Problem 42 Fall during a fishing weekend
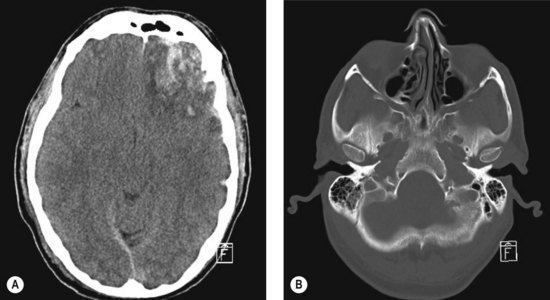
You perform the most important investigation, shown in Figure 42.1A, B.
Q.7
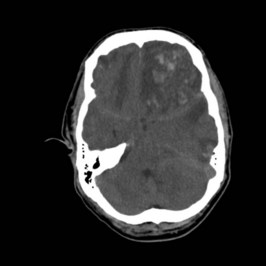
The patient is intubated emergently and an urgent CT head scan is performed. What does Figure 42.2 show?
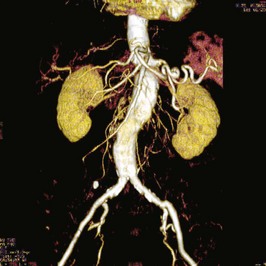
The patient is taken to the operating room and undergoes emergency frontal craniectomy, durotomy and insertion of an external ventricular drain. The intraoperative pathology is shown in Figure 42.3.
Answers
A.1 The patient has sustained a traumatic brain injury and should be assessed using the standardized guidelines for all trauma patients. These include assessment of airway, breathing and circulation (A, B, C), immobilization of the cervical spine and the performance of a brief neurological examination (primary survey). Following this a more detailed secondary survey may be performed to look for further injuries. These principles are detailed in the emergency management of severe trauma (EMST) course manual available through the Royal Australasian College of Surgeons (Committee on Trauma, American College of Surgeons 2008).
A.2 The Glasgow coma score (GCS), originally reported by Drs Teasdale and Jennett in 1974 (Teasdale and Jennet 1974), is an attempt to quantify the level of consciousness of a patient with a head injury in a form which is standardized and hence comparable from place to place, from time to time, and from person to person. The three summed components include the response to eye opening (E), motor response (M) and verbal response (V) (Table 42.1).
| Eye Opening | Motor Response | Verbal Response |
|---|---|---|
| 4 Spontaneous | 6 Obeys command | 5 Orientated |
| 3 To voice | 5 Localizes to pain | 4 Confused |
| 2 To pain | 4 Withdraws from pain | 3 Inappropriate words |
| 1 None | 3 Flexion to pain | 2 Incomprehensible |
| 2 Extension to pain | 1 None | |
| 1 None |
Committee on Trauma, American College of Surgeons. ATLS: Advanced trauma life support program for doctors, 8th edn. Chicago: American College of Surgeons; 2008. Available through Royal Australasian College of Surgeons
Teasdale G., Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81-84.