Chapter 12 Extra-uterine pregnancy/ectopic gestation
OUTCOME FOR THE PREGNANCY
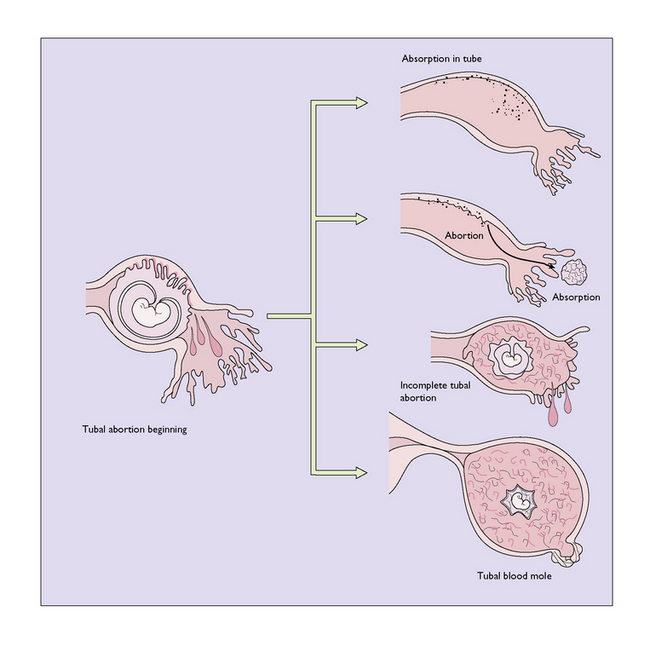
Tubal abortion
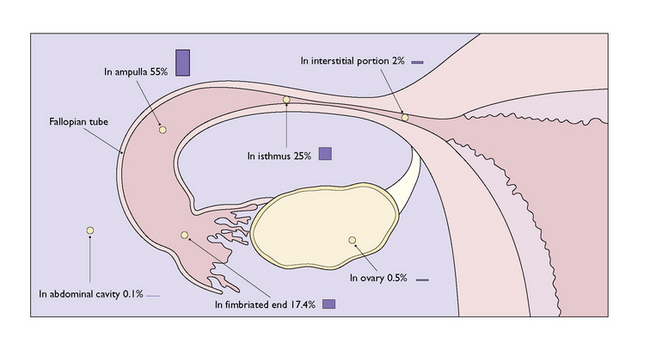
This occurs in 65% of cases and is the usual outcome in fimbrial and ampullary implantation (Fig. 12.2). Repeated small haemorrhages from the invaded area of the tubal wall detach the ovum, which dies and:
Tubal rupture
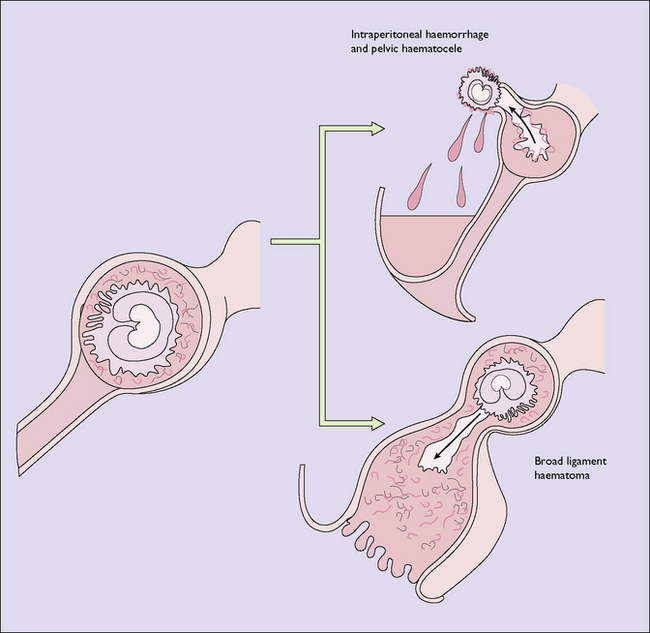
This occurs in 35% of cases and is more common when the implantation is in the isthmus. Whereas the rupture of the ampulla usually occurs between the sixth and 10th weeks, rupture of the isthmus occurs earlier, frequently at the time of the first missed period. The trophoblast burrows deeply and eventually erodes the serosal coat of the tube, the final break being sudden or gradual. Usually the ovum is extruded through the rent and bleeding continues. If the rupture is on the mesenteric side of the tube, a broad ligament haematoma will form (Fig. 12.3).
CLINICAL ASPECTS
The possibility of an ectopic gestation should always be considered in a woman of childbearing age, especially if there is a past history of acute salpingitis. The history (Box 12.1) is of greater importance than the physical signs, as these can be equivocal. Usually there is a short period of amenorrhoea, although in 20% of cases this may not be present. The pain is lower abdominal in site, but not distinguishable from that of abortion. However, in ruptured ectopic gestation fainting usually occurs, although this may only be momentary. Vaginal bleeding follows the pain, and may be mistaken for bleeding due to a delayed menstrual period or an abortion. The bleeding is a slightly brownish colour and continuous, and clots are rarely present (Table 12.1).
| SYMPTOM/SIGN | % |
|---|---|
| Abdominal pain | 90 |
| Amenorrhoea | 80 |
| Adnexal tenderness | 80 |
| Abdominal tenderness | 80 |
| Vaginal bleeding | 70 |
| Adnexal mass | 50 |
DIAGNOSIS
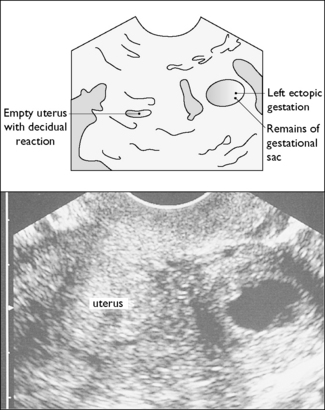
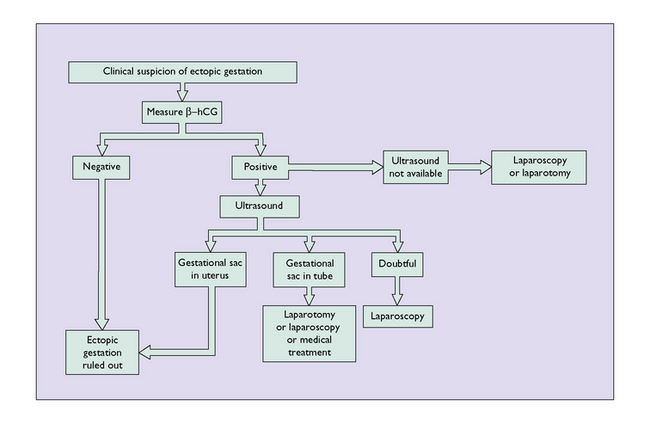
Although in acute cases the presence of internal bleeding is obvious and the diagnosis not in doubt, in subacute cases the diagnosis can be extraordinarily difficult. Laboratory tests may help, but in most instances they are not particularly informative. A radioimmunoassay for serum levels of β-human chorionic gonadotrophin (β-hCG) should be made. A negative result (<5 IU/mL) indicates that the woman is not pregnant, and ectopic gestation can be excluded. If the β-hCG test is positive a pelvic ultrasound examination should be performed, preferably using a transvaginal probe. A fetal heartbeat should be detectable once the β-hCG level reaches 1500 IU. If this shows an empty uterus (Fig. 12.4), and particularly if it shows a sac and fetus in the Fallopian tube, the diagnosis is certain. and treatment should be commenced. If the ultrasound is equivocal serial measurements of β-hCG should be taken. The levels should double every 48 hours, a rise less than 66% being suggestive of an ectopic gestation. On the other hand, if ultrasound shows an intra-uterine pregnancy, a concurrent ectopic pregnancy is extremely unlikely. Routine serum progesterone levels can help to exclude an ectopic pregnancy (>79 nmol/L) and identify a nonviable pregnancy (>15.9 nmol/L).
The diagnosis of suspected ectopic gestation is summarized in Figure 12.5.