004;23:147-155.
121 Beiser M, Hou F, Hyman I, et al. Poverty, family process, and mental health of immigrant children in Canada. Am J Public Health. 2002;92:220-227.
122 Parke RD, Coltrane S, Duffy S, et al. Economic stress, parenting, and child adjustment in Mexican American and European American families. Child Dev. 2004;75:1632-1656.
123 Drotar D. Psychological Interventions in Childhood Chronic Illness. Washington, DC: American Psychological Association, 2006.
124 Pinsof WM, Lebow JL, editors. Family Psychology: The Art of the Science. Oxford, UK: Oxford University Press, 2005.
125 Power TJ, DuPaul GJ, Shapiro ES, et al. Promoting Children’s Health: Integrating School, Family, and Community. New York: Guilford, 2003.
126 Kazak AE, Simms S, Rourke MT. Family systems practice in pediatric psychology. J Pediatr Psychol. 2002;27:133-144.
127 Mikesell DH, McDaniel SH, editors. Integrating Family Therapy: Handbook of Family Psychology and Systems Theory. Washington, DC: American Psychological Association, 1995.
128 Wysocki T, Harris MA, Greco P, et al. Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol. 2000;25:23-33.
129 Kazak AE, Simms S, Alderfer MA, et al. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. J Pediatr Psychol. 2005;30:644-655.
130 Drotar D. Commentary: Involving families in psychological interventions in pediatric psychology: Critical needs and dilemmas. J Pediatr Psychol. 2005;30:689-693.
131 Sameroff AJ. The social context of development. In: Eisenberg N, editor. Contemporary Topics in Developmental Psychology. New York: Wiley; 1987:273-291.
132 Fiese BH, Wamboldt FS. Family routines, rituals, and asthma management: A proposal for family based strategies to increase treatment adherence. Fam Syst Health. 2001;18:405-418.
133 Anderson B, Brackett J, Ho J, et al. An intervention to promote family teamwork in diabetes management tasks. In: Drotar D, editor. Promoting Adherence to Medical Treatment and Chronic Childhood Illness. Mahwah, NJ: Erlbaum; 2000:347-365.
134 Lucyshyn JM, Kayser AT, Irvin LK, et al. Functional assessment and positive behavior support at home with families: Defining effective and contextually appropriate behavior support plans. In: Lucyshyn JM, Dunlap G, editors. Families and Positive Behavior Support: Addressing Problem Behavior in Family Contexts. Baltimore, MD: Paul H. Brookes; 2002:97-132.
135 Olds DL. Prenatal and infancy home visiting by nurses: From randomized trials to community replication. Prev Sci. 2002;3:153-172.
136 Rosenthal CJ, Marshall VW. Generational transmission of family ritual. Am Behav Sci. 1988;31:669-684.
137 Buschbacher P, Fox L, Clarke S. Recapturing desired family routines: A parent-professional behavioral collaboration. Res Pract Persons Severe Disabl. 2004;29:25-39.
138 Woods J, Goldstein H. When the toddler takes over: Changing challenging routines into conduits for communication. Focus Autism Other Dev Disabl. 2003;18:176-181.
139 Kazak AE, Alderfer MA, Rourke MT, et al. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29:211-219.
140 Kazak AE, Alderfer MA, Streisand R, et al. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: A randomized clinical trial. J Fam Psychol. 2004;18:493-504.
141 Kazak AE, Simms S, Barakat L, et al. Surviving Cancer Competently Intervention Program (SCCIP): A cognitive-behavioral and family therapy intervention for adolescent survivors of childhood cancer and their families. Fam Process. 1999;38:175-191.
142 Browne JV, Talmi A. Family-based intervention to enhance infant-parent relationships in the neonatal intensive care unit. J Pediatr Psychol. 2005;30:667-677.
143 McDonough SC. Interaction guidance: Understanding and treating early infant-caregiver relationship disturbances. In: Zeenah CH, editor. Handbook of Infant Mental Health. New York: Guilford; 1993:414-426.
144 Henggeler SW. Multisystemic therapy: An overview of clinical procedures, outcomes, and policy implications. Child Psychol Psychiatry Rev. 1999;4:2-10.
145 Ellis DA, Naar-King S, Frey M, et al. Multisystemic treatment of poorly controlled type I diabetes: Effects on medical resource utilization. J Pediatr Psychol. 2005;30:656-666.
146 McDaniel SH, Campbell TL, Hepworth J, et al, editors. Family-Oriented Primary Care, 2nd ed., New York: Springer, 2005.
147 Kerig P, Lindahl K, editors. Family Observational Coding Systems: Resources for Systemic Research. Mahwah, NJ: Erlbaum, 2001.
148 Holmbeck GN, Coakley RM, Hommeyer JS, et al. Observed and perceived dyadic and systemic functioning in families of preadolescents with spina bifida. J Pediatr Psychol. 2002;27:177-189.
149 Dickstein S, Hayden LC, Schiller M, et al. Providence Family Study Mealtime Family Interaction Coding System. Adapted from the McMaster Clinical Rating Scale. East Providence, RI: E. P. Bradley Hospital, 1994.
150 Jacobs MP, Fiese BH. Family mealtime interactions and overweight children with asthma: Potential for compounded risks? J Pediatr Psychol. 2007;32:64-68.
151 Barney MC, Max JE. The McMaster family assessment device and clinical rating scale: Questionnaire vs. interview in childhood traumatic brain injury. Brain Inj. 2005;19:801-809.
152 LaGreca AM, Auslander WF, Greco P, et al. I get by with a little help from my family and friends: Adolescents’ support for diabetes care. J Pediatr Psychol. 1995;20:449-476.
153 Schroff Pendley J, Kasmen LJ, Miller DL, et al. Peer and family support in children and adolescents with type 1 diabetes. J Pediatr Psychol. 2002;27:429-438.
154 Smilkstein G. The Family APGAR: A proposal for family function test and its use by physicians. J Fam Pract. 1978;6:1231-1239.
155 Palermo TM, Childs G, Burgess ES, et al. Functional limitations of school-aged children seen in primary care. Child Care Health Dev. 2002;28:379-389.
156 Jellinek MS, Murphy JM, Robinson J, et al. Pediatric Symptom Checklist: Screening school-age children for psychosocial dysfunction. J Pediatr. 1988;112:201-209.
157 Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J Marital Fam Ther. 1983;9:171-180.
158 Liakopoulou-Karis M, Alifieraki T, Protagora D, et al. Recurrent abdominal pain and headache: Psychopathology, life events, and family functioning. Eur Child Adolesc Psychiatry. 2002;11:115-122.
159 Shonkoff JP, Phillips DA, editors. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academies Press, 2000.
160 Cicchetti D, Dawson G. Editorial: Multiple levels of analysis. Dev Psychopathol. 2002;14:417-420.
161 Walsh F. A family resilience framework: Innovative practice applications. Fam Relat. 2002;51:130-137.
162 Huston AC. Connecting the science of child development to public policy. SRCD Public Policy Rep. 2005;19(4):3-7.