17 Failure to Thrive
Etiology and Pathogenesis
Nonorganic Factors
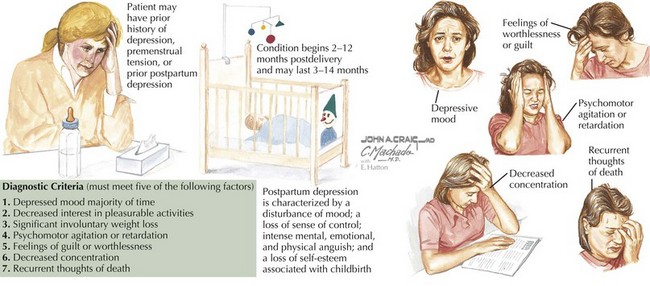
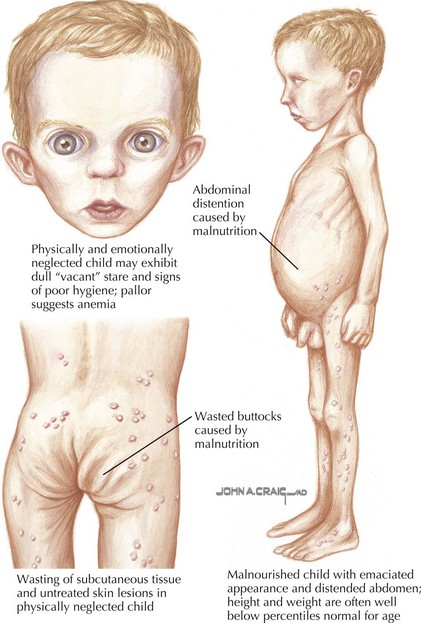
Even if a family is food secure, stressors associated with poverty can cause attachment problems, leading to difficulty in feeding for susceptible children. Families living in shelters or with many family members may have little control over when and where children are fed. Children whose temperaments and appetites require more routine or more frequent meals sometimes fail to thrive in these settings. Domestic violence can be associated with FTT through its detrimental effects on the caregiver, child, or both. Caregiver mental or physical illness, including postpartum depression (Figure 17-1), can also lead to disturbances of attachment. Children who are failing to thrive are at increased risk for abuse and neglect compared with the general population, but most experts believe that the majority of children with FTT are not abused or neglected (Figure 17-2). Some children in stressful living environments appear to have problems absorbing and using calories for growth because they grow poorly despite apparently adequate caloric intake and lack of organic causes for growth failure.
Clinical Presentation
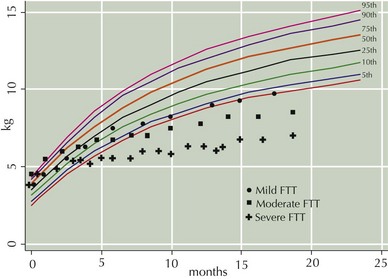
Patients may present throughout infancy and early childhood, although most cases of FTT start in the first year of life. Weight is generally affected earlier and more severely than length. Psychosocial dwarfism is a distinct problem that occurs in patients older than 3 years of age and primarily affects height. Waterlow’s categorization of FTT as mild, moderate, and severe is determined by comparing a child’s growth parameters with the median values for the child’s age and height. Growth patterns demonstrating each of the three classes of FTT are shown in Figure 17-3.
Differential Diagnosis
The differential diagnosis for FTT is broad and often multifactorial. As already noted, many psychosocial stressors and many chronic medical conditions could contribute to FTT. A list of some conditions to consider in the differential diagnosis is presented in Box 17-1.
* In persistent FTT, these conditions should be considered even in the absence of signs or symptoms.
Evaluation and Management
Evaluation
Organic Causes of Failure to Thrive
Most organic causes of FTT can be detected through thorough histories and physical examinations without laboratory evaluation. The history should include a birth history and birth growth parameters as well as family history, including parental height. Symptoms such as diarrhea, vomiting, respiratory problems, or abnormalities on physical examination should prompt further evaluation. Subtle signs such as atopy may suggest possible food allergies and snoring or mouth breathing may be associated with obstructive sleep apnea. Recurrent infections may be a sign of an immune deficiency and should be evaluated further, but they may also be a sign of the decreased effectiveness of the immune system in a malnourished child. Some conditions can cause or contribute to FTT without apparent signs or symptoms, and if children have no apparent cause for FTT and are not adequately responding to treatment, consideration should be given to testing for those conditions listed in Box 17-1: HIV infection, cystic fibrosis, celiac disease, Giardia and urinary tract infections, and renal tubular acidosis, all of which may cause FTT without other symptoms.
Black MM, Dubowitz H, Krishnakumar A, et al. Early intervention and recovery among children with failure to thrive: follow-up at age 8. Pediatrics. 2007;120(1):59-69.
Failure to thrive. In: Kleinman R, editor. Pediatric Nutrition Handbook. ed 6. Elk Grove, IL: American Academy of Pediatrics; 2009:601-636.
Radimer KL, Olson CM, Green JC, et al. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ. 1992;24(suppl):36S-45S.
Zenel JAJr. Failure to thrive: a general pediatrician’s perspective. Pediatr Rev. 1997;18(11):371-378.