CHAPTER 5 Factors Influencing the Outcome of Distal Radius Fractures
The anatomical results of fracture treatment have no meaning unless they are considered in light of the functional outcome.1 Myriad factors affect the clinical result after a distal radius fracture. Most of these predictions are based on the radiographic findings, although the surrounding soft tissue envelope and the intracarpal ligaments have a marked influence. It is useful to identify the variables that have some predictive value regarding the ultimate result to maximize the chances of a favorable outcome.
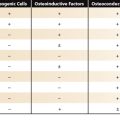
Anatomical Predictors of Fracture Instability
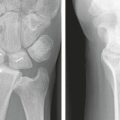
Fracture instability may be defined as an inability to resist displacement after an anatomical reduction. The standard radiographic parameters of the distal radius include a radial inclination of 23 degrees (range 13 to 30 degrees), a radial length of 12 mm (range 8 to 18 mm), and an average volar tilt of 12 degrees (1 to 21 degrees).2–5 There are difficulties in reliably predicting fracture instability based on radiographs alone. Algorithms have been developed to gauge the risk of redisplacement of a fracture after reduction, but to no avail. Two separate scoring systems have been devised to calculate this risk based on the initial injury films. In a prospective study of 80 patients, both scoring systems were found to underestimate the degree of fracture instability and to have a poor correlation with the predicted and the actual instability.6
In a now classic article, Lafontaine and colleagues7 identified numerous risk factors that were associated with redisplacement of a distal radius fracture despite an initial satisfactory reduction. These included the presence of dorsal tilt greater than 20 degrees, comminution, intra-articular involvement, an associated fracture of the ulna, and age older than 60 years. If three or more of these factors were present, there was a high likelihood of fracture collapse. Altissimi and coworkers8 noted that the severity of the initial radial shortening alone seemed to be a reliable indicator of late instability.
Advanced age influences fracture instability because of the associated osteopenia. In patients older than 60 years, Leone and coworkers9 found that the degree of radial shortening, volar tilt, the amount of dorsal comminution, and advanced age were predictive of early or late failure. An unexpected finding was that one third of undisplaced fractures occurred in patients older than 65 years. Abbaszadegan and colleagues10 determined that age was the only statistically significant predictor of secondary displacement. After obtaining an acceptable initial closed reduction, patients who were older than 60 years had four times the risk for 4-week failure over patients younger than 60 years. The risk for displacement increased as age increased.
One can surmise from these observations that there is a higher likelihood of secondary fracture collapse in elderly patients even with less initial displacement. In this age group, Dicpinigaitis and associates11 found that fracture site settling may occur for up to 6 months. Because of the risk of late collapse, adjuvant internal fixation with locking plates should be considered in elderly and osteopenic patients.
Greater force is necessary to fracture the radius in younger patients because of their higher bone density, which can result in more comminution and a higher risk of subsequent fracture collapse.12 In young patients, lesser degrees of fracture site displacement can be tolerated, so adjuvant external or internal fixation should be considered. Trumble and coworkers13,14 recommend internal fixation if there is more than 2 mm of radial shortening and more than 15 degrees of dorsal tilt after a closed reduction, if there is comminution of more than two cortices, or if there is a displaced intra-articular component.
Anatomical Predictors of Osteoarthritis
Articular congruity is paramount in the development of post-traumatic osteoarthritis. In a classic article, Knirk and Jupiter15 retrospectively reviewed 43 intra-articular fractures in 40 young adults (mean age 27.6 years) that were treated at Massachusetts General Hospital, with a mean follow-up of 6.7 years. Because most of the fractures (38 of 43) were treated with older, nonrigid fixation methods that were popular at that time, including cast or pins and plaster, there was a high incidence of residual intra-articular incongruity. Knirk and Jupiter15 noted that radiographic evidence of arthritis was present in 8 of 8 of the fractures in which articular incongruity was 2 mm or more, in contrast to only 2 of 19 of the fractures that healed with a congruous joint. Osteoarthritis was found in 22 of 24 of the patients who had any step-off whatsoever.15
In their study of 59 patients, Altissimi and coworkers16 found a 31% incidence of osteoarthritis when there was 2 mm or more of articular step-off at the 3.5-year follow-up. Catalano and colleagues17 studied 21 patients younger than 45 years old who had undergone internal fixation of displaced intra-articular fractures. At an average of 7.1 years, osteoarthrosis of the radiocarpal joint was radiographically apparent in 16 wrists (76%). A strong association was found between the development of osteoarthrosis of the radiocarpal joint and residual displacement of articular fragments at the time of bony union (P < .01). The authors revisited 16 of these patients at 15 years. Arthrosis was present in 13 of 16 of the wrists, and there was an additional 67% reduction of the joint space.18 Even 1 mm of intra-articular congruence has been associated with the development of arthrosis.19
Predictors of Residual Impairment
Radiographic Predictors
The landmark article by Gartland and Werley20 was instrumental in establishing the link between the anatomical restoration of a distal radius fracture and the functional outcome. This finding has been corroborated by many studies since then. Aro and Koivunen21 looked at the outcomes in 92 patients older than 55 years. They noted that even minor axial shortening of the radius after a Colles’ fracture affected the outcome. The functional end result was unsatisfactory in 4% of the patients with an acceptable anatomical result, in 25% of the patients with radial shortening of 3 to 5 mm, and in 31% of the patients with shortening of more than 5 mm. Fujii and associates22 also determined that radial shortening of 6 mm or more was associated with a poor functional outcome. Combined deformities also are significant. Axial compression of more than 2 mm and dorsal angulation of more than 15 degrees adversely affect the end results.13 Radiographic evidence of carpal instability also has been shown to correlate with poor functional results.23
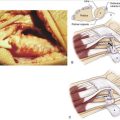
Intracarpal Lesions
Arthroscopic evaluation of extra-articular and intra-articular distal radius fractures has revealed that triangular fibrocartilage and interosseous ligament tears are much more common than previously suspected. Several authors have examined the incidence of intracarpal soft tissue injuries associated with distal radius fractures. Geissler and colleagues24 studied 60 patients and found a triangular fibrocartilage complex injury in 26 (43%). In the series by Lindau and associates25 of 51 patients, 43 (84%) had a triangular fibrocartilage complex injury: 24 had a peripheral tear, 10 had a central perforation, and 9 had a combined central and peripheral tear. In the series by Richards and colleagues26 of 118 patients, triangular fibrocartilage complex injury occurred in 35% of the intra-articular fractures and 53% of the extra-articular fractures. They noted, however, that the preoperative radiographs had no predictive value for assessing interosseous ligament injury. Unrecognized chondral and ligamentous lesions may explain poor outcomes after seemingly well-healed fractures in young adults.25
Post-traumatic Osteoarthritis
Experimental work on displaced intra-articular distal radius fractures has measured significant changes in mean contact stresses with step-offs of only 1 mm.27 Pain has been significantly related to the size of the intra-articular step.28 These findings have prompted some authors to recommend surgical treatment for residual articular incongruity of more than 1 mm.13,29
Ulnar Wrist Pain
One study of 109 Colles’ fractures treated with closed reduction and casting determined that the most important factor for predicting ulnar wrist pain was incongruity of the distal radioulnar joint as a result of residual dorsal angulation of the radius.30 Other studies have found that an increase in the ulnar variance was the most important radiological parameter affecting outcome.31 Ulnocarpal impingement and distal radioulnar joint incongruency are related to the amount of radial shortening and are a common cause of ulnar-sided wrist pain.32 In young patients, distal radioulnar joint instability is another cause for residual pain after a distal radius fracture. Lindau and coworkers33 could not correlate this instability with any specific radiographic parameter, however.
Grip Strength Loss
More than 10 degrees of dorsal tilt leads to a dorsal carpal shift with compressive forces, which causes pain and insecurity with gripping. This condition has been associated with increased difficulty with everyday activities and work.34 Dorsal angulation of more than 20 degrees and a reduction of the radial angle to less than 10 degrees can result in a reduction in grip strength.35
Work-Related Injury
Injury compensation is a predictive factor with regard to patient-reported pain and disability. In a prospective study of 120 patients sustaining a distal radius fracture, the most influential predictor of pain and disability at 6 months was injury compensation. Wrist impairment was moderately correlated with patient-reported pain and disability.36 Fernandez and colleagues19 found that patients with work-related injuries were more than four times less likely to return to work than patients injured outside of work.
Predictors of Loss of Wrist Motion
Experimentally, dorsal tilt of up to 30 degrees and radial translation of up to 10 mm leads to no significant restriction in forearm pronation or supination. Radial shortening of 10 mm reduces forearm pronation by 47% and supination by 29%. Five millimeters of ulnar translation deformity results in a mean 23% loss of pronation.37 Clinical experience has shown that axial compression of more than 2 mm and dorsal angulation exceeding 15 degrees were directly related to diminished range of motion.38
Comminution and intra-articular involvement also predispose toward a loss of movement.35 In a study of 169 distal radius fractures in adults younger than 50 years, fracture union with a step in the radiocarpal articular surface was associated with loss of wrist mobility and difficulty with fine dexterous tasks.34 The predictive value of this evidence is that if a loss of motion is due to bony malalignment, prolonged therapy would be of no benefit.
Predictors of Patient Satisfaction
Wrist Pain and Grip Strength
A total of 53 items were evaluated by a group of 55 patients recovering from a fracture of the distal radius, which established the prevalence, mean severity score, and overall severity score (or impact) of each item as it related to physical function and social and emotional impact. The amount of residual wrist pain influenced patient satisfaction more than motion. Hand dominance also was a significant factor.39
Trumble and colleagues14 devised a combined injury score rating system that included grip strength, range of motion, and pain relief to score the results after internal fixation of displaced intra-articular distal radius fractures. In this retrospective study, 43 patients were evaluated at a mean of 38 months. Patient satisfaction seemed to correlate best with pain relief and grip strength, rather than the postoperative loss of palmar tilt or radial tilt. Preoperative step-off and gap and radial shortening were equated with worse outcomes.14
In other clinical trials, Fujii and associates22 noted that the grip power was the most significant factor related to subjective evaluation. A prospective study of 31 patients recovering from unstable fractures of the distal radius investigated the association between objective variables and the level of post-traumatic disability of the wrist as measured by the patient-rated wrist evaluation (PRWE) score. Grip strength was shown to be a significant predictor of the PRWE score and seemed to be a sensitive indicator of return of wrist function.40
Osteoporosis
A study of the bone mineral densitometry in women older than 40 years who sustained a distal radius fracture showed that the clinical results correlated better with bone mineral density than with the radiological parameters.41 The gist of this observation is that although surgeons continue to strive for perfection, some degree of malalignment seems to be well tolerated. Patient satisfaction often hinges on pain relief and return of grip strength over anatomical restoration. This observation was affirmed by one prospective study of 85 patients who were randomly assigned to either bridging external fixation or plaster immobilization for treatment of a Colles’ type distal radius fracture. Despite a high level of radiographic malunion (50%), overall function, range of movement, and activities of daily living were not limited.42 Involvement of the dominant hand and osteopenia may compromise the end result.
Factors That Are Not Invariably Predictive
Acceptable Reduction
The relationship between form and function is not invariable. Acceptable radiographic reduction of dorsal/volar tilt criteria was not associated with better self-reported functional outcomes or increased satisfaction at 6 months in elderly patients with conservatively treated distal radius fractures.43 A retrospective study of Colles’ fractures in patients 60 years or older revealed an 82% incidence (11 patients) of a good to excellent outcome in undisplaced fractures compared with a 68% incidence (25 patients) in redisplaced fractures.44
Malunion
In the evaluation of the outcomes using the Short-Form 36 survey, a study of 50 patients (mean age 49.6 years) found no correlation with residual radial height, radial tilt, or palmar tilt after internal or external fixation of distal radius fractures. Intra-articular incongruence of 1 mm or greater did correlate with a lower score, however.19
Gliatis and colleagues34 assessed the outcome of 169 fractures of the distal radius in adults younger than 50 years at a mean follow-up of 4.9 years. No measure of either intra-articular or extra-articular malunion influenced the severity or frequency of persistent wrist pain.
Dayican and coworkers45 investigated the results of 108 patients older than 70 years with intra-articular distal radial fractures who would not consent to an operation. At a mean follow-up of 39.5 months, 88.9% were considered to have good and excellent functional results even though 25.9% of the patients had fair and poor anatomical scores.45
In another study, 85 patients with displaced Colles’ fractures were reviewed 10 years after the injury. Initial and 10-year radial shortening and early finger stiffness significantly correlated with final outcome. Dorsal angulation influenced early, but not 10-year, function. Sixty-two percent of patients with an unsatisfactory result had objective features of reflex sympathetic dystrophy compared with only 6% of patients with a satisfactory result.46
A more recent article clarifies this point further. Grewal and MacDermid47 prospectively followed 216 patients with extra-articular distal radius fractures for 1 year and assessed the patient-reported outcomes using the Disabilities of the Arm, Shoulder, and Hand (DASH) score and PRWE. The overall alignment of the distal radius fracture was designated as “unacceptable” if the dorsal angulation was greater than 10 degrees, if the radial inclination was less than 15 degrees, or if there was 3 mm or more of ulnar-positive variance. Patients younger than 65 years showed a very strong link between poor outcomes and the presence of malalignment of the distal radius. Patients 65 years and older showed no significant relationship between malalignment of the distal radius and patient reports of pain and disability. Based on relative risk, malalignment increased the risk of having a poor outcome (DASH > 20 or PRWE > 20) in all age groups. Using the DASH score, patients older than 65 years experience one bad outcome for every eight patients who present with unacceptable alignment. This finding contrasts with younger patients, in whom one in two (based on the DASH) or one in three (based on the PRWE) experience a poor outcome if left with a malaligned distal radius fracture.47
Osteoarthritis
The radiographic presence of osteoarthritis does not always adversely affect the functional outcome.42 In a series of 21 patients with surgically treated intra-articular fractures, osteoarthrosis of the radiocarpal joint was radiographically apparent in 16 (76%) of the wrists at an average follow-up of 7.1 years. The functional status did not correlate, however, with the magnitude of the residual step and gap displacement at the time of fracture healing. All patients had a good or excellent functional outcome regardless of radiographic evidence of osteoarthrosis of the radiocarpal or distal radioulnar joint.17
Summary
Myriad factors determine the outcome after a distal radius fracture, including anatomical alignment, age, motion, pain, and hand dominance. Elderly patients may tolerate greater degrees of residual deformity because of lower functional demands. Unrecognized intracarpal pathology may account for poor functional results despite acceptable radiographic alignment. By exerting control over the factors that can be altered by treatment, the surgeon is better prepared to shepherd the patient on a course toward a functional and pain-free wrist.
1. Carrozzella J, Stern PJ. Treatment of comminuted distal radius fractures with pins and plaster. Hand Clin. 1988;4:391-397.
2. Feipel V, Rinnen D, Rooze M. Postero-anterior radiography of the wrist: normal database of carpal measurements. Surg Radiol Anat. 1998;20:221-226.
3. Friberg S, Lundstrom B. Radiographic measurements of the radio-carpal joint in normal adults. Acta Radiol Diagn (Stockh). 1976;17:249-256.
4. Mann FA, Wilson AJ, Gilula LA. Radiographic evaluation of the wrist: what does the hand surgeon want to know? Radiology. 1992;184:15-24.
5. Solgaard S. Angle of inclination of the articular surface of the distal radius. Radiologe. 1984;24:346-348.
6. Jeong GK, Kaplan FT, Liporace F, et al. An evaluation of two scoring systems to predict instability in fractures of the distal radius. J Trauma. 2004;57:1043-1047.
7. Lafontaine M, Delince P, Hardy D, et al. Instability of fractures of the lower end of the radius: apropos of a series of 167 cases. Acta Orthop Belg. 1989;55:203-216.
8. Altissimi M, Mancini GB, Azzara A, et al. Early and late displacement of fractures of the distal radius: the prediction of instability. Int Orthop. 1994;18:61-65.
9. Leone J, Bhandari M, Adili A, et al. Predictors of early and late instability following conservative treatment of extra-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41.
10. Abbaszadegan H, Jonsson U, von Sivers K. Prediction of instability of Colles’ fractures. Acta Orthop Scand. 1989;60:646-650.
11. Dicpinigaitis P, Wolinsky P, Hiebert R, et al. Can external fixation maintain reduction after distal radius fractures? J Trauma. 2004;57:845-850.
12. Weber ER. A rational approach for the recognition and treatment of Colles’ fracture. Hand Clin. 1987;3:13-21.
13. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19:325-340.
14. Trumble TE, Wagner W, Hanel DP, et al. Intrafocal (Kapandji) pinning of distal radius fractures with and without external fixation. J Hand Surg [Am]. 1998;23:381-394.
15. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659.
16. Altissimi M, Mancini GB, Ciaffoloni E, et al. Comminuted articular fractures of the distal radius: results of conservative treatment. Ital J Orthop Traumatol. 1991;17:117-123.
17. Catalano LW, Cole RJ, Gelberman RH, et al. Displaced intra-articular fractures of the distal aspect of the radius: long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am. 1997;79:1290-1302.
18. Goldfarb CA, Rudzki JR, Catalano LW, et al. Fifteen-year outcome of displaced intra-articular fractures of the distal radius. J Hand Surg [Am]. 2006;31:633-639.
19. Fernandez JJ, Gruen GS, Herndon JH. Outcome of distal radius fractures using the short form 36 health survey. Clin Orthop. 1997;341:36-41.
20. Gartland JJJr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895-907.
21. Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles’ fracture treatment. J Hand Surg [Am]. 1991;16:392-398.
22. Fujii K, Henmi T, Kanematsu Y, et al. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg (Hong Kong). 2002;10:9-15.
23. Batra S, Gupta A. The effect of fracture-related factors on the functional outcome at 1 year in distal radius fractures. Injury. 2002;33:499-502.
24. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
25. Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults: a descriptive arthroscopic study in 50 patients. J Hand Surg [Br]. 1997;22:638-643.
26. Richards RS, Bennett JD, Roth JH, et al. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg [Am]. 1997;22:772-776.
27. Baratz ME, Des Jardins J, Anderson DD, et al. Displaced intra-articular fractures of the distal radius: the effect of fracture displacement on contact stresses in a cadaver model. J Hand Surg [Am]. 1996;21:183-188.
28. Mehta JA, Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular fractures of the distal radius: an arthroscopically-assisted approach. J Bone Joint Surg Br. 2000;82:79-86.
29. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg [Am]. 1991;16:375-384.
30. Tsukazaki T, Iwasaki K. Ulnar wrist pain after Colles’ fracture: 109 fractures followed for 4 years. Acta Orthop Scand. 1993;64:462-464.
31. Hollevoet N, Verdonk R. The functional importance of malunion in distal radius fractures. Acta Orthop Belg. 2003;69:239-245.
32. Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop. 1996;327:135-146.
33. Lindau T, Hagberg L, Adlercreutz C, et al. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop. 2000;376:229-235.
34. Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg [Br]. 2000;25:535-543.
35. Porter M, Stockley I. Fractures of the distal radius: intermediate and end results in relation to radiologic parameters. Clin Orthop. 1987;220:241-252.
36. MacDermid JC, Donner A, Richards RS, et al. Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol. 2002;55:849-854.
37. Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: a cadaveric study. J Hand Surg [Am]. 1997;22:258-262.
38. Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius—factors affecting functional outcome. Hand Surg. 2000;5:145-153.
39. Beaule PE, Dervin GF, Giachino AA, et al. Self-reported disability following distal radius fractures: the influence of hand dominance. J Hand Surg [Am]. 2000;25:476-482.
40. Karnezis IA, Fragkiadakis EG. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84:967-970.
41. Hollevoet N, Verdonk R. Outcome of distal radius fractures in relation to bone mineral density. Acta Orthop Belg. 2003;69:510-514.
42. Young CF, Nanu AM, Checketts RG. Seven-year outcome following Colles’ type distal radial fracture: a comparison of two treatment methods. J Hand Surg [Br]. 2003;28:422-426.
43. Anzarut A, Johnson JA, Rowe BH, et al. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg [Am]. 2004;29:1121-1127.
44. Chang HC, Tay SC, Chan BK, et al. Conservative treatment of redisplaced Colles’ fractures in elderly patients older than 60 years old—anatomical and functional outcome. Hand Surg. 2001;6:137-144.
45. Dayican A, Unal VS, Ozkurt B, et al. Conservative treatment in intra-articular fractures of the distal radius: a study on the functional and anatomic outcome in elderly patients. Yonsei Med J. 2003;44:836-840.
46. Warwick D, Field J, Prothero D, et al. Function ten years after Colles’ fracture. Clin Orthop. 1993;295:270-274.
47. Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg [Am]. 2007;32:962-970.