CHAPTER 9 External Snapping Hip Syndrome
The snapping hip, or coxa saltans, is characterized by a snapping phenomenon that occurs around the hip in association with hip motion. It has been classified into three different types1:
HISTORY AND PHYSICAL EXAMINATION
In some cases, the snapping phenomenon may be visible under the skin and, in some other cases, it may be palpated over the area of the greater trochanter. In symptomatic patients, the snapping phenomenon is accompanied by pain in the area of the greater trochanter. The snapping phenomenon is always voluntary and the patient often volunteers to demonstrate it.1 Asymptomatic snapping (snapping without pain) must always be considered a normal occurrence.4 Clinical diagnosis is evident; the snapping will occur with flexion and extension of the hip. The snapping phenomenon is also described by some patients as the ability to “dislocate the hip.” This is often demonstrated by actively rotating the affected hip while tilting the pelvis in standing position. The voluntary dislocators are more frequently painless and should only be treated with stretching exercises of the iliotibial band. Symptomatic external snapping hip syndrome is always accompanied with pain and tenderness in the posterior greater trochanteric region. The pain is often secondary to greater trochanteric bursitis and may also be related to tendinosis of the trochanteric insertion of the gluteus medius. When Trendelenburg gait is also found, an associated abductor muscle tear must be suspected; this is an indication for surgical treatment.
DIAGNOSTIC IMAGING
Anteroposterior pelvis x-rays should always be done to identify bony abnormalities, calcifications, or other pathology. The snapping phenomenon can be documented with dynamic ultrasonography and associated pathology such as tendinitis, bursitis or muscle tears can be detected.5,6 Iliopsoas bursitis and abductor muscle tears can be diagnosed using magnetic resonance imaging (MRI).7,8
TREATMENT OPTIONS
Conservative Treatment
Most symptomatic cases improve with stretching physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroid infiltration of the greater trochanter bursa.1 When conservative treatment fails, surgical release is indicated. Open iliotibial band release or lengthening has been the traditional surgical option to treat the external snapping hip syndrome.9–12 Recently, we have described a technique for endoscopic iliotibial band release for the treatment of external snapping hip syndrome13 that provides access to the peritrochanteric space.
Arthroscopic Technique
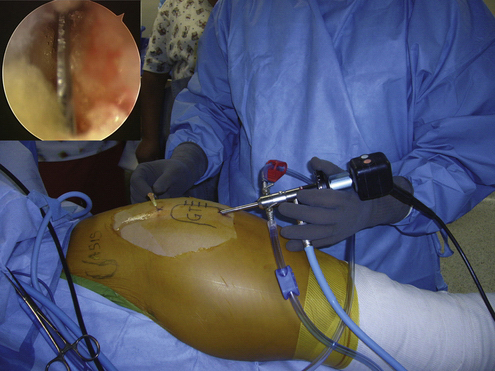
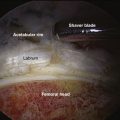
The patient is positioned laterally, similar to the setup for total hip replacement. Surgical drapes must allow for free range of motion of the lower extremity so that the snapping phenomenon is reproduced with flexion and extension of the hip. Snapping usually occurs with flexion of more than 90 degrees. Reproduction of the snapping phenomenon during surgery is important to evaluate when the release of the iliotibial band is complete (Figs. 9-1 and 9-2). No traction is necessary to access the peritrochanteric space, greater trochanteric bursa, and iliotibial band. When there is a combination of periarticular pathology and hip joint pathology, arthroscopic access to the hip joint is necessary. The patient is positioned for hip arthroscopy, preparing for traction to access the central compartment and dynamic positioning for the hip periphery. I favor the lateral position for hip arthroscopy. When arthroscopy of the hip joint is complete, the foot is taken out of the traction device, the perineal post is lowered, and the peritrochanteric space is accessed. This allows for flexion and extension for reproduction of the snapping phenomenon. A more recent positioning method for hip arthroscopy is the Spider device (Tenet Medical, Calgary, Canada) which allows for full range of motion without releasing the foot for the traction device (Figs. 9-3 and 9-4).

FIGURE 9-2 Hip flexion. It is necessary to flex the hip up to 90 degrees to reproduce the snapping phenomenon.

FIGURE 9-3 Patient positioned in lateral decubitus position for arthroscopy of the left hip. Note the horizontal perineal post and the traction device attached to the Spider positioner (Tenet Medical, Alberta, Canada). The image intensifier is horizontally positioned under the table to provide an anteroposterior view of the left hip.
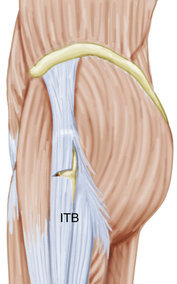
The greater trochanter is the main landmark for portal placement and is marked on the skin using a skin marker. I use two portals, a proximal trochanteric and distal trochanteric. The area of snapping should be between both portals to ensure that iliotibial band release will include the area that generates the problem. We also mark the area of snapping on the skin (Fig. 9-5). We start by infiltrating the space under the iliotibial band with 40 to 50 mL of saline. Next, the inferior trochanteric portal is established using a standard arthroscopic cannula that is introduced under the skin. It is directed proximally to the site of the superior trochanteric portal using the blunt obturator to develop a working space above the iliotibial band. The obturator is exchanged by a 4.0-mm 30-degree arthroscope and the inferior trochanteric portal used as the viewing portal. The site of the proximal trochanteric portal is identified arthroscopically using a needle inserted at the portal landmark (Fig. 9-6), the skin incision is made, and a shaver is introduced to dissect subcutaneous tissue from the iliotibial band situated between the portals (Fig. 9-7). Hemostasis is performed in this step to allow clear visualization of the iliotibial band. A radiofrequency hook probe is then introduced from the proximal trochanteric portal and a 4- to 6-cm vertical retrograde cut is made on the iliotibial band starting at the level of the inferior trochanteric portal and ending at the level of the superior trochanteric portal (Fig. 9-8). The pump pressure should be kept low while working on the subcutaneous space to avoid skin complications.

FIGURE 9-5 Illustration of portals. The anterior superior iliac spine (ASIS) and greater trochanter (GT) have been outlined. The proximal trochanteric portal is superior to the top of greater trochanter and the distal trochanteric portal is inferior to the tip of the greater trochanter. The snapping area must be between the portals. In this case, the snapping area is indicated by horizontal lines. Note how a transparent adhesive dressing has been used to prevent fluid from accessing the patient. A portion of the transparent adhesive dressing has been removed from the surgical area to prevent plastic material to be brought in through the portals.
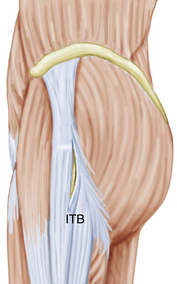
FIGURE 9-8 Vertical cut of the iliotibial band (ITB) above the area of the greater trochanter on a left hip.
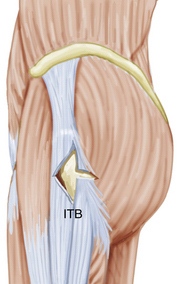
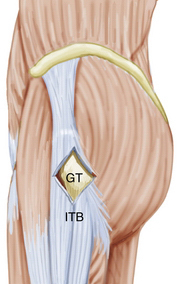
Once the vertical cut on the iliotibial band is complete, the pump pressure can be increased and a transverse anterior cut of 2 cm long is made, starting at the middle of the vertical cut (Fig. 9-9). The resulting superior and inferior anterior flaps are resected using a shaver to develop a triangular defect on the anterior iliotibial band that will provide access to the posterior iliotibial band (Figs. 9-10 and 9-11). Next, a transverse posterior cut is started at the same level of the transverse anterior cut. This is the most important release and should be carried out until the snapping phenomenon is eliminated. Finally, the superior and inferior posterior flaps are resected, which results in a diamond-shaped defect on the iliotibial band (Figs. 9-12 and 9-13). The greater trochanter will rotate freely within the defect without snapping. The greater trochanteric bursa should be removed through the defect on the iliotibial band and the abductor tendons inspected for tears (Fig. 9-14).
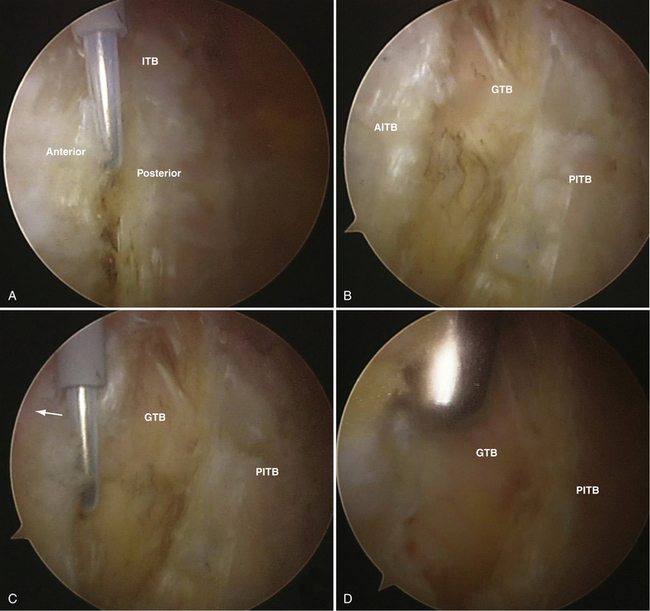
FIGURE 9-11 Endoscopic sequence of an iliotibial band release for external snapping hip syndrome in a left hip, anterior release. A, Vertical release is performed, resulting in anterior and posterior margins of the iliotibial band (ITB). B, When the vertical release is complete the greater trochanteric bursa (GTB) is visible through the defect between the anterior margin of the iliotibial band (AITB) and the posterior margin of the iliotibial band (PITB). C, Direction of the anterior cut at the midportion of the vertical release on the anterior margin of the iliotibial band (arrow). The GTB and PITB are observed behind the radiofrequency hook. D, A mechanical shaver is used to resect the superior and inferior flaps after the anterior transverse release is completed. Note the triangular defect on the iliotibial band. The GTB is visible through the defect. To the right is the PITB.
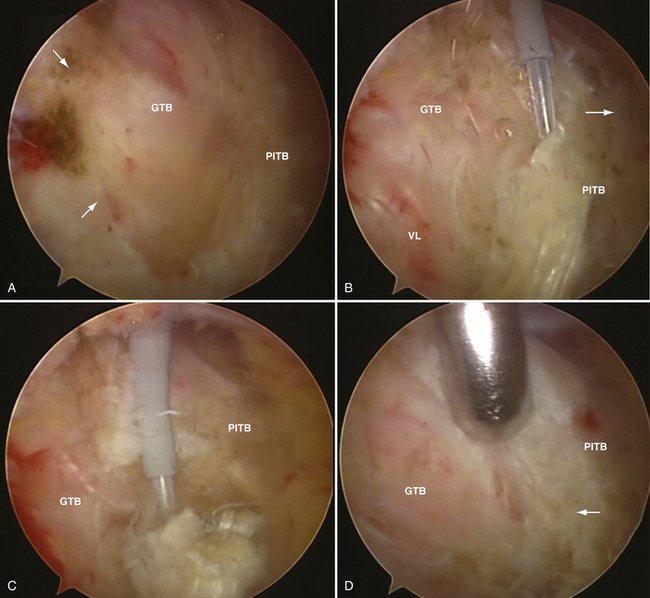
FIGURE 9-12 Endoscopic sequence of an iliotibial band release for external snapping hip syndrome in a left hip, posterior release. A, Triangular defect is observed on the iliotibial band after the flaps forming the anterior transverse cut have been removed. The edges of the anterior release can be seen (arrows). The greater trochanteric bursa is visible through the defect and the posterior margin of the iliotibial band (PITB) is the base of the triangular defect. B, Radiofrequency hook probe used to perform the posterior transverse release at the midportion of the PITB. The direction of the cut is shown (arrow). The greater trochanteric bursa (GTB) and some fibers of the vastus lateralis (VL) are observed through the defect. C, The posterior transverse release of the PITB is complete. The greater trochanteric bursa is visible through the defect. D, Shaver is used to remove the superior and inferior flaps of the posterior transverse release on the PITB. The apex of the posterior release forming the posterior tip of the diamond-shaped defect can be seen (arrow). The GTB is observed through the defect.
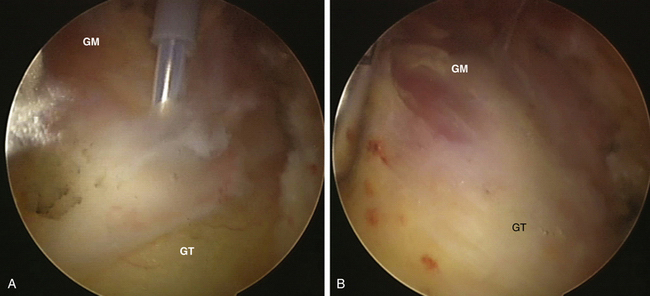
FIGURE 9-14 Endoscopic photographs demonstrating a greater trochanteric bursectomy of a left hip. A, The greater trochanteric bursa is removed using a radiofrequency hook probe. The area is visualized and accessed though a diamond-shape released of the iliotibial band. The greater trochanter (GT) covered by the insertion of gluteus medius and vastus lateralis is at the bottom. Distal fibers of the gluteus medius (GM) are observed through the bursa at the top. B, After resection of the greater trochanteric bursa, the insertion of the GM is clearly observed on the GT. No tears are seen.
PEARLS& PITFALLS
PEARLS
PITFALLS
RESULTS
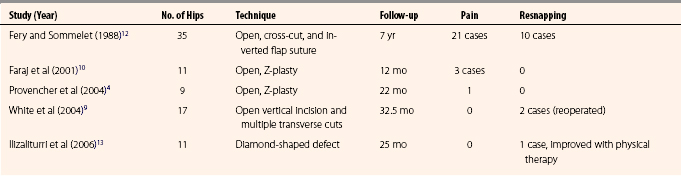
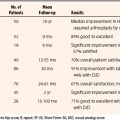
Published literature on the results of surgical treatment of the external snapping hip syndrome is limited. Most reports have been about open releases of the iliotibial band and the evidence is anecdotal.9–12 Recently, our group reported the results of an endoscopic technique to release the iliotibial band with greater trochanteric bursectomy and examination of the abductor tendons.
A summary of the results of open and endoscopic techniques for iliotibial band release in the treatment of external snapping hip syndrome is presented in Table 9-1. There is little information about the results of the endoscopic technique, but they compare well with the reported results of open surgical procedures.
CONCLUSIONS
Only recently has endoscopic management of symptomatic external snapping hip syndrome been reported.13 I have found this procedure to be safe and reproducible. Appropriate patient selection is an important factor for ensuring good results of surgical treatment.
1. Allen WC, Cope R. Coxa saltans: the snapping hip revisited. J Am Acad Orthop Surg. 1995;3:303-308.
2. Binnie JF. Snapping hip (Hanche a resort; Schnellend Hefte). Ann Surg. 1913;58:59-66.
3. Byrd JWT. Evaluation and management of the snapping iliopsoas tendon. Tech Orthop. 2005;20:45-51.
4. Provencher MT, Hofmeister EP, Muldoon MP. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med. 2004;32:470-476.
5. Pelsser V, Cardinal E, Hobden R, et al. Extra-articular snapping hip: sonographic findings. AJR Am J Roentgenol. 2001;176:67-73.
6. Choi YS, Lee SM, Song BY, Paik SH, Yoon YK. Dynamic sonography of external snapping hip syndrome. J Ultrasound Med. 2002;21:753-758.
7. Wunderbaldinger P, Bremer C, Schellenberger E, et al. Imaging features of iliopsoas bursitis. Eur Radiol. 2002;12:409-415.
8. Cvitanic O, Henzie G, Skezas N, et al. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am J Roentgenol. 2004;182:137-143.
9. White RA, Hughes MS, Burd T. A new operative approach in the correction of external coxa saltans. Am J Sports Med. 2004;32:1504-1508.
10. Faraj AA, Moulton A, Sirivastava VM. Snapping iliotibial band. Report of ten cases and review of the literature. Acta Orthop Belg. 2001;67:19-23.
11. Brignall CG, Stainsby GD. The snapping hip: Treatment by Z-plasty. J Bone Joint Surg Br. 1991;73:253-254.
12. Fery A, Sommelet J. The snapping hip: Late results of 24 surgical cases. Int Orthop. 1988;12:277-282.
13. Ilizaliturri VMJr, Martinez-Escalante FA, Chaidez PA, Camacho-Galindo J. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy. 2006;22:505-510.