Chapter 19 FAECAL INCONTINENCE
PREVALENCE
The reported prevalence rates of faecal incontinence in the world vary from 0.7%–11%, depending on the definition and population group studied. This is demonstrated in Table 19.1.
TABLE 19.1 International prevalence rates of faecal incontinence
| Country | Population | Prevalence |
|---|---|---|
| Holland | Women >60 y | 4.2% to 16.9% with rising age |
| France | All >45 y | 11%, 6% to faeces, 60% women |
| UK | Community service | 1.9% |
| USA | Market mailing | 7% soiling, 0.7% to faeces |
| USA | Wisconsin households | 2.2%, 63% women |
| USA | Wisconsin nursing homes | 47% |
| New Zealand | >65 y | 3.1% |
| Australia | Household survey | 6.8% men |
| 10.9% women >15 y | ||
| Australia | Postal survey | Liquid incontinence 9% |
| Random selection from electoral roll (subjects ≥18 y) | Solid incontinence 2% |
Based on Continence Foundation of Australia. Incontinence: some key statistics and quotes clarified. Online.
Available: www.contfound.org.au/pdf/Keystatsquotsmay03.pdf.
AETIOLOGY
Table 19.2 lists the possible causes of faecal incontinence. Looser stool consistency is an important precipitating factor in those predisposed to faecal incontenance by anorectal abnormalities.
TABLE 19.2 Classification of the aetiology of faecal incontinence
| Altered stool consistency—diarrhoeal states |
Previous operations
Haemorrhoidectomy
With current surgical techniques for haemorrhoids, incontinence is a rare complication. However, if the anal sphincter is inadvertently divided, incontinence may result. With the use of a stapled haemorrhoidectomy, there is also a small risk of anal incontinence secondary to dilatation by the instrument. However, this form of incontinence usually resolves with time.
Trauma
Traumatic injury to sphincters may occur during an accident. Serious forms of injury may require a temporary stoma. The anal sphincter is then re-assessed and appropriately treated prior to closure of the stoma at a later stage.
HISTORY
A detailed history is absolutely necessary in the assessment of any pathological condition, paying particular attention to the characteristic cause and extent of the incontinence. It is important to determine the nature of incontinence—whether it is incontinence to solid, liquid or flatus—and to determine the frequency of the incontinence and the necessity to wear a protective pad. Other associated symptoms such as urgency need to be determined as well as social limitation as a result of the incontinence.
There are many continence scoring systems available in the literature. Most of them are useful for research purposes but are not practical for day-to-day use. The St Mark’s scoring system is listed in Table 19.3. A clue to the severity of incontinence is determining the frequency of the incontinence, the necessity to wear a protective pad and the effect on social function.
| Symptom severity | Score |
| Incontinence to solid stool | |
| Never | 0 |
| Less than once per month | 1 |
| Less than once per week | 2 |
| Most days | 3 |
| Incontinence to liquid stool | |
| Never | 0 |
| Less than once per month | 1 |
| Less than once per week | 2 |
| Most days | 3 |
| Incontinence to flatus | |
| Never | 0 |
| Less than once per month | 1 |
| Less than once per week | 2 |
| Most days | 3 |
| Ability to withhold defecation more than 15 min | |
| Yes | 0 |
| No | 1 |
0 = fully continent; 13 = regularly completely incontinent to all rectal contents.
PHYSICAL EXAMINATION
INVESTIGATIONS
TREATMENT
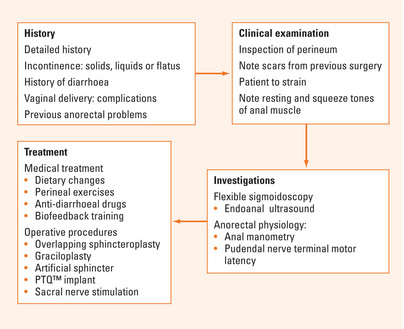
Treatment of incontinence involves non-operative and operative procedures (see Figure 19.1).
Operative procedures
Overlapping sphincteroplasty
This operation is indicated for patients with a definite sphincter defect. The operation involves dividing the scar tissue and overlapping the sphincter complex (internal and external anal sphincters). The short-term results are good in about 80%–90% of patients. However, the results are not as good on long-term follow-up.
Postanal repair
This operation is now seldom performed and its success rate is said to be about 50%.
Sacral nerve stimulation
This operation is indicated for patients who fail conservative management of faecal incontinence. It is divided into two stages. The first stage involves testing the effect of stimulating the pelvic nerve—mainly S3. This is performed via insertion of lead wires into the S3 foramen to stimulate the S3 nerve. The wire is then connected to an external temporary pacemaker. The patient carries the pacemaker around for 7–10 days during this trial period to see whether the stimulation improves their continence. If continence does not improve over the trial period, the wires are then removed. If the continence improves, a permanent pacemaker is then inserted under the skin in either the buttock or the anterior abdominal wall. This stimulation of nerve leads to increase of anal tone and therefore improves continence. The result from the operation showed that 85% of patients have significant improvement—85% of patients have more than 50% reduction in incontinent episodes.
SUMMARY
A detailed history and clinical examination is important with special emphasis on vaginal delivery and any complications (Figure 19.1). On per rectum examination, assess resting tone and squeeze tone. Investigations include flexible sigmoidoscopy, which is mandatory, endoanal ultrasound, anal manometry and pudendal nerve terminal motor latency.
Kalantar JS, Howell S, Talley NJ. Prevalence of faecal incontinence and associated risk factors; an underdiagnosed problem in the Australian community? Med J Aust. 2002;176(2):47-48.
Madoff RD, Parker SC, Varma MG, et al. Faecal incontinence in adults. Lancet. 2004;364:621-632.
Norton C. Behavioral management of fecal incontinence in adults. Gastroenterology. 2004;126(1 Suppl 1):S64-S70.
Rao SS. Pathophysiology of adult fecal incontinence. Gastroenterology. 2004;126(1 Suppl 1):S14-S22.
Wald A. Clinical practice. Fecal incontinence in adults. N Engl J Med. 2007;356:1648-1655.