32. Facioscapulohumeral Dystrophy
Definition
Facioscapulohumeral dystrophy (FSHD) is a relatively benign, autosomal dominant form of muscular dystrophy that produces marked atrophy of the facial musculature, shoulder girdle, and arm. Facioscapulohumeral dystrophy is also known as Landouzy-Dejerine dystrophy.
Incidence
The incidence of FSHD is approximately 1:20,000. It is the third-most common muscular dystrophy, with a higher frequency in males than females.
Etiology
The specific genetic defect that produces FSHD is not yet known. Several mechanisms have been proposed, including:
1. Position variegation effect on a proximal gene(s)
2. Mutation of a functional gene within the Kpnl repeat units
3. A mitochondrial dysfunction
4. Increased susceptibility to myoblastic oxidative stress
Signs and Symptoms
• Anterior axillary fold upward slope
• Asymmetrical weakness
• Difficulty drinking through a straw
• Difficulty with labial sounds and whistling
• Facial muscle weakness
• Footdrop gait
• Weak scapular fixation
• Weakness of anterior tibialis muscle
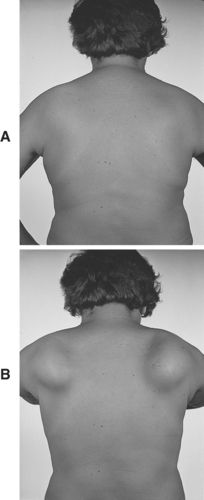 |
| Facioscapulohumeral Dystrophy. At rest (A) and with the arms exerting forward pressure (B). |
Medical Management
There is no definitive therapy for treatment of FSHD. There have been a few reports of use of albuterol; in one report an oral sustained-release form of the drug was given for 3 months and produced a 12% increase in muscle strength. Another study was a double-blind, placebo-controlled randomized trial of two strengths of albuterol, which demonstrated no improvement in global strength but reported that muscle mass and grip strength improved.
Complications
• Atrial arrest
• Bundle branch block
• Coats’ disease
• Dilated cardiomyopathy
• Epilepsy
• Hearing loss (possibly unilateral)
• Labile hypertension
• Mental impairment
Anesthesia Implications
The most relevant physiologic concern for the anesthetist is the patient’s diminution of vital capacity. This reduction is related to the weakness of respiratory accessory muscles. The patient with FSHD is likely to have recurrent upper-respiratory infections. The anesthetist should carefully auscultate the chest and inquire about any upper-respiratory symptoms or infections the patient may have. As with any other elective procedure, the surgery is best postponed until appropriate treatment can be completed and the infection can be resolved. As a result of the reduced vital capacity because of the weakness of the accessory muscles, development of atelectasis is a concern. To avert the development of atelectasis, a small amount of positive end-expiratory pressure (PEEP), such as 3 to 5 cm H 2O, may be effective.







