Chapter 37 Expansion sphincter pharyngoplasty
1 INTRODUCTION
Snoring results from the vibration of the soft tissues in the oral cavity – the soft palate, uvula, tonsils, base of tongue, epiglottis and lateral pharyngeal walls. These vibrating soft tissues when subjected to negative pressure within the upper airway may lead to collapse of the upper airway. It is known that when inspiratory transpharyngeal pressure exceeds the pharyngeal dilating muscle action, apneas and hypopneas occur.1 Collapse of the upper airway is usually multilevel, at the level of the velopharynx, the base of tongue, and the lateral pharyngeal walls. Many patients with obstructive sleep apnea (OSA) have bulky thick lateral pharyngeal walls that vibrate and contribute to the collapse of the upper airway in these patients. The level of collapse is assessed using the Mueller maneuver recorded with fiberoptic flexible nasopharyngoscopy. The Mueller maneuver is usually graded on a five-point scale, 0 to 4.2 Terris et al. described the Mueller maneuver finding based on three levels: soft palatal collapse, lateral pharyngeal wall collapse and base of tongue collapse.3 Lateral pharyngeal muscle wall collapse has been demonstrated to be important in the pathogenesis of OSA in imaging studies.4,5 It is well known that lateral pharyngeal wall collapse plays a significant role in the pathogenesis of OSA. Most authors concur that it is difficult to create, surgically, adequate lateral pharyngeal wall tension to prevent its collapse.
Lateral pharyngoplasty, first described by Cahali,1 was aimed at addressing lateral pharyngeal wall collapse in patients with OSA. The procedure showed promising results; however, many patients had prolonged dysphagia postoperatively.
Orticochea6 first described the construction of a dynamic muscle sphincter, by isolating the palatopharyngeus muscle and transposing it bilaterally, superiorly in the midline, for treatment of velopharyngeal incompetence in patients with cleft palates. Christel et al.7 modified Orticochea’s procedure, by isolating the palatopharyngeus muscle bilaterally, apposing it more superiorly and closing the lateral pharyngeal defects with Z-plasty sutures. Utilizing these procedures, the authors present an innovative technique in creating this tension in the lateral pharyngeal walls, preventing its collapse and reducing the number of apneic episodes. The expansion sphincter pharyngoplasty basically consists of a tonsillectomy, expansion pharyngoplasty, and rotation of the palatopharyngeus muscle, a partial uvulectomy and closure of the anterior and posterior tonsillar pillars.
2 PATIENT SELECTION
The authors conducted a prospective randomized clinical trial in 45 adults, age above 18 years old, who have mainly type I Fujita (retropalatal obstruction) and lateral pharyngeal wall collapse. The inclusion criteria included patients with small tonsils (tonsil size 1 and 2), Body Mass Index (BMI) < 30, and Friedman clinical stage II and III who had failed or cannot tolerate nasal continuous positive airway pressure (CPAP) therapy. The clinical examination included height, weight, neck circumference, BMI, and assessment of the nasal cavity, posterior nasal space, oropharyngeal area, soft palatal redundancy, uvula size and thickness, tonsillar size and Friedman tongue position. Flexible nasoendoscopy was performed for all patients, and collapse during a Mueller’s maneuver was graded for the soft palate, lateral pharyngeal walls and base of tongue on a five-point scale.3 These patients were randomized into either the traditional uvulopalatopharyngoplasty (UPPP) procedure or the expansion sphincter pharyngoplasty (ESP). The mean follow-up time was 6.5 months. All patients had a postoperative polysomnogram at 6 months.
3 SURGICAL TECHNIQUE
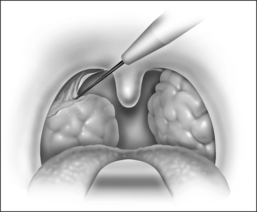
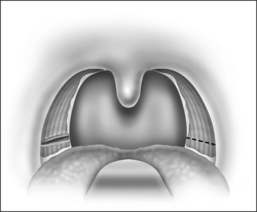
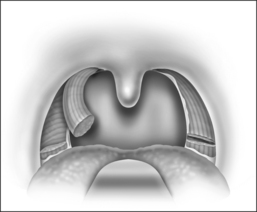
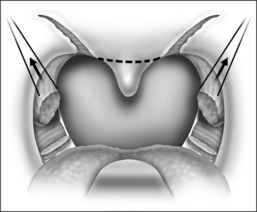
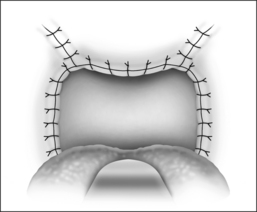
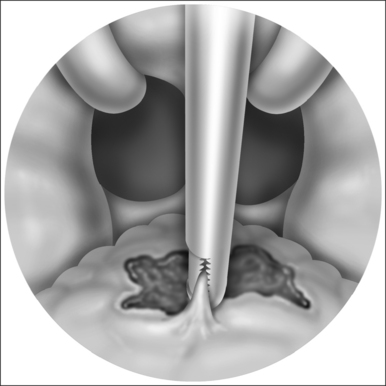
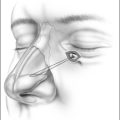
The procedure is done under general anesthesia, with the patient in the supine position. The authors perform the procedure with orotracheal intubation, and a Boyle–Davis mouth gag within the oral cavity keeping the mouth open, and isolating the endotracheal tube forwards. A bilateral tonsillectomy is performed (Fig. 37.1). The palatopharyngeus muscle is identified; its inferior end is transected horizontally (Fig. 37.2). The muscle is isolated and left with its posterior surface partially attached to the posterior horizontal superior pharyngeal constrictor muscles (Fig. 37.3). It is rotated superolaterally with a figure 8 suture, through the muscle bulk itself, with a Vicryl 3/0 round body needle. A superolateral incision is made on the anterior pillar arch bilaterally, identifying the arching fibers of the palatoglossus muscles (Fig. 37.4). The palatopharyngeus muscle is then attached to the arching fibers of the soft palate anteriorly and a partial uvulectomy is then performed (Fig. 37.5). The anterior and posterior tonsillar pillars are then apposed with Vicryl sutures (Fig. 37.6). The same steps are repeated on the opposite side. This new technique of expansion sphincter pharyngoplasty was modified from the Orticochea procedure and lateral pharyngoplasty. The principle of this technique is to isolate the palatopharyngeus muscle (the main part of the lateral pharyngeal wall bulk) and rotate this muscle supero-anterolaterally, in order to create the lateral wall tension and remove the bulk of the lateral pharyngeal walls. The key is to not completely isolate the muscle into a tube and rotate it, but rather to keep part of its fibrous attachment to the superior pharyngeal constrictor muscle, so as to create the necessary tension and pull supero-anterolaterally. A complete or partial uvulectomy is performed together with this procedure.
5 SUCCESS RATE OF PROCEDURE
The lateral pharyngoplasty technique, described by Cahali, showed that ten patients with moderate to severe OSA, and who had mainly lateral pharyngeal wall collapse noted on clinical endoscopic examination, had promising results.1 All ten patients had improvements in their AHI, with a mean of 45.8, reducing to 15.2 (P=0.009) postoperatively, with a mean follow-up of 8 months. There was also improvement in Apnea Index (AI), with a reduction from a mean of 22.4 to 4.8 (P=0.005). There were, however, significant swallowing problems in all ten patients who underwent this procedure. All patients had dysphagia; this ranged from 8 days to 70 days postoperatively (mean 20.4 days). One patient had persistent velopharyngeal insufficiency for up to 6 weeks. Another patient had permanent loss of taste for chocolate for 6 months. Cahali et al.9 compared lateral pharyngoplasty with the traditional uvulopalatopharyngoplasty in 27 patients with OSA. All 15 patients who underwent lateral pharyngoplasty achieved significant reduction in excessive daytime sleepiness, AHI and AI. There were also improvements in the REM sleep percentage and morning headaches in patients who had lateral pharyngoplasty, compared to those who underwent the traditional uvulopalatopharyngoplasty. They concluded that patients who underwent the lateral pharyngoplasty technique have better clinical and polysomnographic results.
1. Cahali MB. Lateral pharyngoplasty: a new treatment for OSAHS. Laryngoscope. 2003;113:1961-1968.
2. Borowiecki BD, Sassin JF. Surgical treatment of sleep apnoea. Arch Otolaryngol. 1983;109:506-512.
3. Terris DJ, Hanasono MM, Liu YC. Reliability of the Mueller maneuver and its association with sleep-disordered breathing. Laryngoscope. 2000;110:1819-1823.
4. Remmers JE, De Groot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol. 1978;44:931-938.
5. Schwab RJ, Gefter WB, Hoffman EA, et al. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385-1400.
6. Orticochea M. Construction of a dynamic muscle sphincter in cleft palates. Plast Reconstr Surg. 1968;41:323-327.
7. Christel SR, Georges B, Christel D, Jacques L, Bernard R, Patrick L, Jean-Louis P. Sphincter pharyngoplasty as a treatment of velopharyngeal incompetence in young people. Chest. 2004;125:864-871.
8. Schwab RJ, Gupta KB, Gefter WB, et al. Upper airway and soft tissue anatomy in normal subjects and patients with sleep disordered breathing: significance of the lateral pharyngeal walls. Am J Respir Crit Care Med. 1995;152:1673-1689.
9. Cahali MB, Formigoni GG, Gebrim EM, Miziara ID. Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep. 2004;27(5):844-846.