Eyelid Anatomy and Function
Overview of External Anatomy
The eyelids comprise of an upper and lower eyelid, joined at the medial and lateral canthi. The average aperture of the eyelids measures about 30 mm in horizontal width, and approximately 10 mm in vertical height. The highest peak on the upper eyelid lies slightly nasal, and the lowest contour of the lower eyelid rests slightly lateral. The upper eyelid generally covers 1–3 mm of the upper cornea, and the lower eyelid typically rests at, or near the lower limbus. The upper eyelid crease falls 6–10 mm from the eyelid lash line. The brow is positioned anterior to the superior orbital rim.1–4
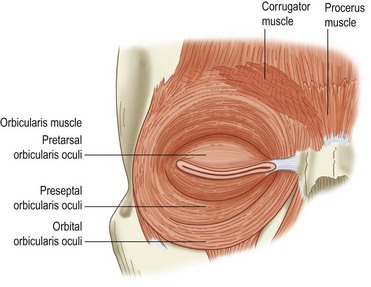
Eyelid Muscles: Protractors
The main protractor of the eyelid, which serves to close the eye, is the orbicularis oculi. It is innervated by the facial nerve, and divided into the pretarsal, preseptal, and orbital portions (Fig. 2.1). The pretarsal and preseptal portions are used in spontaneous blink, and the orbital portion is needed for forced eyelid closure. Facial nerve palsy can lead to lagophthalmos and incomplete blink.
Eyelid Muscles: Retractors
Upper Lid Retractor: Levator
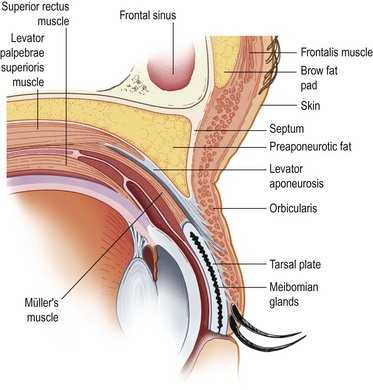
Whitnall’s ligament or superior traverse ligament is a condensation of elastic fibers of the anterior sheath of the levator muscle. It is located between the transition of the levator aponeurosis and muscle. It provides the suspension support for the upper eyelid and superior orbital tissues. It is thought to transfer the vector of force of the levator muscle from anterior–posterior to superior–inferior. It is analogous to Lockwood’s ligament in the lower eyelid. Medially it attaches near the trochlea and superior oblique tendon, and laterally, it runs through the lacrimal gland, and attaches to the inside of the lateral orbital wall, approximately 10 mm above the lateral tubercle.1–4
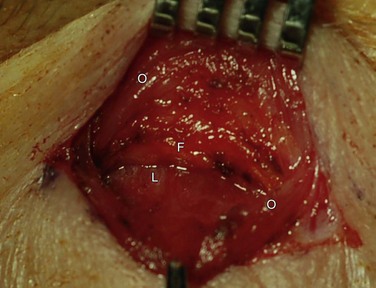
The levator aponeurosis divides into an anterior and posterior portion just above the superior tarsal border. The anterior portion inserts into the pretarsal orbicularis. The most superior portion of these attachments forms the eyelid crease with contraction of the levator complex (Fig. 2.2). The posterior portion inserts onto the anterior surface of the tarsus. The aponeurosis appears as a thick whitish band between Whitnall’s ligament and the tarsal plate (Fig. 2.3).
The medial horn of levator aponeurosis inserts onto the posterior lacrimal crest.
Upper Lid Retractor: Müller’s Muscle
Müller’s muscle originates underneath the levator aponeurosis, 12–13 mm above the upper tarsal margin. It is 15–20 mm wide. It is sympathetically innervated, extends inferiorly to insert at the superior tarsal border, and provides 2 mm of elevation. If interrupted, as in Horner’s syndrome, it causes a mild ptosis. Müller’s muscle is firmly attached to the palpebral conjunctiva. The peripheral arterial arcade is located between the levator aponeurosis and Müller’s muscle above the superior tarsal border and can serve as a useful surgical landmark.1–4
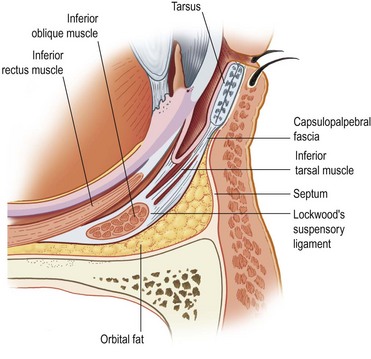
Lower Lid Retractors
The lower eyelid retractors serve to depress the eyelid in downgaze, and maintain the upright position of the tarsal plate. The capsulopalpebral fascia in the lower lid is analogous to the levator in the upper lid (Fig. 2.4). It is fibrous tissue that originates from the sheath of the inferior rectus muscle, divides as it encircles the inferior oblique and fuses with the sheath of the inferior oblique. Then the two portions join to form Lockwood’s ligament.
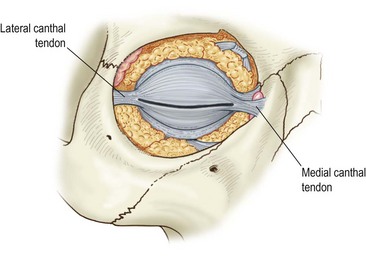
Canthal Tendons
The canthal tendons are extensions of the orbicularis muscle and attach to the periorbita/periosteum over bone (Fig. 2.5).
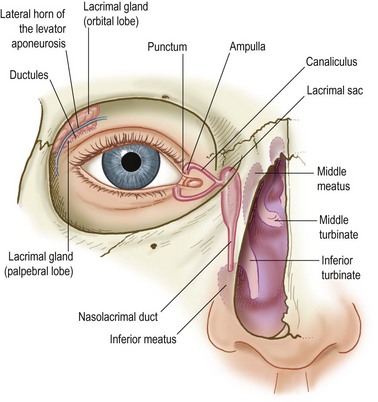
Lacrimal Drainage System
The gateways of lacrimal drainage are the puncta. The puncta are located medially on the upper and lower eyelids, on lacrimal papilla. The puncta are on the posterior aspect of the eyelid margin, and are medial to the ciliary border. The upper punctum is medial to the lower lid punctum (Fig. 2.6).
References
1. Nerad, JA. Techniques in ophthalmic plastic surgery: a personal tutorial, 1st ed. Philadelphia: Elsevier Health Sciences; 2009.
2. Tyers, AG, Collins, JRO. Colour atlas of ophthalmic plastic surgery, 2nd ed. Philadelphia: Elsevier Health Sciences; 2001.
3. Kersten, RC, Bartley, GB, Nerad, JA, et al. Basic and clinical science course, section 7: orbit, eyelids, and lacrimal system. San Francisco: American Academy of Ophthalmology; 2001.
4. Levine, MR. Manual of oculoplastic surgery, 4th ed. Thorofare: SLACK Incorporated; 2010.