Chapter 2 Fair Game
Maki DD, Grossman RI. Patterns of disease spread in metastatic breast carcinoma: influence of estrogen and progesterone receptor status. AJNR Am J Neuroradiol. 2000;21:1064-1066.
Walker R, Kessar P, Blanchard R, et al. Turbo STIR magnetic resonance imaging as a whole-body screening tool for metastases in patients with breast carcinoma: preliminary clinical experience. J Magn Reson Imaging. 2000;11:343-350.
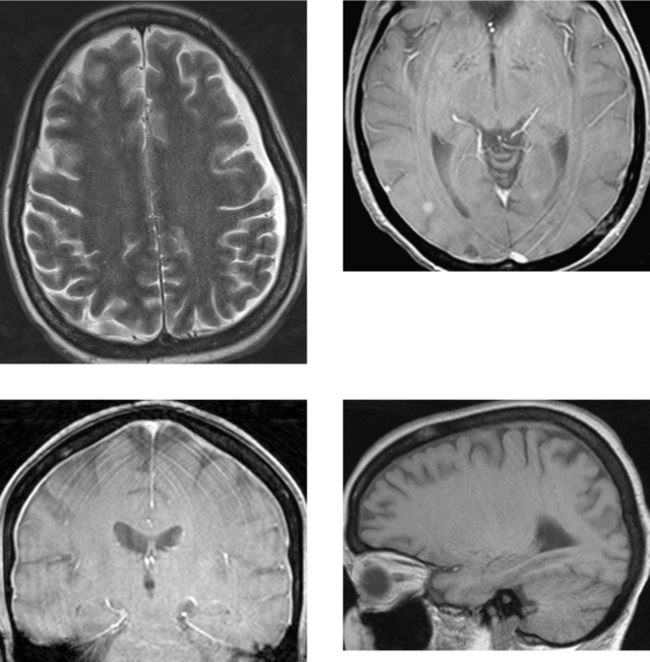
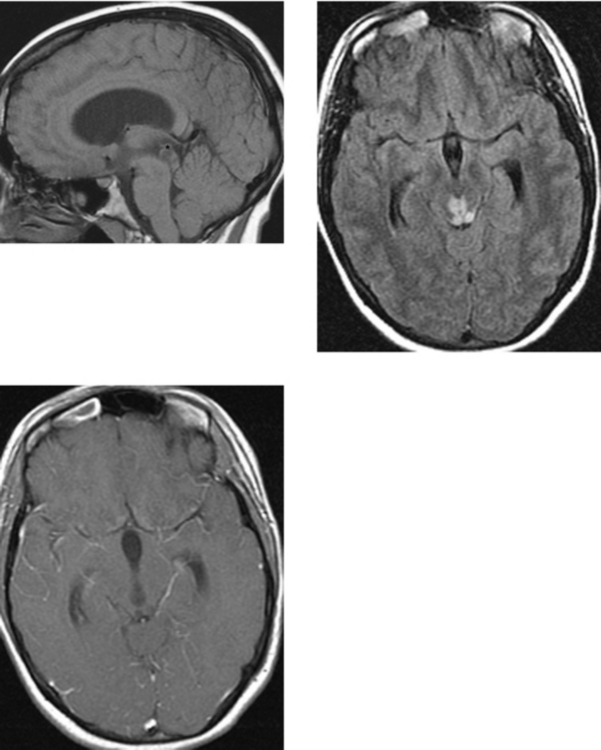
CASE 52 Aqueductal Stenosis
CASE 53 Rathke’s Cleft Cyst
CASE 54 Optic Neuritis (Demyelinating Disease)
Al-Shafai, Mikulis DJ. Diffusion MR imaging in a case of acute ischemic optic neuropathy. Am J Neuroradiol. 2006;27:255-257.
Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med. 1993;329:1764-1769.
CASE 55 Ocular Trauma—Lens Dislocation and Globe Rupture
CASE 56 Developmental Venous Anomaly
CASE 57 Fibrous Dysplasia of the Calvaria
CASE 58 Cavernous Sinus Mass—Meningioma
Hirsch WLJr, Hryshko FG, Sekhar LN, et al. Comparison of MR imaging, CT, and angiography in the evaluation of the enlarged cavernous sinus. AJNR Am J Neuroradiol. 1988;9:907-915.
Hudgins PA. Imaging of the cavernous sinus: management of cavernous sinus pathology. Techniques in Neurosurgery. 2003;8:211-219.
CASE 59 Pyogenic Ventriculitis with Acute Hydrocephalus
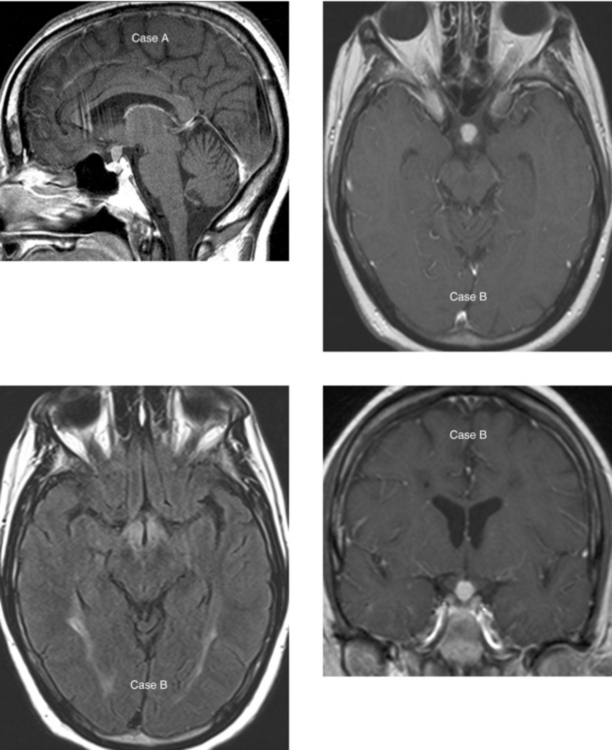
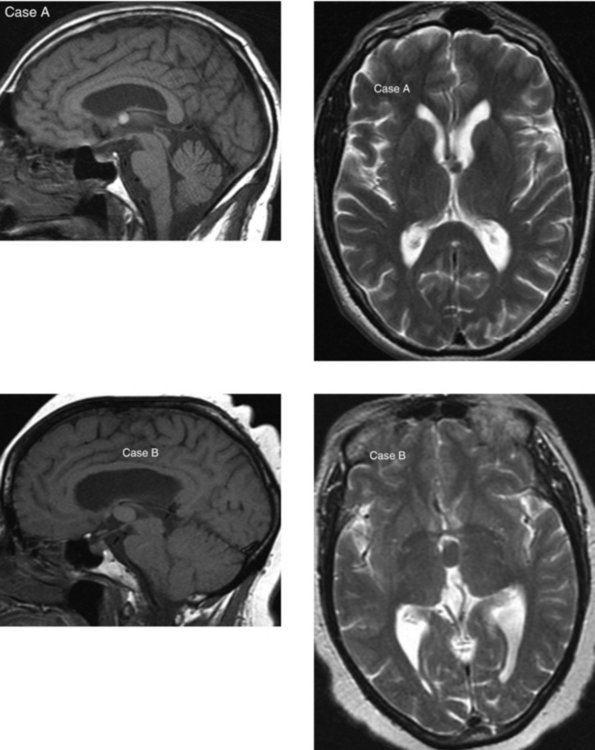
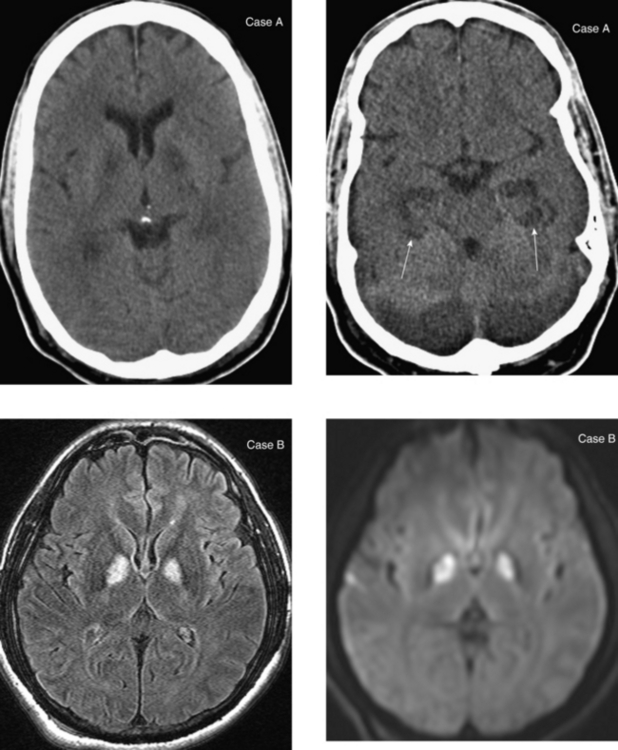
CASE 60 Lesions of the Pituitary Stalk and Hypothalamus: Case A—Sarcoidosis; Case B—Langerhans’ Cell Histiocytosis
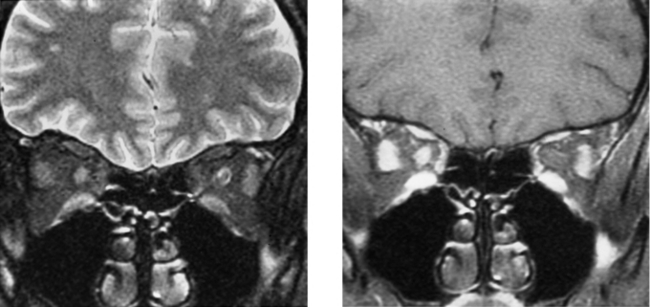
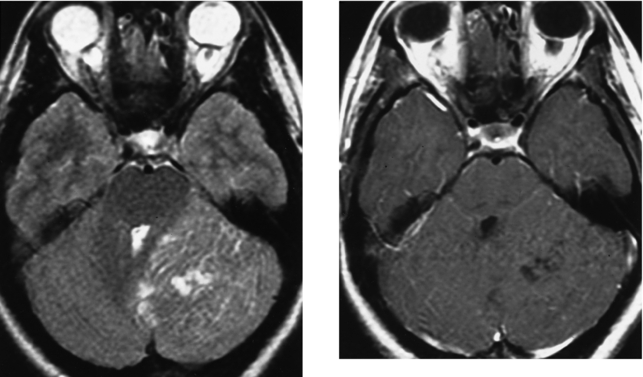
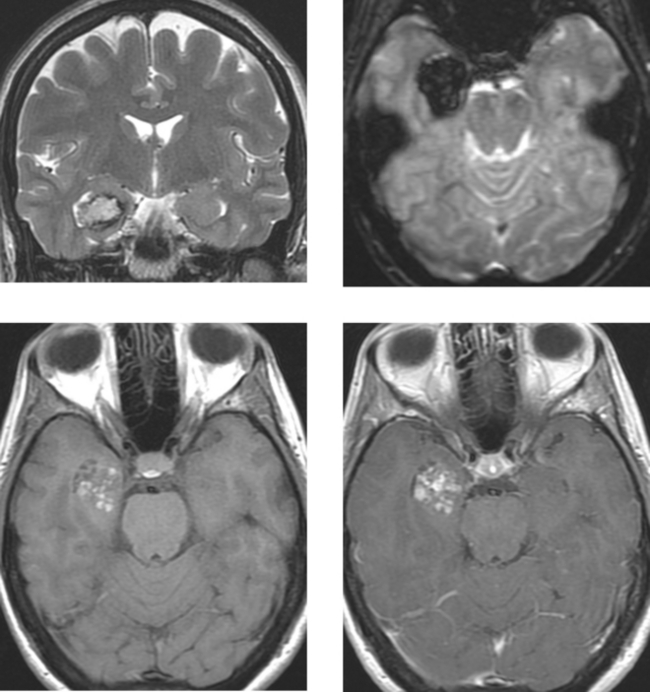
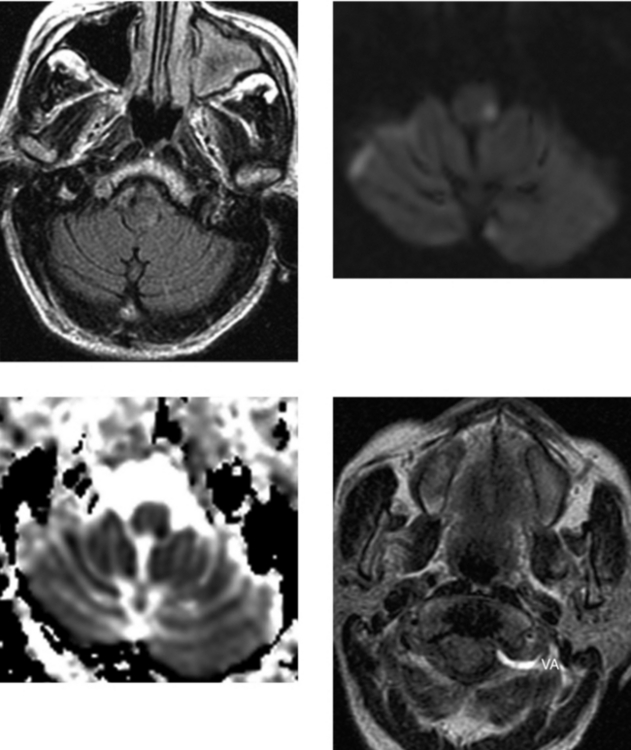
CASE 61 Lhermitte-Duclos Disease (Dysplastic Gangliocytoma of the Cerebellum)
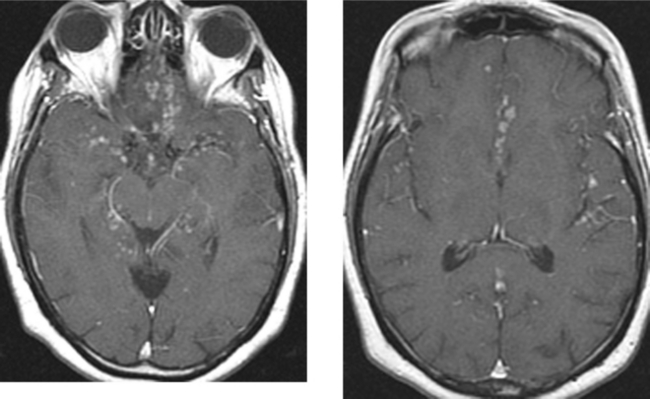
CASE 62 Basilar Meningitis—Sarcoidosis
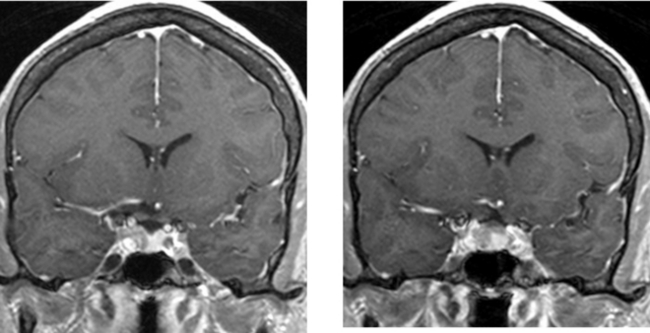
CASE 63 Pituitary Microadenoma
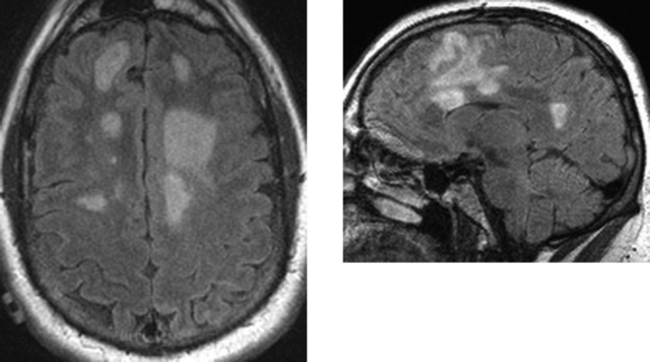
CASE 64 Multiple Sclerosis—Marburg Type
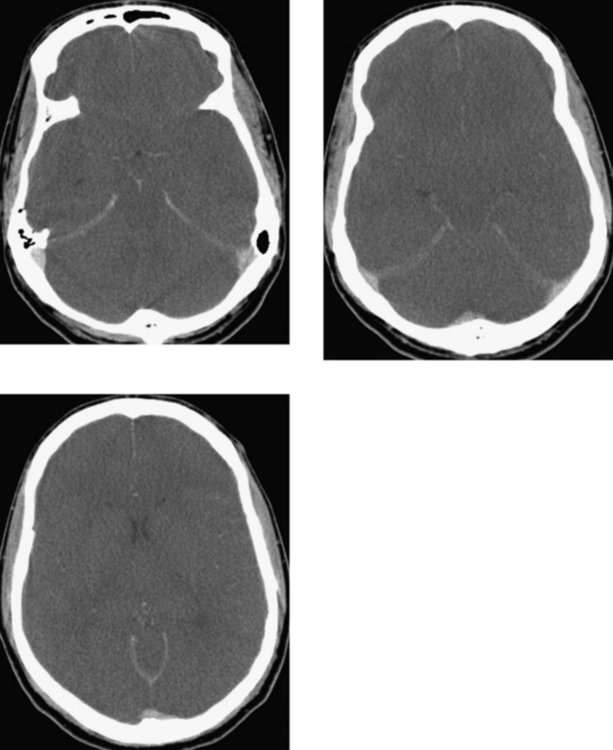
CASE 65 Transtentorial Herniation
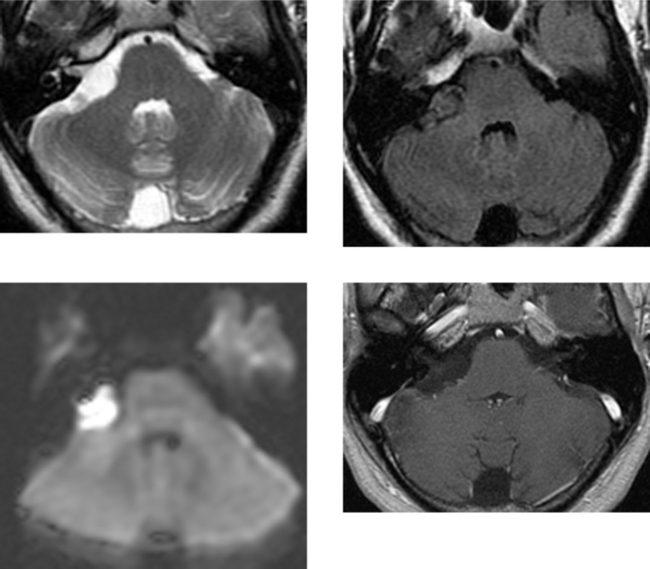
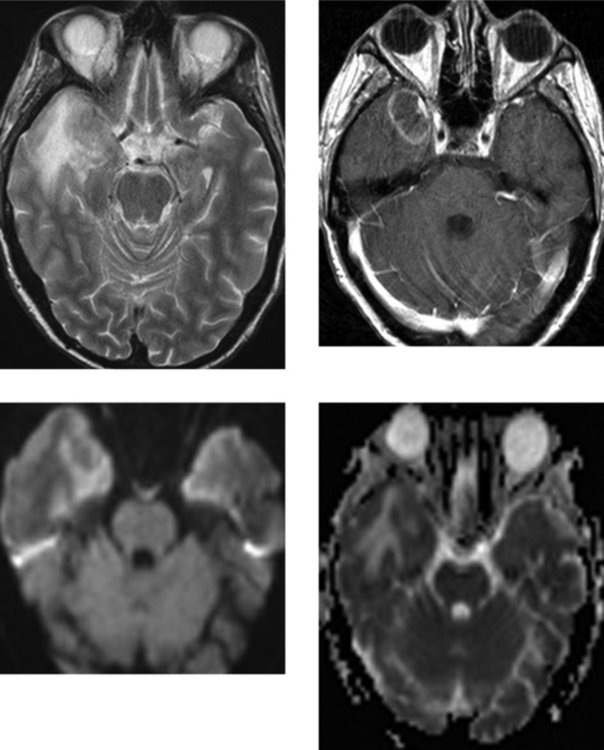
CASE 66 Epidermoid Cyst—Cerebellopontine Cistern
Kallmes DF, Provenzale JM, Cloft HJ, McClendon RE. Typical and atypical MR imaging features of intracranial epidermoid tumors. AJR Am J Roentgenol. 1997;169:883-887.
Tien RD, Felsberg GJ, Lirng JF. Variable bandwidth steady-state free-precession MR imaging: a technique for improving characterization of epidermoid tumor and arachnoid cyst. AJR Am J Roentgenol. 1995;164:689-692.
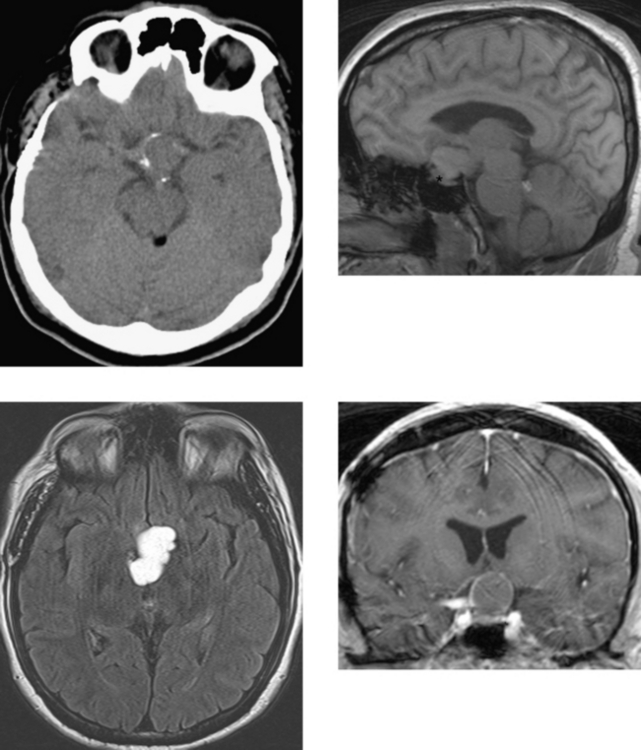
CASE 67 Cavernous Malformation (Cavernous Hemangioma, Occult Cerebrovascular Malformation)
CASE 68 Persistent Trigeminal Artery
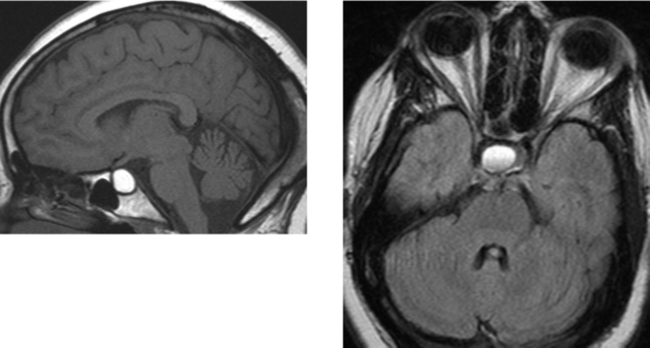
CASE 69 Colloid Cyst
Armao D, Castillo M, Chen H, Kwock L. Colloid cyst of the third ventricle: imaging-pathologic correlation. AJNR Am J Neuroradiol. 2000;21:1470-1477.
El Khoury C, Brugieres P, Decq P, et al. Colloid cysts of the third ventricle: are MR imaging patterns predictive of difficulty with percutaneous treatment? AJNR Am J Neuroradiol. 2000;21:489-492.
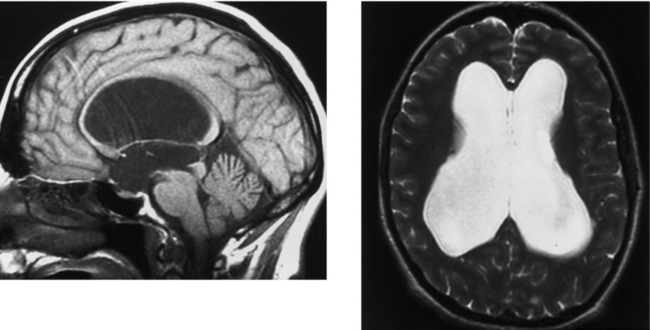
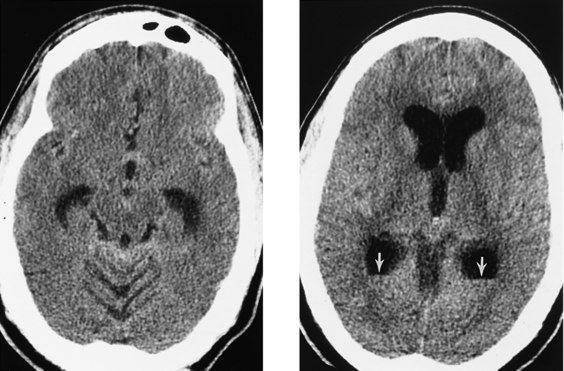
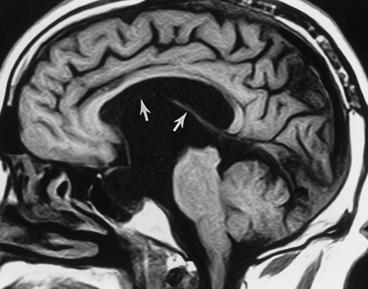
CASE 70 Cavum Septum Pellucidum and Cavum Vergae
Cowley AR, Moody DM, Alexander EJr, Ball MR, Laster DW. Distinctive CT appearance of cyst of the cavum septi pellucidi. AJR Am J Roentgenol. 1979;133:548-550.
Nakano S, Hojo H, Kataoka K, Yamasaki S. Age related incidence of cavum septi pellucidi and cavum vergae on CT scans of pediatric patients. J Comput Assist Tomogr. 1982;5:348-349.
Silbert PL, Gubbay SS, Vaughan RJ. Cavum septum pellucidum and obstructive hydrocephalus. J Neurol Neurosurg Psychiatry. 1993;56:820-822.
CASE 71 Toxoplasmosis Infection in Acquired Immunodeficiency Syndrome
Camacho DL, Smith JK, Castillo M. Differentiation of toxoplasmosis and lymphoma in AIDS patients by using apparent diffusion coefficients. AJNR Am J Neuroradiol. 2003;24:633-637.
Ernst TM, Chang L, Witt MD, et al. Cerebral toxoplasmosis and lymphoma in AIDS: perfusion MR imaging experience in 13 patients. Radiology. 1998;208:663-669.
CASE 72 Encephalocele—Developmental
CASE 73 Cysticercosis of the Central Nervous System
Arriada-Mendicoa N, Celis-Lopez MA, Higuera-Calleja J, Corona-Vazquez T. Imaging features of sellar cysticercosis. AJNR Am J Neuroradiol. 2003;24:1386-1389.
Braga F, Rocha AJ, Gomes HR, Filho GH, Silva CF, Fonseca RB. Noninvasive MR cisternography with fluid-attenuated inversion recovery and 100% supplemental O2 in the evaluation of neurocysticercosis. AJNR Am J Neuroradiol. 2004;25:295-297.
CASE 74 Facial Nerve—Inflammation (Viral)
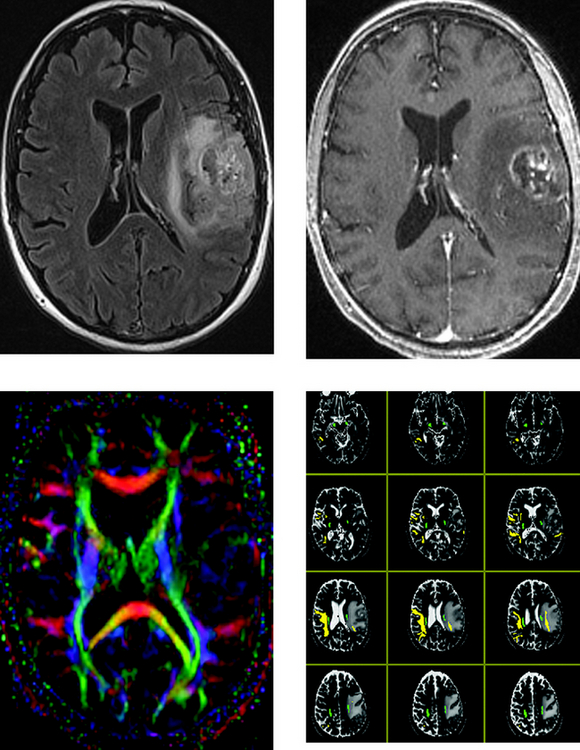
CASE 75 Magnetic Resonance Tractography— Preoperative Mapping of the Corticospinal Tracts for Glioblastoma Multiforme Resection
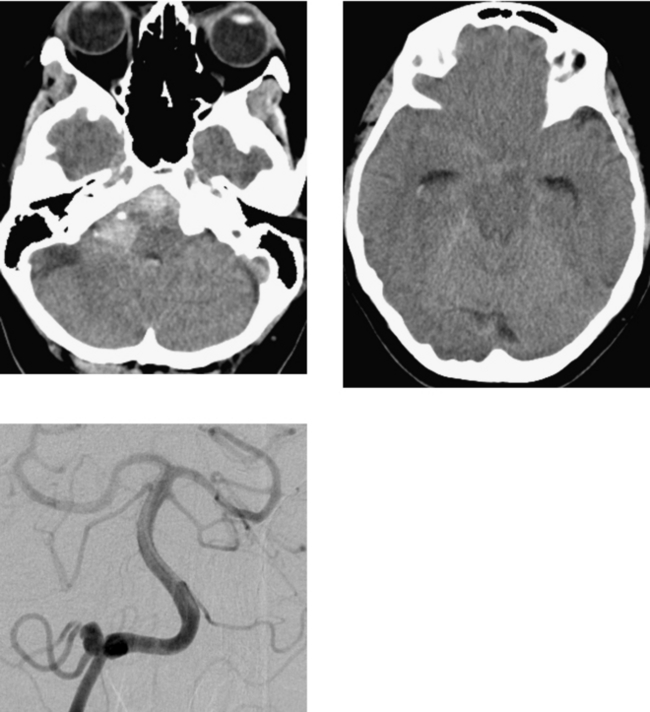
CASE 76 Right Posterior Inferior Cerebellar Artery Aneurysm Rupture
CASE 77 Ganglioglioma
Koeller KK, Henry JM. From the archives of the AFIP: superficial gliomas. Radiologic-pathologic correlation. RadioGraphics. 2001;21:1533-1556.
Provenzale JM, Ali U, Barboriak DP, Kallmes DF, Delong DM, McLendon RE. Comparison of patient age with MR imaging features of gangliogliomas. AJR Am J Roentgenol. 2000;174:859-862.
CASE 78 Paget’s Disease—Osteitis Deformans
Richards PS, Bargiota A, Corrall RJ. Paget’s disease causing an Arnold-Chiari type 1 malformation: radiographic findings. AJR Am J Roentgenol. 2001;176:816-817.
Tehranzadeh J, Fung Y, Donohue M, Anavim A, Pribram HW. Computed tomography of Paget’s disease of the skull versus fibrous dysplasia. Skeletal Radiol. 1998;27:664-672.
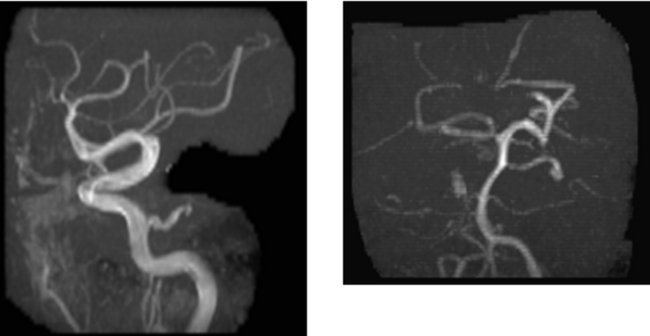
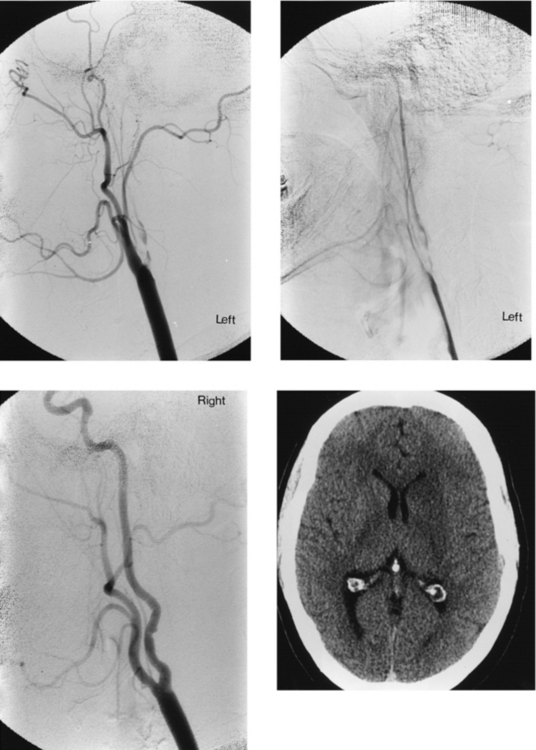
CASE 79 Fibromuscular Dysplasia—Complicated by Acute Stroke
CASE 80 Carbon Monoxide Poisoning
CASE 81 Lateral Medullary Syndrome—Wallenberg’s Syndrome
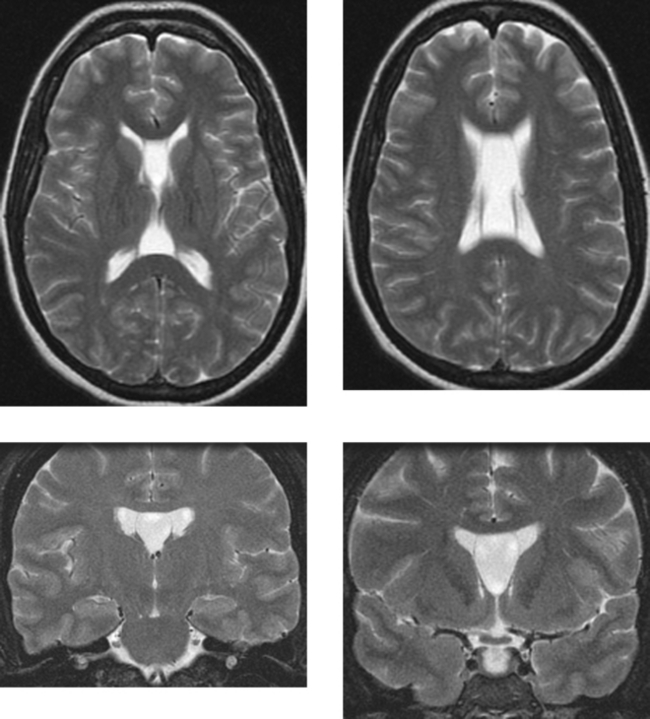
CASE 82 Wallerian Degeneration
Mazumdar A, Mukherjee P, Miller JH, Malde H, McKinstry RC. Diffusion-weighted imaging of acute corticospinal tract injury preceding Wallerian degeneration in the maturing human brain. AJNR Am J Neuroradiol. 2003;24:1057-1066.
Uchino A, Sawada A, Takase Y, Egashira R, Kudo S. Transient detection of early Wallerian degeneration on diffusion weighted MRI after an acute cerebrovascular accident. Neuroradiology. 2004;46:183-188.
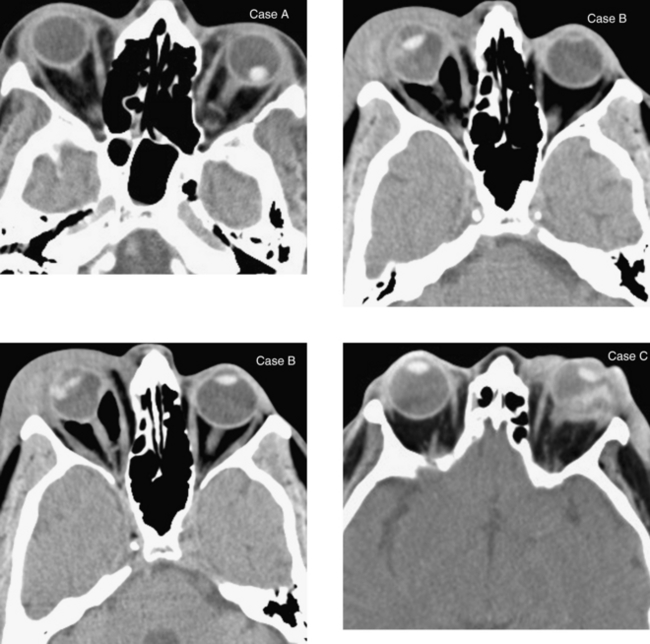
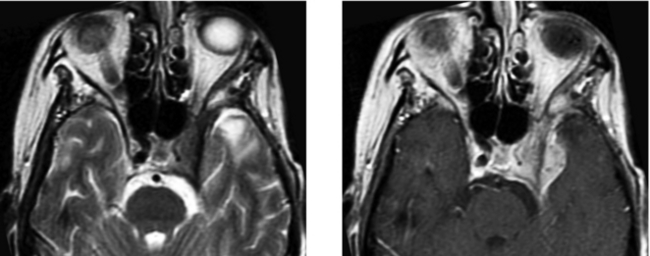
CASE 84 Thyroid Ophthalmopathy—with Optic Nerve Compression in the Orbital Apex
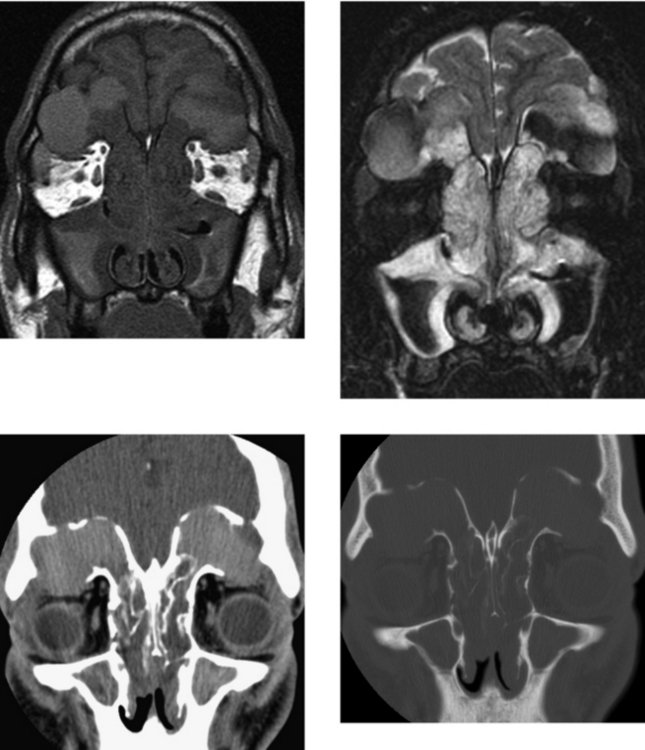
CASE 85 Bilateral Frontal Sinus Mucoceles
Ishibashi T, Kikuchi S. Mucocele-like lesions of the sphenoid sinus with hypointense foci on T2-weighted magnetic resonance imaging. Neuroradiology. 2001;43:1108-1111.
Tassel P, Lee YY, Jing BS, De Pena CA. Mucoceles of the paranasal sinuses: MR imaging with CT correlation. AJR Am J Roentgenol. 1989;153:407-412.
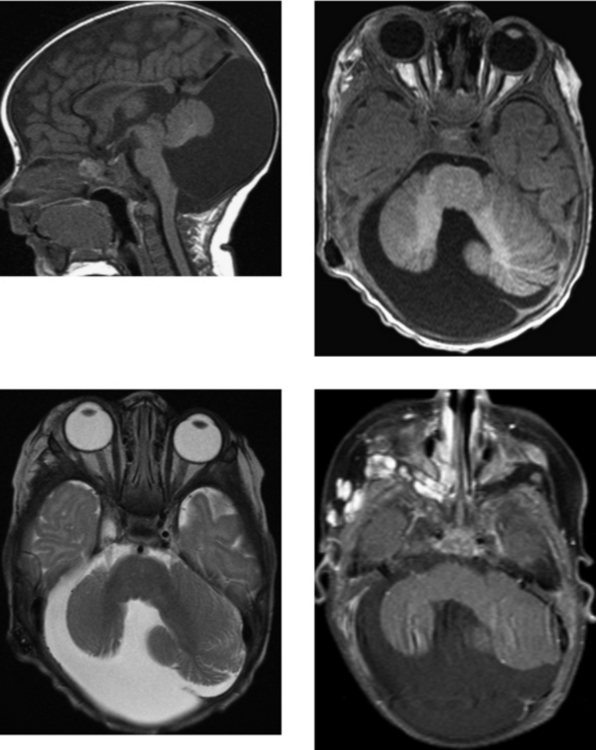
CASE 86 Suprasellar Cistern Arachnoid Cyst
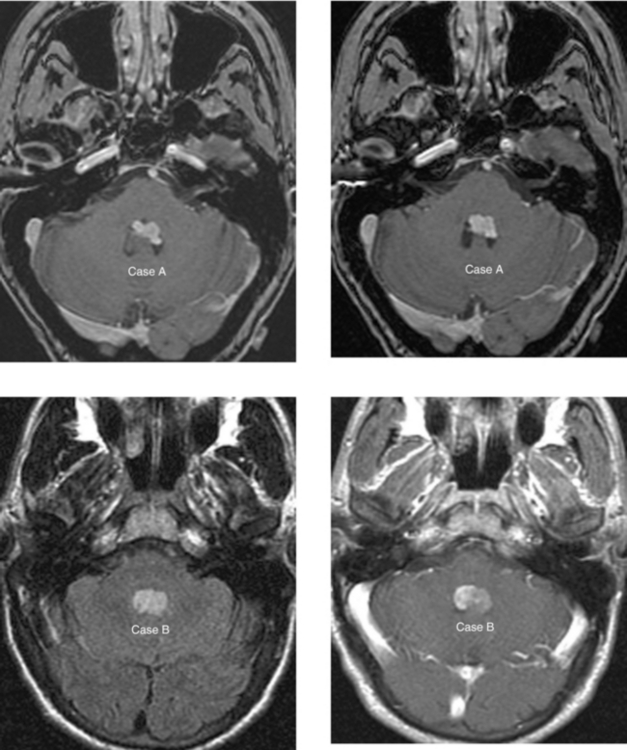
CASE 87 Fourth Ventricular Neoplasms—Choroid Plexus Papilloma and Ependymoma
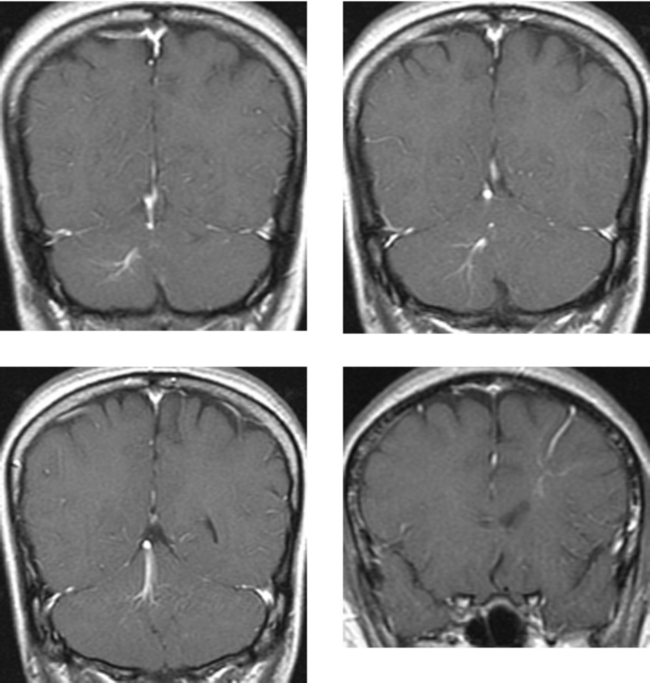
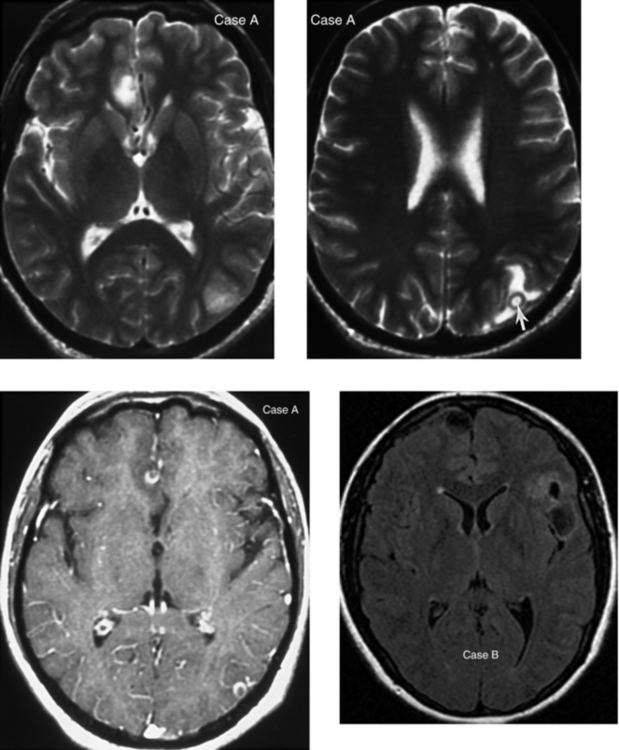
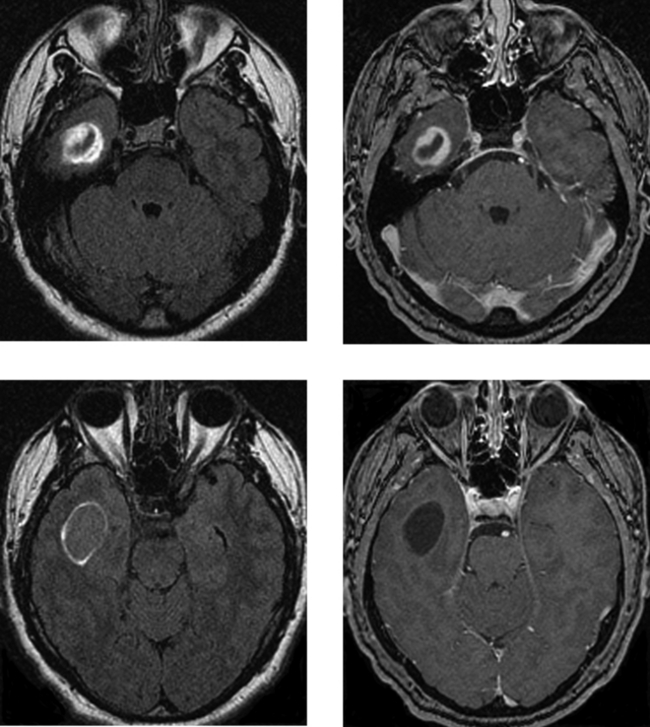
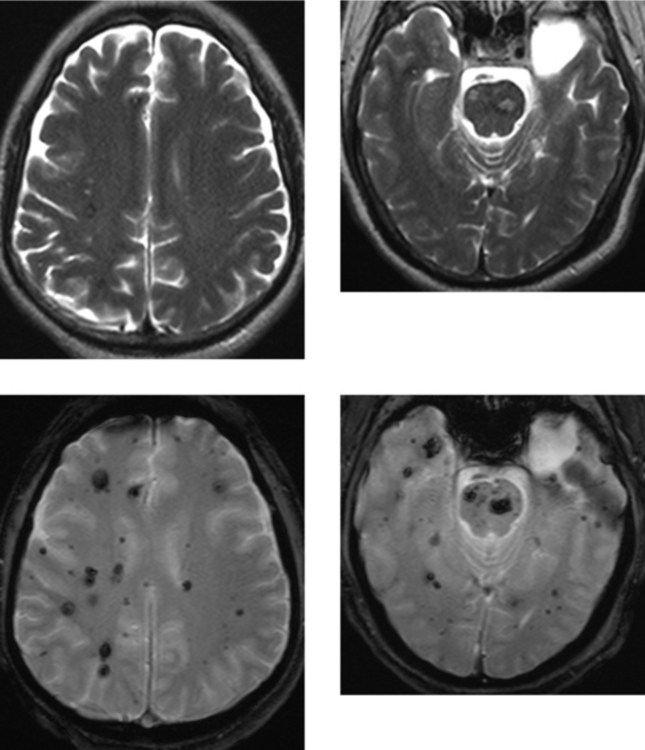
CASE 88 Multiple Cavernous Malformations—Familial Pattern
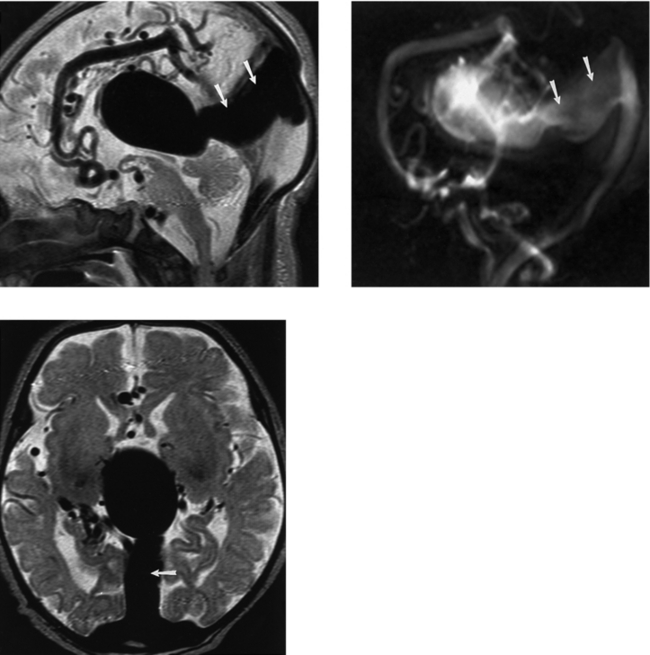
CASE 89 Vein of Galen Aneurysm
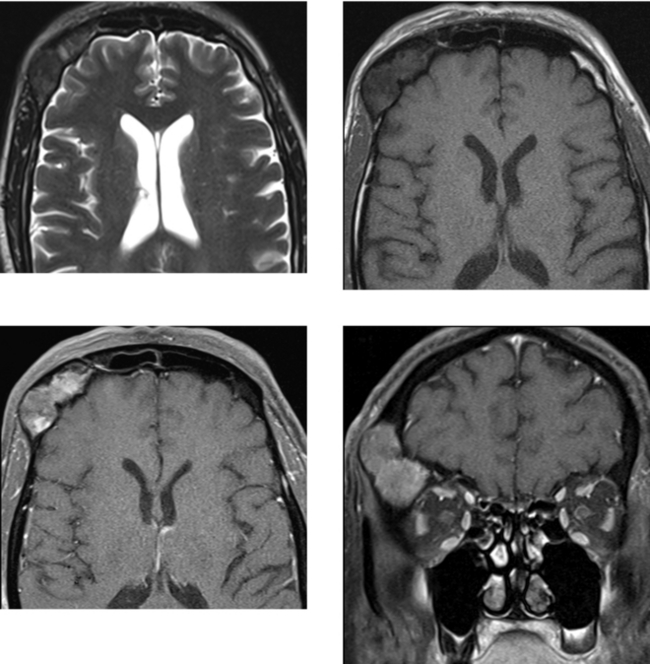
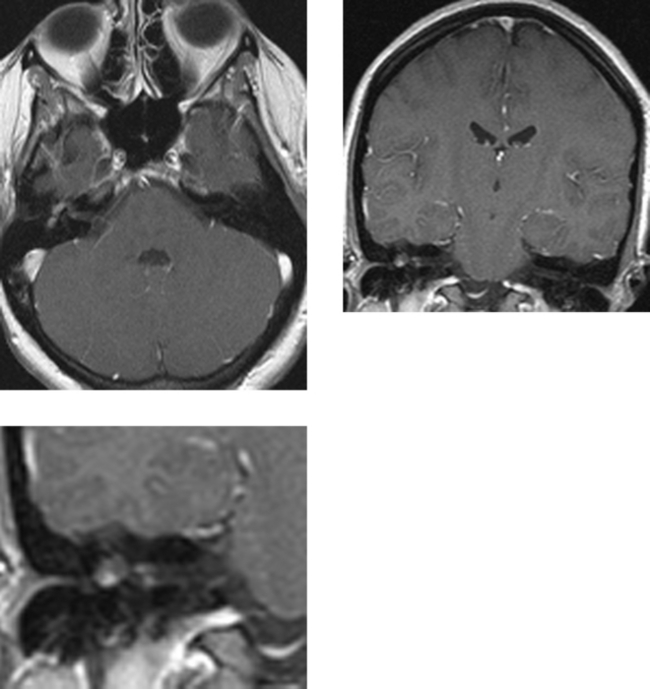
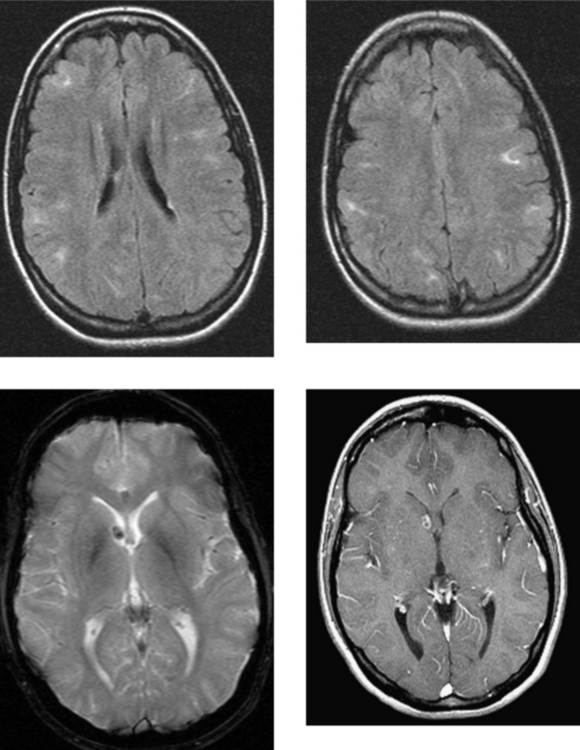
CASE 90 Tuberous Sclerosis (Bourneville’s Disease)
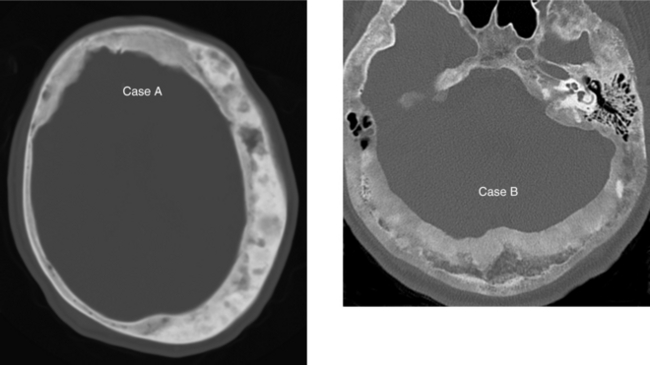
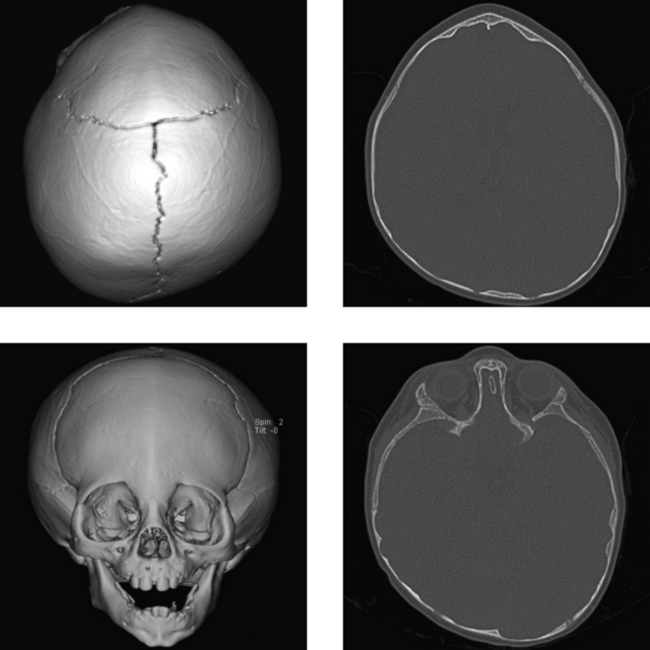
CASE 91 Craniosynostosis—Metopic Suture
Aviv RI, Rodger E, Hall CM. Craniosynostosis. Clin Radiol. 2002;57:93-102.
Medina LS. Three-dimensional CT maximum intensity projections of the calvaria: a new approach for diagnosis of craniosynostosis and fractures. AJNR Am J Neuroradiol. 2000;12:1951-1954.
Ngo AV, Sze RW, Parisi MT, et al. Cranial suture simulator for ultrasound diagnosis of craniosynostosis. Pediatr Radiol. 2004;34:535-540.
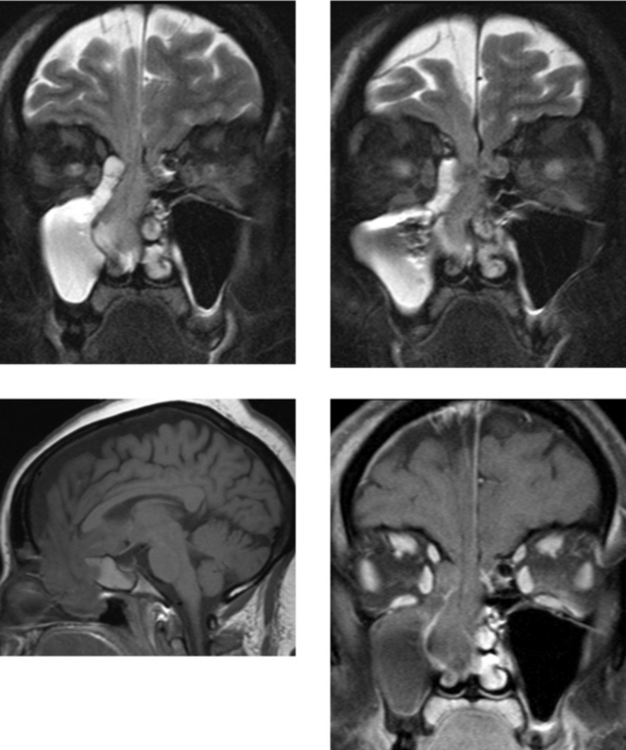
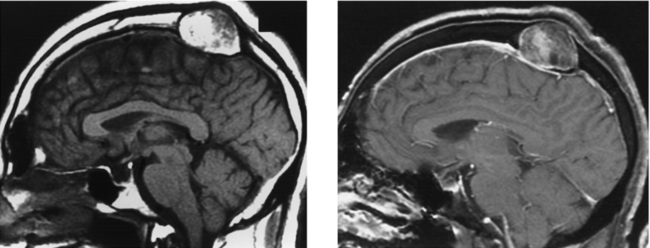
CASE 93 Craniopharyngioma—Recurrent Adamantinomatous Type
Nagahata M, Hosoya T, Kayama T, Yamaguchi K. Edema along the optic tract: a useful MR finding for the diagnosis of craniopharyngiomas. AJNR Am J Neuroradiol. 1998;19:1753-1757.
Sartoretti-Schefer S, Wichmann W, Aguzzi A, Valavanis A. MR differentiation of adamantinous and squamous-papillary craniopharyngiomas. AJNR Am J Neuroradiol. 1997;18:77-87.
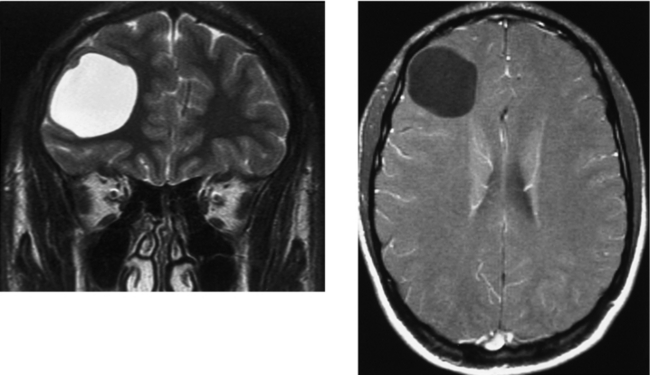
CASE 95 Porencephalic Cyst