CHAPTER 24 Failure Modes of Unicompartmental Arthroplasty
 Unicompartmental arthroplasty is a common surgical procedure in the patient with unicompartmental disease.
Unicompartmental arthroplasty is a common surgical procedure in the patient with unicompartmental disease.Introduction
Unicompartmental knee arthroplasty (UKA) has become a common surgical procedure for unicompartmental osteoarthritis both nationally and internationally in the middle-aged and older patient. Midterm and long-term survivorship of UKA is highly variable. From 1998 to 2005, the incidence of performance of UKA increased at a rate of 32.5% compared to an increase in the performance of total knee arthroplasty of 9.4% during the same period.1 In the past 30 years, multiple authors have reported on the indications and contraindications for UKA.2–23
Indications
The classic indications for UKA include:
The “one-finger test” has been reported as a useful indicator as to the location of the pain correlative with the patient’s radiographs exhibiting single-compartment osteoarthritis.3
Contraindications
Contraindications have included:
Operating on patients who exhibit contraindications can result in reduced survivorship of UKA.2,3
Etiology of Failures
Furthermore, failures of UKA can occur as a result of:
Some designs that are no longer utilized exhibited exceedingly high failure rates as a result of component design and polyethylene failure.24,25 Furthermore, using all-polyethylene tibial (APT) components in elderly patients with increased posterior tibial slope and removal of significant amounts of tibial bone have resulted in increased medial tibial collapse with subsidence of the tibial component in some patients.26 Despite recent articles indicating that metal backing reduces strains across the cement-bone interface,27 the longest published survivorship has utilized APT components with specific undersurface macrostructure on both the inferior portion of the APT component and its eccentric post. However, it has been emphasized that minimal tibial bone was removed in those cases that exhibited the longest survivorship.19,28
 The Importance of Surgical Technique (see Video 24-1)
The Importance of Surgical Technique (see Video 24-1)
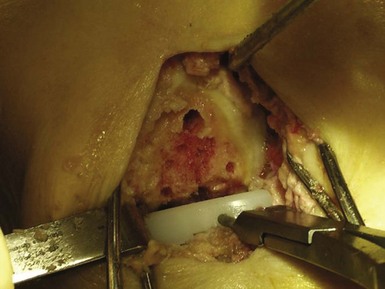
Surgical technique is critical when performing UKA, and accounts for failures regardless of the prosthesis utilized. Surgical recommendations include lateralization of the femoral component when doing medial UKA to account for external rotation during extension of the knee (Fig. 24–1). When using an all-polyethylene component, it is important to implant the widest tibial component possible from the medial tibial cortex to the anterior cruciate ligament, resting on the medial tibial cortex (Fig. 24–2). Using a Steinmann pin through the intercondylar notch to retract the patella and facilitate exposure is helpful. Appropriate cement technique is critical and involves drilling, using pulse lavage, and drying the surfaces prior to applying the cement (Fig. 24–3). The cement should be applied in its doughy stage as well.29 This allows for improved fixation of both the femoral and tibial components.30 When choosing APT components, laboratory studies have confirmed that a dovetail undersurface macrostructure of the tibial component provides the greatest resistance to lift-off and shear stresses (Fig. 24–4). Waffle undersurface patterns tend to result in the worst resistance to lift-off and shear stress application.31,32
Complications of Surgical Technique
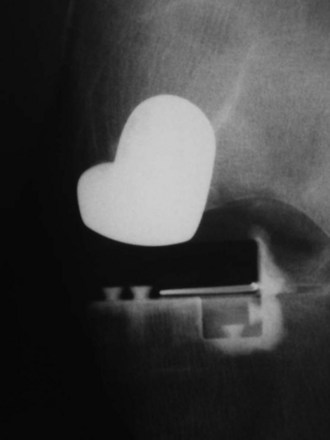
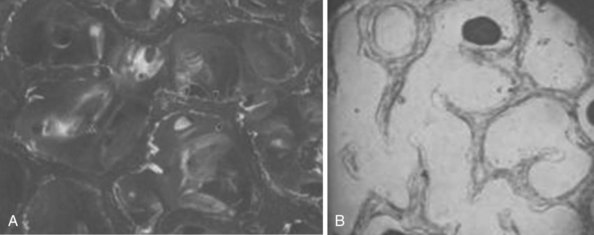
It is critical to avoid removal of too much tibial bone in order to prevent fracture and/or subsidence of the tibial component. Fractures have been reported (Figs. 24–5 and 24–6) through the tibial pin sites, resulting in difficult revision scenarios.33–35 Early medial collapse has been reported with significant medial bone removal, and an 11% rate of subsidence of the medially placed APT components has been reported with 2.5-year follow-ups. Upon radiographic review of these patients, the tibial component lacked peripheral support and there was significant bone removal.26 As originally reported by Bloebaum et al.,36 the majority of the proximal tibia, when resecting approximately 6–11 mm below the articular surface, is highly porous cancellous bone consisting predominantly of air. When viewing these resected specimens through the electron microscope, it is apparent that up to 80% of the proximal tibia is cancellous bone at these levels, as demonstrated by polarized (Fig. 24–7A) and nonpolarized (Fig. 24–7B) electron microscopic views of the proximal tibia.36 Furthermore, the posteromedial and posterolateral aspects of the resected proximal tibia have up to 20% more bone than the remainder of the articular surface. This observation would clearly explain why fixation can be an issue and subsidence may occur, especially anteromedially and anterolaterally, if too much tibial bone is resected or an undersized tibial component is placed without medial tibial cortex contact and support.
Malalignment
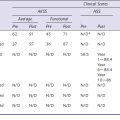
Alignment is critical to the success of UKA. Squire et al. originally reported this concept in 1999 when they noted in a series of UKA patients that 46% had loss of lateral joint space postoperatively.37 The etiology of lateral compartment wear subsequent to medial UKA is usually secondary to overcorrecting preoperative varus alignment and placing the patient into postoperative valgus (Fig. 24–8). In one consecutive series of 100 patients,16 83% developed progressive lateral joint space collapse due to progressive wear of the lateral compartment (Fig. 24–9). Berger et al.,23 however, noted that only 18% developed progressive joint space collapse subsequent to UKA when these patients were placed in neutral to slight mechanical varus (Fig. 24–10). Biopsies of the pristine surface of the lateral compartment in “normal”-appearing lateral compartment chondral surfaces has confirmed early changes of osteoarthritis histologically, indicating that preexistent degenerative arthritis may be present in asymptomatic knee compartments.38 Medial-lateral mismatch can occur due to inappropriate placement of the components in the sagittal plane on the medial femoral condyle or the tibial plateau. In addition, sizing of the femur and tibia is important as well since the tibial component should rest on the medial tibial cortex to avoid subsidence, which is a common failure modality if too much tibial bone is removed or the tibial component is undersized. Lateral positioning of the femoral component onto the medial femoral condyle is helpful to avoid medial-lateral mismatch.3,25,26 Older prosthetic designs more commonly resulted in articular surface mismatch due to attempts at matching surface geometry configurations of the femoral and tibial components (Fig. 24–11).
Failure of Fixation
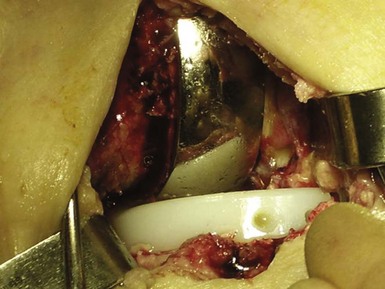
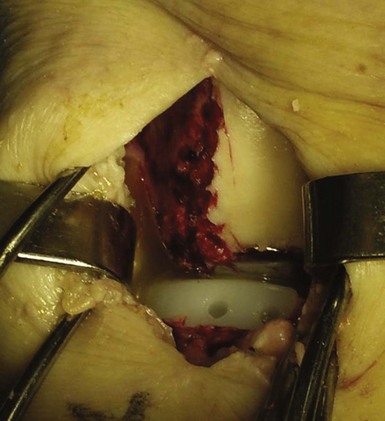
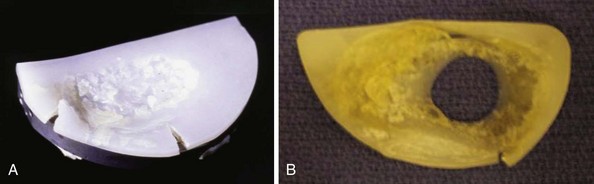
Failure of fixation is most commonly due to cement technique and/or component design (Fig. 24–12). Polyethylene wear with premature failure of the tibial insert was more common previously due to the usage of thin polyethylene inserts (Fig. 24–13) and sterilization issues resulting in delamination and early wear of the polyethylene tibial insert.25 Cement removal can be compromised due to a mini-incision exposure resulting in cement retained posterior to the APT component. When implanting the tibial component, a “snowplow effect” (Fig. 24–14A) can occur resulting in “heaping up” of bone posteriorly (Fig. 24–14B and 14C), which can eventually fracture and result in loose body formation.39 It is important to use a small curved curette or similar instrument to remove cement posteriorly when implanting the APT component.
Inappropriate Patient Selection
Inappropriate patient selection includes choosing patients with more than single-compartment disease and/or global knee pain.3 Controversy exists, however, as to the amount of preexistent patellofemoral arthritis that can be ignored at the time of unicompartmental arthroplasty. Some authors argue that there is no contraindication to preexistent patellofemoral disease unless there is bone loss and lateral facet grooving.40 Extremely active patients are a concern when performing this procedure since loosening and premature wear is possible. Obesity has been implicated as a failure mechanism in UKA. As was noted by Behrend et al. in 2005, when other factors were excluded, obesity was a major causative factor in midterm and long-term survivorship of UKA.41 In a retrospective review of 921 UKAs in the Healtheast Total Joint Registry,18 a statistical analysis to compare cumulative revision rates using the Wilcoxon rank-sum test, Kaplan-Meier survival analysis, the log rank test, and the Cox proportional hazards regression test was performed. The average follow-up was 7.2 years with a range of 2 to 14 years. Obesity was defined as a body mass index (BMI) greater than 30. The results of this review confirmed no increased risk of revision for overweight or obese patients when compared to normal-BMI patients after adjustment for age and year of index procedure.42
1 Riddle D, Jiranek W, McGlynn F. Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty. 2008;23:408-412.
2 Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg. 2008;16:9-18.
3 Bert J. Unicompartmental knee replacement. Orthop Clin North Am. 2005;36:513-522.
4 Skolnick M, Coventry M, Ilstrup D. Geometric total knee arthroplasty: a two year follow-up. J Bone Joint Surg [Am]. 1976;58:749-753.
5 Skolnick M, Peterson L, Combs J. Polycentric knee arthroplasty—a two year follow-up. J Bone Joint Surg [Am]. 1975;57:1033-1038.
6 Bae D, Guhl J, Keane S, Unicompartmental knee arthroplasty for single compartment disease: clinical experience with an average 4 year follow-up study. Clin Orthop Relat Res, 176, 1983, 233-238.
7 Laskin R. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg [Am]. 1978;60:182-185.
8 Cameron H, Hunter G, Welsh R, et al, Unicompartmental knee replacement. Clin Orthop Relat Res, 160, 1981, 109-113.
9 Insall J, Aglietti P. A 5 to 7 year follow up of unicondylar arthroplasty. J Bone Joint Surg [Am]. 1980;62:1329-1337.
10 Marmor L, The modular knee. Clin Orthop Relat Res, 94, 1973, 242-248.
11 Marmor L, Unicompartmental arthroplasty of the knee with a minimum of 10 year followup. Clin Orthop Relat Res, 228, 1988, 171-177.
12 Scott R, Cobb A, Ewald P, et al, Unicompartmental knee arthroplasty: 8 to 12 year follow-up with survivorship analysis. Clin Orthop Relat Res, 271, 1991, 96-100.
13 Heck D, Marmor L, Gibson A, et al, Unicompartmental knee arthroplasty: a multicenter investigation with long term follow-up evaluation. Clin Orthop Relat Res, 286, 1993, 154-159.
14 Cartier A, Kozinn S, Scott R. Unicompartmental knee arthroplasty surgery. J Arthroplasty. 1996;11:782-786.
15 Grelsamer RP. Unicompartmental osteoarthritis of the knee. J Bone Joint Surg [Am]. 1995;77:278-292.
16 Bert J. Ten year survivorship of metal backed unicompartmental arthroplasty. J Arthroplasty. 1998;13:901-905.
17 Svärd UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of independent series. J Bone Joint Surg [Br]. 2001;83:191-194.
18 Gioe T, Bert J, Killeen K, et al, Analysis of unicompartmental arthroplasty in a community based implant registry. Clin Orthop Relat Res, 416, 2003, 111-119.
19 Steele R, Hutabarat S, Evans R, et al. Survivorship of the St. Georg Sled medial unicompartmental knee replacement beyond 10 years. J Bone Joint Surg [Br]. 2006;88:1164-1172.
20 Repicci J. Benefits and limitations of the unicondylar knee prosthesis. J Orthop. 2003;26:274-279.
21 Sah A, Springer B, Scott R, Unicompartmental knee arthroplasty in octogenerians: survival longer than the patient. Clin Orthop Relat Res, 451, 2006, 107-112.
22 O’Rourke M, Gardner J, Callaghan J, et al, The John Insall Award. Unicompartmental knee replacement: a minimum 21 year follow-up, end results study. Clin Orthop Relat Res, 440, 2005, 27-34.
23 Berger R, Meneghini R, Jacobs J, et al. Results of unicompartmental knee arthroplasy at a minimun of ten years of follow-up. J Bone Joint Surg [Am]. 2005;87:999-1004.
24 Hamilton W, Collier M, Tarabee E. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):98-107.
25 Bert J, Smith R. Failures of metal-backed unicompartmental arthroplasty. Knee. 1997;4:41-48.
26 Aleto TJ, Berend ME, Ritter MA, et al. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23:159-163.
27 Small S, Behrend M, Ritter M, et al. Metal backing significantly decreases tibial strains in unicompartmental knee arthroplasty. Manuscript submitted for publication, January 2010.
28 Newman J, Pydisetty R, Ackroyd C. Unicompartmental or total knee replacement: the results of a prospective randomized controlled trial. J Bone Joint Surg [Br]. 2009;91:52-57.
29 Bert J. Unicompartmental arthroplasty for unicompartmental knee arthritis. Tech Knee Surg. 2007;6(4):1-10.
30 Bert J, McShane M, Is it necessary to cement the tibial stem in cemented total knee arthroplasty?. Clin Orthop Relat Res, 356, 1998, 73-78.
31 Bert J, Koeneman J. A comparison of the mechanical stability of various unicompartmental tibial componenents. J Orthop Arthroplasty Rounds. 1994;17:559-564.
32 Rosa RA, Bert JM, Bruce W, et al. An evaluation of all-ultra-high molecular weight polyethylene unicompartmental tibial component cement fixation mechanisms. J Bone Joint Surg [Am]. 2002;84(Suppl 2):102-104.
33 Yang KY, Yeo SJ, Lo NN. Stress fracture of the medial tibial plateau after minimally invasive unicompartmental knee arthroplasty: a report of 2 cases. J Arthroplasty. 2003;18:801-803.
34 Brumby S, Carrington R, Zayontz S, et al. Tibial plateau stress fracture: a complication of unicompartmental knee arthroplasty using 4 guide pinholes. J Arthroplasty. 2003;18:809-812.
35 Song M, Kim B, Seong J, et al. Early complications after minimally invasive mobile-bearing unicompartmental arthroplasty. J Arthroplasty. 2009;24:1281-1284.
36 Bloebaum R, Bachus K, Mitchell W, et al, Analysis of the bone surface area in resected tibia. Clin Orthop Relat Res, 309, 1994, 2-10.
37 Squire M, Callaghan J, Goetz D, et al, Unicompartmental knee replacement: a minimum 15 year followup study. Clin Orthop Relat Res, 367, 1999, 61-72.
38 Bert J. Histologic appearance of pristine articular cartilage in knees with unicompartmental osteoarthritis. J Knee Surg. 2007;20:15-20.
39 Hamilton W, et al. Incidence and causes of reoperation after minimally invasive unicompartmental knee arthroplasty. Presented at the AAOS 73rd Annual Meeting, Chicago, IL, March 22–24, 2006.
40 Beard DJ, Pandit H, Ostlere S, et al. Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]. 2007;89:1602-1607.
41 Behrend K, Lombardi A, Mallory T, et al, Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin Orthop Relat Res, 440, 2005, 60-66.
42 Bert J, Tatman P, Mehle S, Killeen K. The effect of body mass index on survivorship of unicompartmental knee arthroplasty. Manuscript submitted for publication, February 2010.