Facilitating Ventilation Patterns and Breathing Strategies
Individuals with breathing impairments (whether primary or secondary in origin) require a variety of interventions to optimize ventilation and oxygen delivery, as well as improving functional outcomes. Some interventions are passive in nature, such as the positioning of the patient or the application of an abdominal binder for better diaphragmatic positioning. Other interventions require very active participation on the part of the therapist, patient, or both, such as in assisted-cough techniques, in glossopharyngeal breathing instruction, or in learning a more efficient breathing pattern. Ideally techniques are incorporated into the patient’s total physical rehabilitation program, such as the use of ventilation strategies pairing breathing with movement. All of these diverse aspects of treatment play an important role in the development of a successful rehabilitation program to meet the needs of patients with pulmonary impairments. No single intervention or approach is appropriate in all cases. Sound clinical judgment and experience must be exercised when applying these ideas in each person. The interventions identified in this chapter are not inclusive. They are meant to provide examples and guidelines and to stimulate the clinician’s creative talents in order to incorporate the interventions into a comprehensive treatment program determined by individual needs that improve the outcomes for each patient (Box 23-1).
Positioning Concerns
All patients spend some portion of the day in a horizontal position for rest or sleep. Some who are acutely ill or medically compromised spent extended time in bed, and major emphasis must be placed on the mobilization of patients early and often to prevent immobility from exerting its negative effects on all body systems (see Chapter 18). Studies have shown that patients who are medicated and spend extended time on ventilators in the ICU have developed critical illness neuromuscular syndrome or ICU-acquired weakness. Interventions shown to help prevent this problem are physical therapy/activity and daily interruptions of sedative medication.1,2,3 These studies validate the need for intervention to prevent untoward effects of immobility and sedation.
Despite these problems, the time spent in a horizontal position can be used as an opportunity to assist patients in passive drainage and preventing the retention of lung secretions. It can be a natural beginning in the development of a patient’s long-term respiratory program (e.g., the prevention of respiratory complications in a patient with tetraplegia). Specific postural drainage positions are covered under airway clearance interventions (see Chapter 21). Using a combination of these positions and the patient’s position in bed, in the hospital or at home, can help to achieve multiple goals. First, various horizontal positions can assist patients in passively clearing secretions that they may have difficulty clearing actively. Pneumonia is still the leading cause of death in patients with spinal cord injury (SCI) who are tetraplegic.4 Second, these position changes provide for skin relief and better circulation. Finally, they assist in retarding the development of joint contractures or other musculoskeletal abnormalities. A four-position rotation (i.e., supine, prone, and side-to-side) or a modified six-position rotation (supine, three-quarter supine, side-lying, three-quarter prone on each side) is usually an effective and reasonable means of incorporating these goals into a long-term prophylactic program.
Simple adaptations may make ventilation easier in each of these postures. For example, when the patient is in the supine position, placing the patient’s arms up over his or her head facilitates greater anterior upper chest expansion.5 Likewise, positioning the pelvis in a slight posterior tilt facilitates more diaphragmatic excursion. (Detailed explanations of positioning are discussed in Chapter 42.) Observation of all precautions and contraindications to passive positioning is still warranted, and positions should be modified based on the individual need of each patient.
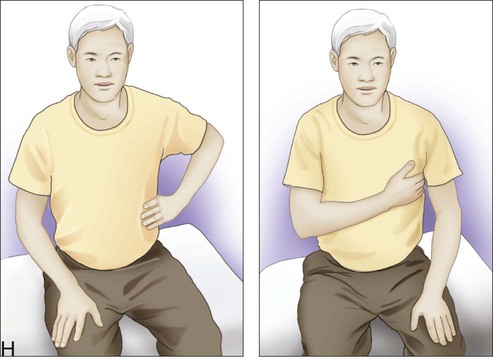
Just as passive positioning of the patient in bed helps to maintain airway clearance and improve ventilation potential, optimal passive positioning of the patient’s skeletal frame in an upright posture (sitting, standing) helps to maximize the mechanical advantages that facilitate breathing and improve cardiovascular fluid shifts. For example, patients with SCIs resulting in tetraplegia will be unable to support their intestinal contents properly under the diaphragm to allow for maximal expansion of the chest in all three planes of ventilation (see Chapter 39). The use of an abdominal support from the iliac crest to the base of the xiphoid process provides positive-pressure support to restore intestinal positioning to an upright position (Figure 23-1). Research has documented well the significant improvements in vital capacity (VC), inspiratory capacity, and tidal volume (TV) in sitting with the use of a strong abdominal support.6 These binders have also been used in nursing care to provide for better circulation and the prevention of hypotension.
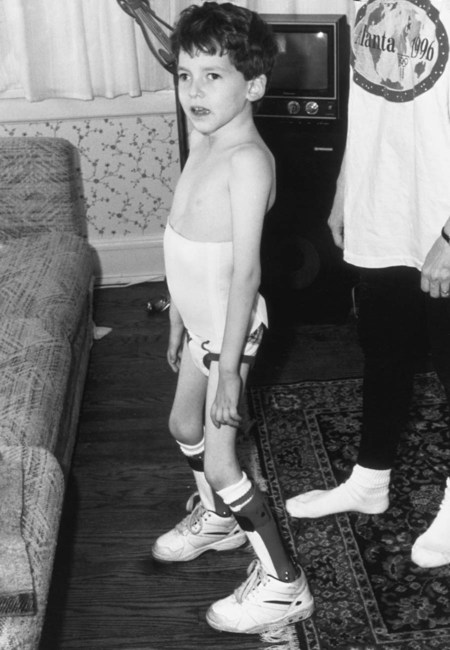
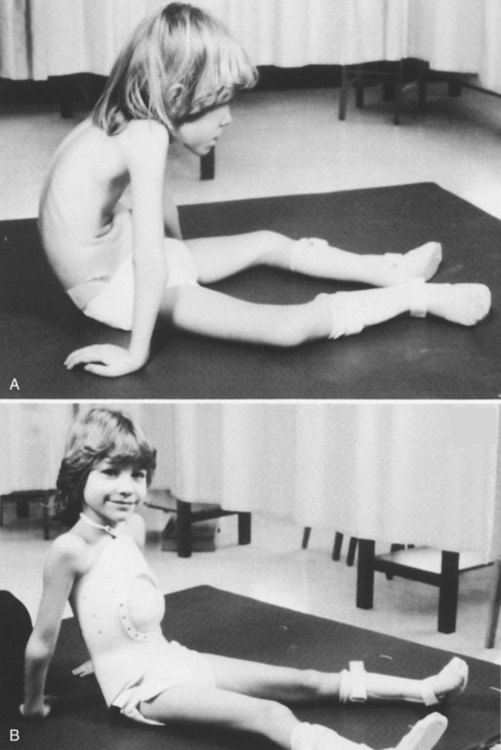
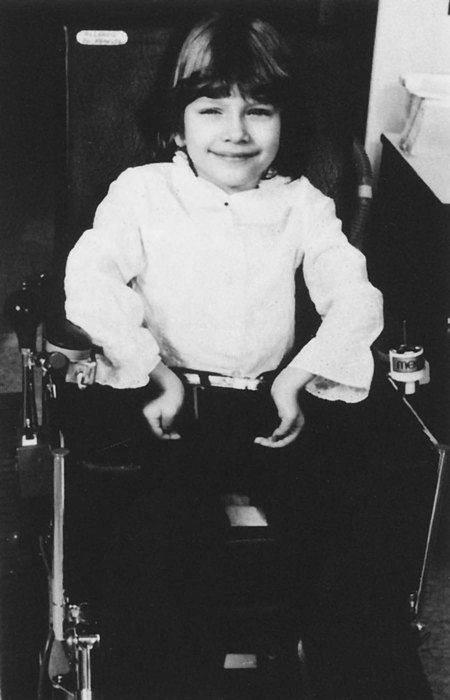
A rigid type of abdominal support can be used when the vertebral column and the abdominal viscera need support. These are called body jackets or total contact thoracic lumbar sacral orthoses (TLSOs) (Figure 23-2). A TLSO is a rigid trunk support molded individually to the shape of the patient’s entire trunk from the axilla down to the pubis. It is composed of two separate pieces, a front and a back, ideally with an anterior cutout in the abdomen to allow for normal diaphragmatic displacement of the viscera. In addition to these jackets, an elastic binder is applied around the abdomen to allow for diaphragmatic motion but minimize excessive displacement of the abdominal contents. This is particularly appropriate for a growing child who needs more spinal stability and for the completely flaccid patient with tetraplegia, who may also require the same support. Because head and neck positioning are so dependent on trunk positioning, a body jacket may make the difference for these patients between being dependent or independent in an upright posture. It may result in significantly better head control and eye contact and improved phonation. However, because the TLSO limits trunk movement, its usefulness for each patient must be assessed carefully.
The next consideration in passive respiratory techniques is proper wheelchair positioning. Optimal performance in ventilatory functioning, as well as many other areas of rehabilitation, depends on good alignment of the body against the force of gravity. Symmetry must be strived for through the use of a body jacket, lateral trunk supports in the wheelchair, abdominal binders, or some other means (Figure 23-3). This is especially important for patients with hemiplegia in whom habitual asymmetrical posturing leads to musculoskeletal problems later. Symmetrical breathing patterns and uniform aeration of all lung segments are augmented by careful upright positioning. Therefore everything from the type of neck and trunk support to the height and width of the arm rests to the length and type of the foot supports must be carefully analyzed for each patient.
Ventilatory and Movement Strategies for Improving Functional Outcomes
The patient is first positioned for successful ventilation. Then motor activities should be introduced. Interventions chosen will improve the patient’s ventilatory support, or the therapist should capitalize on the patient’s good ventilatory support to improve the motor activity. Using ventilatory strategies to improve motor performance or movement strategies to improve ventilation performance enables patients to achieve their functional goals sooner and have better health, including fewer respiratory complications. Generally, these simple concepts take no more than 1 to 2 additional minutes of therapy time, with no additional equipment costs other than a few extra pillows or towels. Therefore time and money are not mitigating factors. However, these ideas do require the practitioner to look carefully at the patient before beginning any treatment intervention and to ask, “Have I positioned my patient for ventilatory success?”; “Am I simply treating the patient in whatever position I found her or him in?”; and “Have I carefully chosen my verbal cues to include a ventilatory response and a functional response?” The practitioner must actively include ventilation in every activity to help the patient understand that breathing transcends all activities. Breathing is the bridge to function. A summary of the most important ventilation-movement strategies is listed in Box 23-2.
Incorporating Simple Therapy Tasks
Inspiration
After the patient has been carefully positioned for respiratory success, as described previously, begin the patient’s therapy or daily-living activities. In a study looking at rhythmic pronation and supination wrist movements, inspiration and exhalation adapted and became coordinated with the arm movement (Table 23-1).7,8 Accordingly, then, the simple task of passive range of movement (ROM) can easily include the active goal of increasing ventilation by asking the patient to breathe in and look up when his or her arm is raised up into shoulder flexion. This encourages the patient to breathe in when the chest wall muscles are being stretched and the ribs are naturally opening up, causing both activities to be more successful. It also begins to teach the patient to use ventilatory strategies to optimize potential functional movement, such as in reaching up to a kitchen cabinet. Patients need to focus on avoiding breath holding and incorporating breathing during each activity.
Table 23-1
Anatomy of Inspiration and Expiration
| Inspiration | Expiration | |
| Trunk | Trunk extension | Trunk flexion |
| Shoulders | Shoulder flexion, abduction, and external rotation movements | Shoulder extension, adduction, and internal rotation movements |
| Gaze | Upward eye gaze | Downward eye gaze |
Exhalation
Thus the therapist may ask the patient to slowly count out loud to 10 while the arm is being returned eccentrically to his or her side. The patient learns to correlate exhalation with shoulder extension while simultaneously learning a much more complex idea—that of controlling his or her rate and volume of expiration by including deliberate speech during exhalation maneuvers. Research is being done in the area of respiratory plasticity to evaluate changes with exercise and conditioning.9,10 Clinical observation demonstrates that patients will incorporate new ventilation strategies and that these strategies become less cognitive and more based in habit as they are repeated.
In a recent study of strategies for respiratory exercise patterns with upper extremity movements in patients with chronic obstructive pulmonary disease (COPD), 15 patients were instructed in the reverse pattern. For example, with shoulder flexion they performed the activity with exhalation versus inhalation. The researchers concluded that there was less chest asynchrony and that it may be an important strategy for people with COPD to use the opposite pattern.11 This study had only 15 patients with COPD; however, it may be noted that with ventilatory strategies, patients may try different ways of incorporating breathing. As long as patients are not breath holding, therapists should feel safe encouraging them to try techniques and see what works best for them.
Dynamic Activities
Dressing
Upper extremity dressing and upper extremity exercise can incorporate the same ideas. All movements should be coordinated with appropriate chest wall movements to maximize upper extremity tasks. Thus every time the arm is moving up above 90 degrees of shoulder flexion, the patient should be asked to breathe in, allowing for the normal shoulder/rib-cage rhythm to occur. Full shoulder flexion requires the opening of the intercostal spacing and the separation of the individual ribs.12 Many patients with neurological impairments have lost the intrinsic mobility of the chest wall and thus may have lost some functional shoulder ROM as well. Not pairing inspiration with shoulder flexion is likely to limit the patient’s shoulder ROM to approximately 140 to 150 degrees. It may also encourage Valsalva maneuvers during the activity and may cause more shoulder pain.
Facilitating a Controlled Diaphragmatic Breathing Pattern
Many patients with lung cancer also have COPD, which increases their postoperative complications because of impaired pulmonary function before surgery. In a study of patients with COPD who needed to undergo surgical resection for cancer, it was found that a preoperative pulmonary rehabilitation program of 10 visits over a 4-week period consisting of exercise prescription, inspiratory muscle training, and slow breathing technique improved patients’ postoperative progress. The group in this program required a shorter period of time in the ICU and fewer days using a chest tube. Although this study was done with only nine patients, it has implications for improvement of postoperative success. However, in many cases, it may not be feasible to have 4 weeks of pulmonary rehabilitation before lung surgery. Some surgeons are hesitant to delay the needed surgery for pulmonary rehabilitation. A larger study would need to be conducted to demonstrate cost effectiveness, as well as the benefits and risks.13
Vital capacity is also affected in cases of tetraplegia, in which patients’ vital capacity may be reduced to 1000 to 1500 mL from their normal 3000-mL vital capacity (50%). If the normal TV (normal volume of breathing) is 500 mL, this means that with each breath the patient would use 33% to 50% of his or her vital capacity (maximal inspiration followed by maximal exhalation). This would greatly increase the work of breathing and oxygen consumption just for normal quiet breathing. The patient would have little pulmonary reserve. This can lead to respiratory muscle fatigue. During exercise or stress, the patient would have an increased subjective feeling of shortness of breath and feel an increase in the work of breathing. In addition, patients with spinal cord injury who are smokers experience excessive vital capacity losses.14 Commonly used terms to describe breathing patterns are listed in Box 23-3. A listing of indications for teaching controlled-breathing techniques is provided in Box 23-4.
It should be appreciated that breathing comfortably and in a controlled manner is associated with wellness and a sense of ease. Even normal individuals who are under stress and have increased work levels are more cognizant of the increase in their work of breathing. For a patient who struggles with every breath and wonders how it will be possible to get through the day, ventilatory strategies and breathing-control techniques can be the key to maximizing potential. A list of goals for teaching controlled-breathing techniques is found in Box 23-5.
Breathing control has long been used in yoga to focus and to promote meditation. This is a key to maximizing rehabilitation. Patients who cannot breathe cannot function! It is of primary importance to assess patients’ breathing at rest and during exercise. People often hold their breath with exertion, especially during new activities, so it is vital to assess the cardiopulmonary and neuromuscular response to each new activity. In many rehabilitation centers and health clubs, Pilates exercise regimens have been used to help patients achieve core strength and back stabilization. Pilates is a method of physical and mental conditioning combined with body, mind, and spirit integration; it has been also used by dancers and choreographers to improve postural control, increase ease of movement, and improve their performance. The first phase of Pilates incorporates diaphragmatic breathing before continuing with the steps to activate the muscles of the core (multifidus, diaphragm, pelvic floor, and transverse abdominis). The belief is that when the individual has a strong core, the posture will improve and the performance of other functional activities will be improved. This is similar to our concept of teaching diaphragmatic breathing control before functional activities in people with respiratory impairments. Joseph Pilates actually used the term contrology to define his concepts. That is what we are striving to teach our patients—breath control, then function.15
Considerations in Teaching Breathing Control to Patients with Primary Versus Secondary Pulmonary Dysfunction
Patients with primary lung disease, such as COPD, asthma, bronchitis, or cystic fibrosis, present a picture very different from that of patients with secondary pulmonary deficits, SCI, Parkinson disease, myasthenia gravis, or Guillain-Barré syndrome. In general, patients with primary lung disease tend to overuse their accessory muscles and greatly increase the work of breathing secondary to shortness of breath or coughing. They often complain that they have difficulty “getting the air out,” which demonstrates the decreased expiratory flow rates noted on pulmonary function tests. This can lead to dynamic hyperinflation, in which patients continue to gasp and increase the respiratory rate so more air is coming in, but there is not time for the air to be exhaled. Large volumes of air can get trapped in the lungs, which causes increased feelings of shortness of breath and panic. The goal with these patients is to teach them to relax the neck and chest accessory muscles and use more diaphragmatic breathing (abdominal and lateral costal breathing) to reduce the work of breathing in combination with relaxed pursed-lips breathing and prolonged exhalation. Their treatment programs focus on energy conservation, relaxation, and pacing activity with breath control. In pulmonary rehabilitation programs, exercise is a key component. Patients learn to coordinate their breathing with their activities and find that they have less dyspnea with exertion.16,17
There has been controversy in the literature about the effectiveness of diaphragmatic breathing. No standardized “norms” of how to perform diaphragmatic breathing exist. However, many skilled cardiovascular and pulmonary physical therapists would consider teaching the patient with COPD how to relax the accessory muscles and use the diaphragm as an important part of the patient’s pulmonary rehabilitation. Dechman reported that in a search of the literature, pursed-lips breathing was considered most effective by people with COPD and that the literature does not strongly support the use of diaphragmatic breathing in people with COPD.18 Cahalin found there are both positive and potentially detrimental effects to diaphragmatic breathing training.19 Each individual patient needs to be evaluated to consider whether diaphragmatic breathing may be beneficial. For example, patients with severe hyperinflation and flattened diaphragms secondarily will most likely not benefit from diaphragmatic breathing because the muscle length tension relationship is abnormal and will not result in an appropriate movement of the diaphragm. With patients who have mild to moderate COPD and are overusing the accessory muscles, diaphragmatic breathing may be very helpful; it may require less oxygen consumption, decrease the respiratory rate, and increase the tidal volume.
Patients with secondary pulmonary dysfunction, such as SCI, have a more restrictive component to inspiration. In these cases, accessory muscles may be intact, but they are not being used to facilitate deep breathing or coughing. Patients may have strong diaphragmatic breaths, but the upper chest collapses on inspiration (paradoxical breathing; see Chapter 39). The goal is to teach these patients to use the accessory muscles to balance the upper and lower chest. This facilitates an increase in vital capacity that prevents atelectasis and pneumonia by increasing the volume of ventilation and improving the cough mechanism.
 Does the patient have more difficulty during inspiration or exhalation?
Does the patient have more difficulty during inspiration or exhalation?
 Is there a normal sequence to inspiration (i.e., abdominal wall rise, then lateral costal expansion, then upper chest expansion, with a full inspiration)? Or does the chest sink and the abdomen rise on inspiration?
Is there a normal sequence to inspiration (i.e., abdominal wall rise, then lateral costal expansion, then upper chest expansion, with a full inspiration)? Or does the chest sink and the abdomen rise on inspiration?
 Does the patient appear to be working hard to breathe? Is the patient using the accessory muscles to an extreme?
Does the patient appear to be working hard to breathe? Is the patient using the accessory muscles to an extreme?
 Does the patient frequently clear the throat, have trouble coughing, or have difficulty speaking at a normal volume and for the normal length of sentences?
Does the patient frequently clear the throat, have trouble coughing, or have difficulty speaking at a normal volume and for the normal length of sentences?
 Is ventilation the limiting factor in accomplishing an activity (e.g., transfer, gait, or bed mobility)?
Is ventilation the limiting factor in accomplishing an activity (e.g., transfer, gait, or bed mobility)?
Pursed-Lips Breathing
Pursed-lips breathing is a strategy that is often spontaneously used by people with COPD during episodes of dyspnea. Many patients feel this breathing pattern helps to decrease their breathlessness. The effect of PLB is an increase in the time of exhalation, which results in a decrease in the end-expiratory volume and an increase in the total time of the respiratory cycle. This results in a decreased respiratory rate and increased TV. According to studies, a decrease in the Borg scale of perceived exertion also occurs when PLB is used.20 This technique has been acknowledged by many patients with respiratory impairments as being very easy to learn and yet very effective, quick to use, and readily incorporated into their activities to reduce dyspnea.21
Relationship of the Diaphragm and Posture
The respiratory action of the diaphragm and other respiratory muscles is normally coordinated with the need to provide postural control of the trunk during movement of the extremities.8 The diaphragm acts both as a muscle of respiration and as a muscle that works in providing core stability to the trunk. However, when respiratory demand increases, the diaphragm may not be able to continue to provide both of these functions.22–27 Because the diaphragm is the primary muscle of respiration, postural control may be impaired. A complete discussion of this concept is provided in Chapter 39.
Facilitating Diaphragmatic Breathing
In the initial phases of breathing retraining, patients are taught to use the easiest intervention that facilitates diaphragmatic breathing; if it is not successful, a progression of specific facilitation and inhibition techniques will be tried. A summary of methods of facilitating diaphragmatic ventilation patterns is given in Box 23-6.
Positioning Concerns
Position of Pelvis
The first step in facilitating any breathing pattern is to position the patient for ventilatory success. The details are discussed in this chapter and in Chapter 42. Often a patient’s posture and pelvic position have dramatic effects on breathing. In general, a slight, relative posterior tilt of the pelvis facilitates diaphragmatic breathing, and a relative anterior tilt facilitates the opening of the anterior chest and upper chest breathing. It is helpful to see what difference a slight, relative change in pelvic position will do to a patient’s ability to ventilate. This is especially true in secondary pulmonary problems related to neurological and neuromuscular dysfunction. A lumbar roll or a roll under the ischial tuberosities can facilitate an anterior pelvic tilt (see Chapter 42).
Repatterning Technique
Sniffing
If working toward a generalized controlled-breathing pattern does not improve the patient’s ventilatory pattern adequately, a technique that more specifically addresses the need to initiate breathing from the diaphragm can be attempted. Sniffing is a simple and effective means of teaching diaphragmatic breathing.28 Sniffing is accomplished primarily by the diaphragm. This technique can be used first, before attempting more specific diaphragmatic training with patients who are capable of attempting sniffing because of its simplicity.
 Choosing a gravity-eliminated position such as side-lying or a gravity-assisted position such as a supported semi-Fowler sitting position (supported spine)
Choosing a gravity-eliminated position such as side-lying or a gravity-assisted position such as a supported semi-Fowler sitting position (supported spine)
 Choosing a relatively posteriorly tilted pelvis with flexed knees
Choosing a relatively posteriorly tilted pelvis with flexed knees
 Choosing arm flexion below 90 degrees (in relative shoulder extension, adduction, and internal rotation)
Choosing arm flexion below 90 degrees (in relative shoulder extension, adduction, and internal rotation)
 Choosing to use a pillow or pillows under the patient’s head
Choosing to use a pillow or pillows under the patient’s head
For each patient, choices will be different (e.g., the amount of knee flexion or the number of pillows). Find the right combination of positioning characteristics that best facilitates diaphragmatic movement for that particular patient. (For details on positioning, see Chapter 42.) In this manner the therapist sets up the patient for ventilatory success before beginning the manual or verbal technique.
Procedure for Teaching Controlled Diaphragmatic Breathing (Scoop Technique)
The following is a suggested sequence:
1. Position the patient for success, generally side-lying in a semi-Fowler position or supine in a semi-Fowler position, with a bend in the knees to achieve a relative posterior pelvic tilt and relaxation of the abdominal muscles.
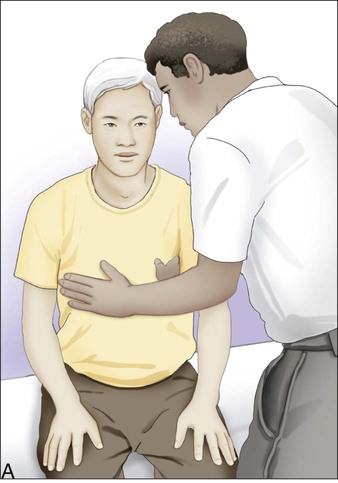
2. Place your hand on the patient’s abdomen at the level of the umbilicus. Tell the patient you want to feel his or her breathing. Follow the patient’s breathing pattern for a few cycles until you are in synchrony with his or her respiratory rhythm. Do not invade the patient’s breathing pattern; rather, at first, follow its movement.
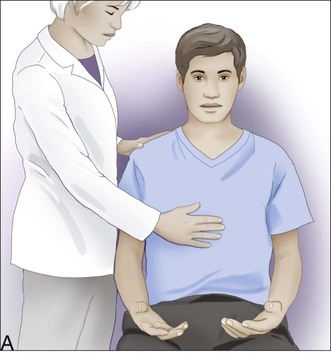
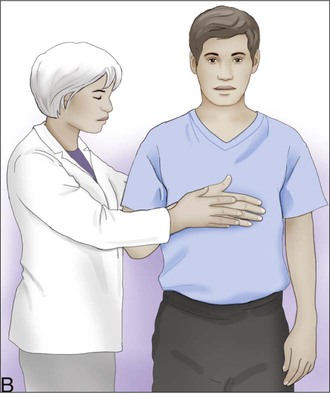
3. After the normal end of the patient’s exhalation, give a slow stretch and “scoop” your hand up and under the anterior thorax as shown in Figure 23-4, A. Then ask the patient, “Now, breathe into my hand,” as the slow scoop stretch is done.
4. As the scoop stretch is performed, instruct the patient to “breathe into my hand” during the inspiration. Give a scoop at the end of exhalation with each breath. The verbal command can be effectively replaced after a few respiratory cycles with the therapist’s audible breathing to facilitate the ventilatory pattern.
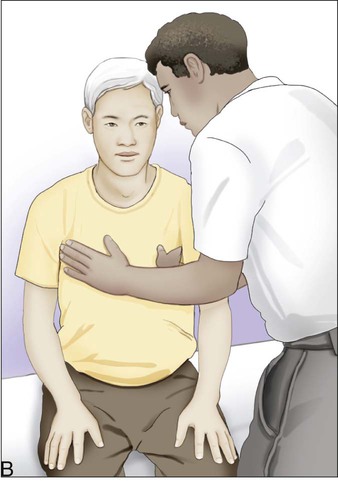
5. After achieving some success, call the patient’s attention to the awareness of the breathing pattern. For example, ask, “Can you feel how your abdomen rises as you breathe in and your ribs go up to the side?” The patient’s hand can be placed on the abdomen with the therapist’s hand on top. Reinforce the breathing pattern, then remove your hand and allow the patient to feel independently the ventilatory pattern (Figure 23-4, B).
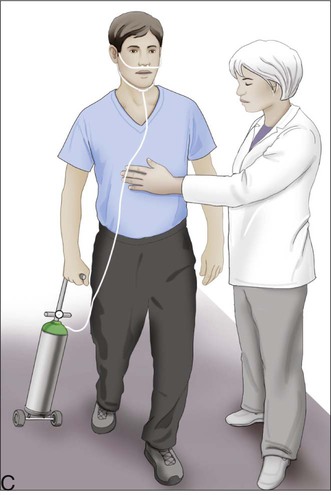
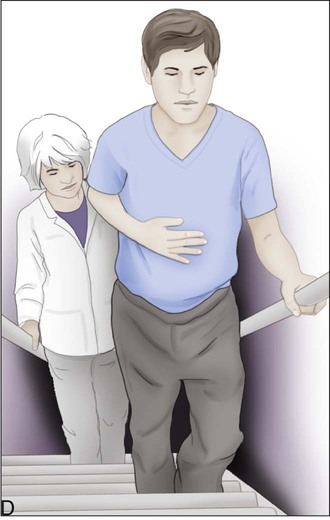
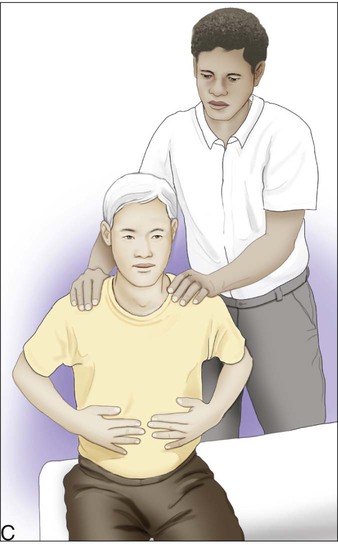
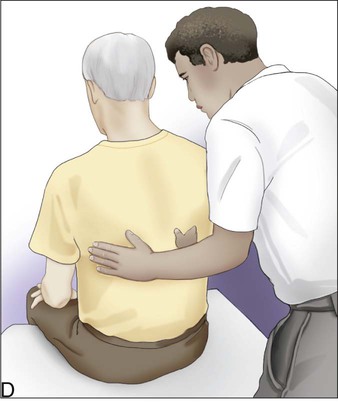
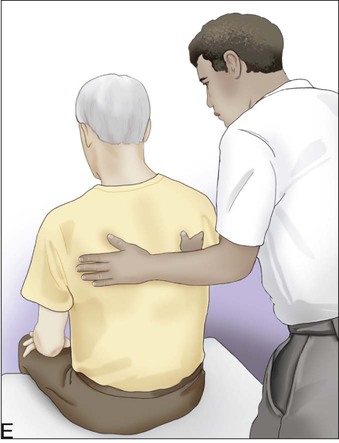
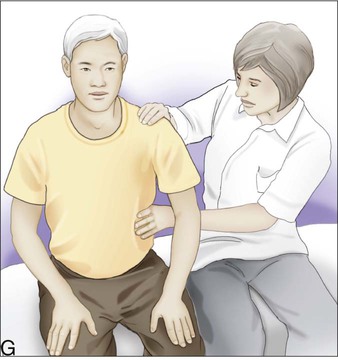
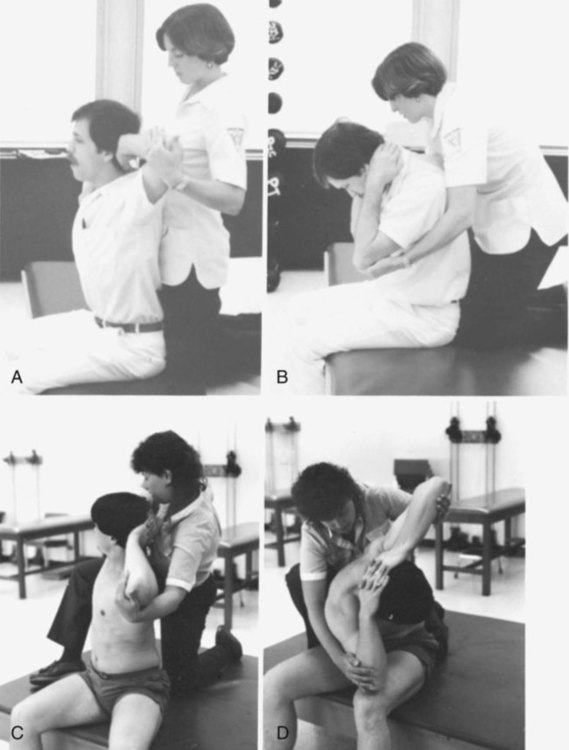
When the patient has mastered the breathing pattern in the side-lying position, try supine. Then progress to sitting (Figure 23-5, A), then standing (Figure 23-5, B), then walking (Figure 23-5, C) and, finally, stairs (Figure 23-5, D). Each position increases the difficulty in performing diaphragmatic breathing. In the side-lying or supine position, the patient is fully supported. The side-lying position is especially good for initial teaching of diaphragmatic breathing because the diaphragm is in a gravity-eliminated position. In the supine position, the patient must breathe against gravity. As he or she progresses to sitting, the patient must also provide trunk support and maintain stability against gravity, as well as relax the shoulders. In standing, the entire body must be supported, and when walking and stairs are added, the elements of breathing coordination, weight shifting, and balance increase the complexity of the activity.
In general, the preferred pattern for a patient with primary pulmonary dysfunction is as follows:
1. Have the patient pause at the base of the stairs to gain control.
2. Have the patient take a breath in and move up one step while exhaling.
3. The patient then pauses to inspire and exhales while walking up another step.
4. The patient should be encouraged to use the handrail and pace his or her movement slowly and with breath control.
Lateral Costal Breathing
Lateral costal breathing also facilitates diaphragmatic excursion. It may be done bilaterally or unilaterally (Figure 23-6). Lower chest lateral costal expansion facilitates diaphragmatic and intercostal breathing in which the mid-chest recruits primarily intercostal activity.29
Mobilizing the Thorax
It is beyond the scope of this textbook to detail all the numerous techniques involved in musculoskeletal mobilization of the thorax, but some simple techniques and suggestions for further study are presented. A summary of mobilization techniques is found in Box 23-7.
 Myofascial release of tight connective tissues (e.g., scar tissue secondary to areas of surgery or trauma)
Myofascial release of tight connective tissues (e.g., scar tissue secondary to areas of surgery or trauma)
 Soft tissue release in tight muscle groups (Note: Neurologically impaired patients often present with tightness in the pectoralis, intercostal, and quadratus lumborum muscle groups, whereas orthopedically impaired patients tend to have more tightness in the neck and back muscles.)
Soft tissue release in tight muscle groups (Note: Neurologically impaired patients often present with tightness in the pectoralis, intercostal, and quadratus lumborum muscle groups, whereas orthopedically impaired patients tend to have more tightness in the neck and back muscles.)
Facilitating Accessory Muscles in Ventilation
If the patient is still not demonstrating an optimal breathing pattern after experiencing appropriate positioning, appropriate ventilatory strategies, chest wall mobilization, and diaphragmatic retraining, specific facilitatory or inhibitory techniques should be initiated to stimulate the accessory muscles of ventilation. Specific techniques are discussed here in detail. A summary of interventions is listed in Box 23-8.
Because the diaphragm normally supplies the bulk of the inspired air during quiet breathing, diaphragmatic breathing is the preferred pattern of breathing. However, after certain neurological insults, strictly diaphragmatic breathing may not be possible or even preferred.30 Unlike pulmonary rehabilitation programs for people with COPD or asthma, in which diaphragmatic breathing is almost always encouraged and use of accessory muscles discouraged, the restoration of independent, efficient breathing patterns for people with neurological impairment may require the regular use of accessory muscles.
Pectoralis Facilitation
The pectoralis muscle group provides powerful anterior and lateral expansion of the upper chest and can substitute quite effectively for paralyzed intercostal muscles in the upper chest when trained to do so. Training usually begins in either a modified side-lying or a supine position. To increase the use of this muscle group during inspiration, the therapist should place his or her hand in the same direction as the contracting muscle fibers. Specific proprioceptive input is very important when facilitating a muscle, so make sure the hand is placed diagonally on the upper thorax (Figure 23-7).
Sternocleidomastoid and Scalene Facilitation
The same principle can be applied to the sternocleidomastoid and scalene muscles.31 When the patient is in the supine position, the therapist need change only the angle of hand alignment to more specifically facilitate the sternocleidomastoid and scalene muscles. Turning the hands parallel to the trunk so that the fingers are pointing up toward the neck rather than pointing out toward the shoulder, the therapist applies the same quick stretch and uses the same verbal cues. The altered hand position now specifically facilitates the sternocleidomastoid and scalene muscles and secondarily influences the pectoralis muscles. The sternocleidomastoid and scalene muscles expand the chest primarily in a superior and anterior plane, whereas the pectoralis muscles expand the chest primarily in a lateral and anterior plane, thus accounting for the slight difference in the facilitation positioning.
Inhibition of the Diaphragm
An unusually strong diaphragm, acting without support from surrounding musculature, specifically the intercostals and abdominal muscles, may also need to be inhibited. For example, patients with paraplegia or lower-level tetraplegia with intact diaphragm but absent abdominal and intercostal muscles may demonstrate a paradoxical breathing pattern (see compensatory breathing patterns, Chapter 39). In this case, the accessory muscles must be encouraged to keep the diaphragm in check, attempting to avoid the development of a pectus excavatum. The goal of this breathing retraining method is to stop the paradoxical movements of the upper chest during inspiration by balancing the use of the upper and lower chest. In some cases, spastic intercostal muscles, found in some spinal cord injuries, may intercede to prevent this paradoxical movement by maintaining the upper chest’s position during inspiration in spite of the negative pressure within the chest and gravity’s influence on the chest. Balancing the movement of the chest should produce an increase in TV and VC potential and mobilize a greater portion of the chest.
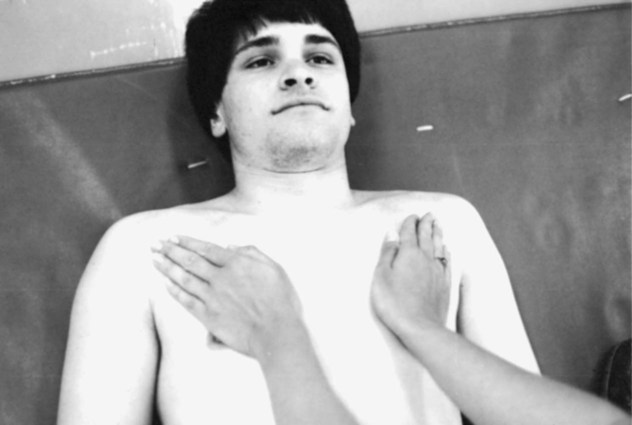
To perform the diaphragm-inhibiting technique, the patient is positioned in a supine, semi-sitting, or side-lying position, with the top arm positioned overhead or pulled back at the waist to open up the upper chest. If the patient can tolerate it, pillows are removed from under his or her head, the pelvis tilted anteriorly, and airway safety is assessed by checking to see whether the patient can still swallow comfortably. The heel of the therapist’s hand is placed lightly on the patient’s abdomen at about the level of the umbilicus. No instructions are given to the patient at this point. As the patient begins to exhale a normal breath of air, the therapist gently allows the heel of his or her hand to move up and in toward the central tendon of the patient’s diaphragm (see Figure 23-4). When the expiration of that breath is complete, the therapist strictly maintains the hand position in that shortened expiratory position. During the following inspiratory phase, the diaphragm will experience some gentle resistance to its inferior descent, causing inhibition to its full ROM. On the next expiration, the technique is repeated, with the therapist carefully pushing the heel of his or her hand further up and in, maintaining greater inhibition during each inspiratory phase. After two or three ventilatory cycles, a patient usually begins subconsciously to alter his or her breathing pattern to include more upper chest expansion in order to reconcile the diaphragm’s transient inability to produce enough chest expansion to yield an adequate TV. The therapist should carefully observe which accessory muscles the patient spontaneously chooses. Are they used symmetrically? What is the general quality of the movement? Is the onset harsh or smooth? Does the patient appear fatigued or uncoordinated?
This technique is particularly effective in patients who are having difficulty cognitively altering their own breathing patterns, such as small children, brain-damaged patients, or slow motor learners, because it requires no cognitive effort until success has already been achieved. Extra care must be taken to avoid initiating any applied pressure quickly because of the likelihood of eliciting unwanted abdominal contractions or spasticity32 or eliciting a stronger diaphragmatic contraction resulting from the quick stretch reflex. The technique should never be painful. The therapist must keep his or her hand on the abdomen, not the rib cage, to properly influence the diaphragm. This technique can be progressed by changing postures, which requires greater trunk control. Can the patient still maintain the overall pattern? Can the patient breathe without paradoxical movements against gravity?
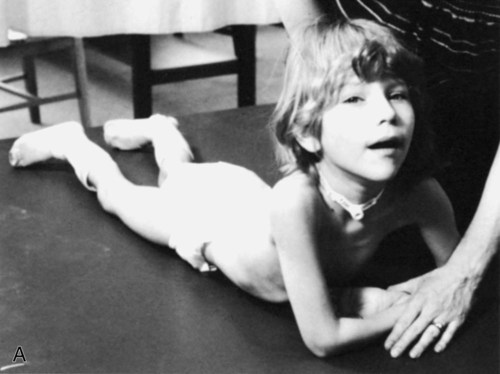
The second technique is for the more advanced patient and simply presents a physical block to diaphragmatic excursion. The patient is positioned in a prone-on-elbows position (Figure 23-8, A). In patients who are most severely impaired neurologically, the lower chest will be in direct contact with the surface, so lower anterior and inferior expansion is inhibited and lateral costal expansion is limited. The upper chest is positioned in extension and the upper extremities are fixed, optimizing the length-tension relationship of the anterior and superior accessory muscles for easy facilitation. In addition, anterior excursion of the upper chest is now in a gravity-assisted posture. Through the use of head and neck patterns, such as in PNF diagonals, or the use of static-dynamic activities, such as in weight shifting to one supporting limb while reaching out with the other extremity, the therapist can readily facilitate greater upper chest breathing (Figure 23-8, B). Therapists can use these same patterns to achieve other goals, such as increased head and neck control, increased shoulder stability, or increased upper body balance. Thus by helping patients to coordinate movement goals with ventilatory patterns, it becomes more likely that patients will incorporate these patterns functionally into their daily activities. This is the ultimate goal of any ventilatory retraining procedure.
Patients with Asymmetrical Dysfunction
Patients with asymmetrical weakness need a different approach from the controlled or upper chest breathing patterns presented previously.33 These patients need facilitation of the weaker side to promote symmetrical chest wall expansion in both the upper and lower chest. A summary of techniques is listed in Box 23-9.
Reducing Respiratory Rates
In addition to altering breathing patterns through facilitation and inhibition techniques, reducing RRs may also be necessary before arriving at an efficient breathing pattern for some patients. See Box 23-10 for a summary of techniques. Many patients with neurological impairment who have high neuromuscular tone increase their RRs to compensate for a decrease in their TVs or because of brainstem impairments that affect the respiratory centers. In addition, many patients who are anxious, such as people with asthma and those who have orthopedic or surgical conditions and are experiencing pain, may also demonstrate excessively high RRs. Attempting to restore ventilatory efficiency may require increasing TV while concurrently decreasing RR.
Counter-Rotation
 Patients with decreased cognitive functioning after a neurological insult or after surgery
Patients with decreased cognitive functioning after a neurological insult or after surgery
As described in Chapter 22, counter-rotation also can be easily adapted as a very effective assisted-cough technique. One medical contraindication for this technique, because of its rotary nature, is bony instability of the spine.
The second phase requires the therapist to slowly change position. Transitioning to a diagonal posture, the therapist then stands or half-kneels behind the patient near his or her hips, turning to a diagonal position until facing the patient’s head at roughly a 45-degree angle. Here the hand placement begins to get more specific. Assume again that the patient is side-lying on the left. At the beginning of the expiratory cycle, the therapist’s left hand slowly glides over the patient’s shoulder on the right pectoral region, with care being taken not to unintentionally use the thumb or finger tips; the right hand slowly glides back to the patient’s right gluteal fossa (the hollow of the buttocks) (see Figure 22-6, A). The therapist can then manually compress the rib cage on all three planes of ventilation at the end of exhalation by gently pulling the shoulder back and down, while simultaneously pushing the hip up and forward. This movement promotes more complete exhalation.
Butterfly Technique
This technique can be modified to encourage more intercostal and oblique abdominal muscle contractions by using a diagonal rather than a straight plane of movement. Have the patient look up and over one shoulder as he or she breathes in and brings arms up and behind the head. Then have the patient look down and away toward the opposite knee while breathing out and bringing arms down to the opposite knee (Figure 23-9).
Glossopharyngeal Breathing
A small number of patients with neurological impairments require more than just promoting the use of accessory muscles or changing RR to meet basic ventilatory needs.34 In the past decade, more people experiencing high-level SCIs (above C4) have survived the initial trauma because of advances in medical technology. The therapist in the rehabilitation setting is then faced with the difficult task of restoring quality of life. For these patients, as well as many older adult polio patients, mastery of the glossopharyngeal breathing (GPB) technique allows for greater voluntary ventilation, which many patients say improves the quality of their lives. This augmented breathing pattern allows patients to regain some control over their lives and to regain control over their ventilation, which was lost as a result of severe neurological insult.
If possible, the patient is positioned in an upright or at least a symmetrical position. Specifically, the patient is instructed to bring the jaws down and then forward as if reaching the bottom lip up for a carrot dangling just in front and above the upper lip (Figure 23-10, A). Slight cervical hyperextension is necessary to allow for maximal temporal mandibular joint (TMJ) excursion. (A contraindication for this technique is a TMJ disorder.) The lips should be shaped as if they were making the sound oop. The patient is then told to close the mouth, reaching the bottom lip up to the top lip (Figure 23-10, B). The tongue and jaw are drawn back toward the throat, with the mouth and tongue formed as though saying up or ell (see Figure 23-10, B). The lower jaw moves in a roughly rectangular pattern. Most patients learn the stroking maneuvers by making the sounds; as they become more proficient, the sounds and excessive head and neck motions diminish. Often, the students (patients) outperform the teachers (therapists) because through consistent use, they learn all of the technique’s finer subtleties.
Although this technique can be broken down into several stages, as it has been here for the purpose of description, most of the literature cautions the therapist against doing so.35 Simple, minimal instructions seem to accomplish more, perhaps because the continuity of movement is so essential to the success of the inhalation. Specific instructions can be given later if necessary.
Common problems encountered with GPB instruction can be found in Box 23-11. Avoiding any instruction for the tongue seems to produce better results. Concentrate on assisting the patient in learning the external physical movements.
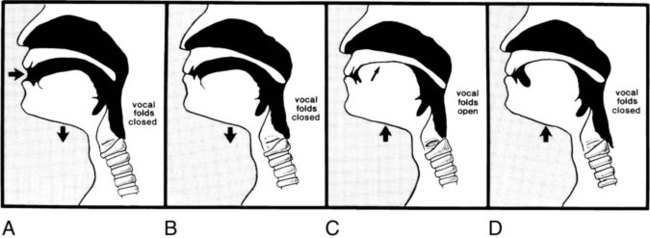
Enhancing Vocalization Skills
In contrast to procedures that assist a patient in inhalation, procedures intended to improve a patient’s phonation skill must focus on elongating the expiration phase. Coughing is a gross-motor skill that relies more on force than on fine control of the ventilatory muscles for its effectiveness. Conversely, phonation requires precise, fine-motor control of these muscles and demands that the vocal folds provide a consistent air flow through the larynx. Both are expiration activities and they depend on the preceding inspiration for optimal performance; however, coughing uses concentric contractions of the expiratory muscles to force the air out, whereas quiet talking uses primarily eccentric contractions of the inspiratory muscles to slowly release the air during expiration. Because of these differences, procedures to improve coughing and phonation are different in focus. Considering the relationship between speaking and breathing and the concepts of shared respiratory control, it is notable that speaking can lead to shortness of breath and shortness of breath can alter speaking ability.36 Previous discussions of posture and use of abdominal binders in patients with spinal cord injury should also be considered when speaking is impaired.37 A summary of techniques is listed in Box 23-12. Coughing is covered in detail in Chapter 22.