29 Fallot’s tetralogy
Salient features
Examination
• Left parasternal heave with normal left ventricular impulse
• Second sound is single (absent second pulmonic sound)
• Ejection systolic murmur heard in the pulmonary area
Advanced-level questions
What is the survival of Fallot’s Tetralogy?
The rate of survival in uncorrected patients (Am J Cardiol 1978;42:458–66) is:
What do you know regarding the relation between congenital heart disease and embryology of heart development?
In order of embryologic development, the steps embryogenesis include:
1 Looping, laterality and single-ventricle defects (e.g. double-inlet LV, situs inversus totalis)
2 Conotruncal defects (e.g. tetralogy of Fallot, double-outlet RV)
3 Atrioventricular canal defects (e.g. endocardial cushion defect, common atrioventricular canal defect)
4 Right ventricular outflow tract obstruction (e.g. pulmonary valve atresia or stenosis, Ebstein’s anomaly)
5 Left ventricular outflow tract obstruction (e.g. aortic valve atresia or stenosis, hypoplastic left heart)
6 Septal defects (e.g. ventricular septal defect, atrial septal defect)
What is the treatment for Fallot’s tetralogy?
• Total correction under the age of 1 year when there is no need for an outflow transannular patch. A second-stage total correction can be performed when the child is over the age of 2 years. The mortality associated with surgery is <3% in children and 2.5 to 8.5% in adults.
• Blalock–Taussig shunting is performed nowadays only if the anatomy is unfavourable for a total correction.
• Modified Blalock–Taussig shunting is the interposition of a tubular graft between the subclavian and pulmonary arteries.
• The Waterston shunt involves anastomosis of the back of the ascending aorta to the pulmonary artery. It is used when surgery is required in a child younger than 3 months, because the subclavian artery is too small for a good Blalock–Taussig shunt.
• The Potts shunt involves anastomosis of the descending aorta to the back of the pulmonary artery (JAMA 1946;132:627).
• The Glenn operation involves anastomosis of the superior vena cava to the right pulmonary artery. The bidirectional Glenn procedure involves anastomosis of the superior vena cava to both pulmonary arteries.
• Pulmonary balloon valvuloplasty is sometimes used as an alternative for surgery.
What is Fallot’s triology?
Atrial septal defect, pulmonary stenosis and right ventricular hypertrophy.
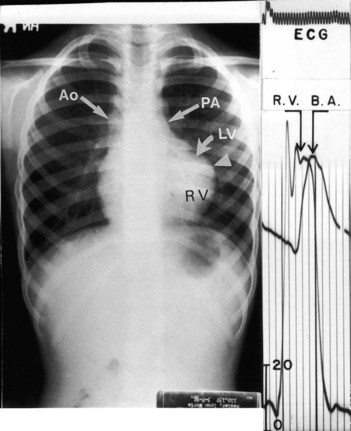
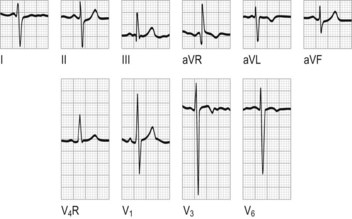
What are the findings from investigations?
What are the arrhythmias detected with Holter monitoring with repaired tetralogy of Fallot?
What are long-term complications in patients with repaired tetralogy of Fallot?
• Pulmonary regurgitation may develop as a result of surgical repair of the right ventricular outflow tract).
• Enlargement of the RV occurs, resulting in RV dysfunction, and repair or replacement of the pulmonary valve may be required.
• An aneurysm may form at the site where the RV outflow tract was repaired.
• Residual or recurrent obstruction of the RV outflow tract, requiring repeated surgery.
• Residual ventricular septal defects in approximately 10–20% of patients with repaired tetralogy of Fallot; such patients may require repeated surgery if the defects are of sufficient size.
• Right bundle branch block is common after repair of tetralogy of Fallot, but complete heart block is rare.
• Aortic root dilatation resulting in aortic regurgitation, usually mild.