CHAPTER 2 Extracorporeal Membrane Oxygenation Cannulation
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations—Patient Management before Extracorporeal Life Support
Type of Support
Cannula Considerations
Selection of Technique
Step 3: Operative Steps—Cannula Insertion for Neonatal ECLS
VV/VA Cannulation: Open Technique
Preoperative
Operation
Position of Patient
Exposure of the Carotid Sheath
Dissection of the Vessels
Arteriotomy/Venotomy
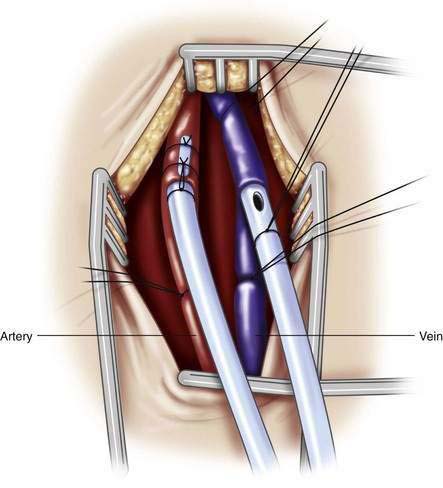
Cannula Placement (Fig. 2-1)
VV Cannulation: Semi-open Technique
Incision and Vein Exposure
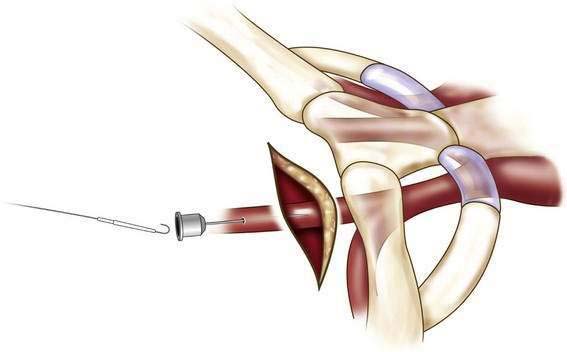
Guidewire Placement (Fig. 2-2)
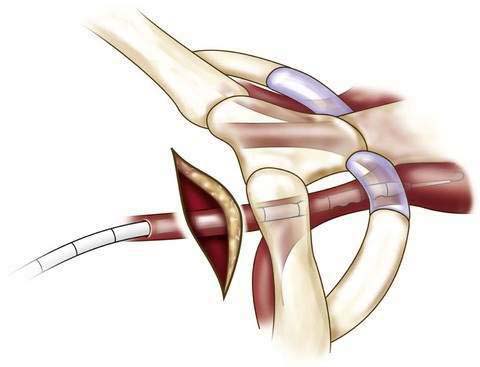
Cannula Placement (Fig. 2-3)
Wound Closure and Cannula Fixation
Cannula Insertion for Pediatric ECLS
Venovenous Bypass
Cannula Insertion for Adolescent ECLS
Venovenous Bypass
Venoarterial Bypass
 Jugular vein to carotid artery bypass as used in infants has been used successfully and works well, especially for combined cardiac and pulmonary support. It provides very good perfusion to all branches of the aortic arch and distal aorta, but it increases afterload by increasing aortic pressure. Ligation of the cerebral artery may cause cerebral edema.
Jugular vein to carotid artery bypass as used in infants has been used successfully and works well, especially for combined cardiac and pulmonary support. It provides very good perfusion to all branches of the aortic arch and distal aorta, but it increases afterload by increasing aortic pressure. Ligation of the cerebral artery may cause cerebral edema. Jugular vein to femoral artery bypass provides adequate distal perfusion, but this approach can fail to perfuse the aortic arch in situations where the native cardiac function is good. If the blood ejected from the left ventricle is desaturated because of pulmonary dysfunction, the aortic arch might not receive well-oxygenated pump blood, and the result will be hypoxemia in the upper half of the body. This problem can be solved by adding an additional perfusion cannula to the venous circulation to create venoarteriovenous bypass, which increases oxygenation of the right ventricular blood much like VV bypass and provides the hemodynamic support of VA bypass. The increased afterload from VA bypass may prevent the failing left ventricle from ejecting blood and result in high left atrial pressure, causing pulmonary edema. This situation can be managed by draining blood from the left atrium into the venous side of the bypass circuit either from direct cannulation of the left atrium by thoracotomy or by catheter-based balloon atrial septostomy.
Jugular vein to femoral artery bypass provides adequate distal perfusion, but this approach can fail to perfuse the aortic arch in situations where the native cardiac function is good. If the blood ejected from the left ventricle is desaturated because of pulmonary dysfunction, the aortic arch might not receive well-oxygenated pump blood, and the result will be hypoxemia in the upper half of the body. This problem can be solved by adding an additional perfusion cannula to the venous circulation to create venoarteriovenous bypass, which increases oxygenation of the right ventricular blood much like VV bypass and provides the hemodynamic support of VA bypass. The increased afterload from VA bypass may prevent the failing left ventricle from ejecting blood and result in high left atrial pressure, causing pulmonary edema. This situation can be managed by draining blood from the left atrium into the venous side of the bypass circuit either from direct cannulation of the left atrium by thoracotomy or by catheter-based balloon atrial septostomy. Arterial cannulation can be performed either percutaneously or by direct cutdown of the vessel. With either method, if the cannula is large enough to diminish flow, distal ischemia may result. Several methods of managing this type of ischemia have been described.
Arterial cannulation can be performed either percutaneously or by direct cutdown of the vessel. With either method, if the cannula is large enough to diminish flow, distal ischemia may result. Several methods of managing this type of ischemia have been described. Placement of a distal perfusion catheter can be used with the open technique by placing a connector with a side port and placing small tubing directed into the vessel distally at the cutdown site. With the percutaneous technique, an arterial line can be placed into either the dorsalis pedis or posterior tibial artery by cutdown and the distal pressure measured. If the pressure is less than 50 mm Hg, the catheter can be perfused by a line from the perfusion limb of the circuit.
Placement of a distal perfusion catheter can be used with the open technique by placing a connector with a side port and placing small tubing directed into the vessel distally at the cutdown site. With the percutaneous technique, an arterial line can be placed into either the dorsalis pedis or posterior tibial artery by cutdown and the distal pressure measured. If the pressure is less than 50 mm Hg, the catheter can be perfused by a line from the perfusion limb of the circuit. Arterial decannulation is more complicated. Direct pressure may be all that is needed for percutaneously placed arterial cannulas. The larger the cannula is in relation to the artery, the more likely that a pseudoaneurysm or arterial stenosis will result.
Arterial decannulation is more complicated. Direct pressure may be all that is needed for percutaneously placed arterial cannulas. The larger the cannula is in relation to the artery, the more likely that a pseudoaneurysm or arterial stenosis will result. An alternative to this method is venous patch angioplasty, a technique used for removing arterial cannulas placed by cutdown. In this technique, the vessel is controlled by a clamp, and the cannula is removed. A diamond-shaped patch of vein is then sutured into the defect, which both closes the hole and prevents stricture at the repair site.
An alternative to this method is venous patch angioplasty, a technique used for removing arterial cannulas placed by cutdown. In this technique, the vessel is controlled by a clamp, and the cannula is removed. A diamond-shaped patch of vein is then sutured into the defect, which both closes the hole and prevents stricture at the repair site.Transthoracic Cannulation
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Difficulty Threading the Venous Cannula
Vein Division
Proximal Vein Lost in Mediastinum
Foley DS, Swaniker F, Pranikoff T, Bartlett RH, Hirschl R. Percutaneous cannulation for venovenous extracorporeal life support (ECLS). J Pediatr Surg. 2000;35:943-947.
Lazar EL, Abramson SJ, Weinstein S, et al. Neuroimaging of brain injury in neonates treated with extracorporeal membrane oxygenation: Lessons learned from serial examinations. J Pediatr Surg. 1994;29:186-191.
Miskulin J, Annich G, Grams R, et al. Venous-arteriovenous cannulation for adult ECMO patients with cardiogenic shock. 14th Annual ELSO Conference, September 10-12, 2004, Chicago, IL.
Montoya JP, Merz SI, Bartlett RH. A standardized system for describing flow/pressure relationships in vascular access devices. Trans Am Soc Artif Intern Organs. 1991;37:4-8.
Peek GJ, Firmin RK, Moore HM, et al. Cannulation of neonates for venovenous extracorporeal life support. Ann Thoracic Surg. 1996;61:1291-1292.
Pranikoff T, Hirschl RB. Neonatal extracorporeal membrane oxygenation. In Carter DC, Russell RCG, editors: Rob and Smith’s operative surgery, 6th ed, London: Butterworth-Heinemann, 2005.
Pranikoff T, Hirschl RB, Remenapp R, Swaniker F, Bartlett RH. Venovenous extracorporeal life support via percutaneous cannulation in 94 patients. Chest. 1999;115:818-822.
Pranikoff T, Hirschl RB. Neonatal extracorporeal membrane oxygenation. In Carter DC, Russell RCG, editors: Rob and Smith’s operative surgery, 5th ed, London: Butterworth-Heinemann, 1995.
Rich PB, Awad SS, Crotti S, Hirschl RB, Bartlett RH, Schreiner RJ. A prospective comparison of atrio-femoral and femoro-atrial flow in adult venovenous extracorporeal life support. J Thorac Cardiovasc Surg. 1998;116:628-632.
Schumacher RE, Barks JD, Johnston MV, et al. Right-sided brain lesions in infants following extracorporeal membrane oxygenation. Pediatrics. 1988;82:155-161.
Sinard JM, Merz SI, Hatcher MD, et al. Evaluation of extracorporeal perfusion catheters using a standardized measurement technique—the M-number. Trans Am Soc Artif Intern Organs. 1991;37:60-64.
Streltz LJ, Bej MD, Graziani LJ, et al. Utility of serial EEGs in neonates during extracorporeal membrane oxygenation. Pediatr Neurol. 1992;8:190-196.
1996 UK collaborative randomized trial of neonatal extracorporeal membrane oxygenation. UK Collaborative ECMO Trial Group. Lancet. 1996;348:75-82.
Walker LK, Short BL, Traystman RJ. Impairment of cerebral autoregulation during venovenous extracorporeal membrane oxygenation in the newborn lamb. Crit Care Med. 1996;24:2001-2006.