Exercise Testing and Training
Primary Cardiovascular and Pulmonary Dysfunction
The principles of physical therapy practice in the management of individuals with primary cardiovascular and pulmonary conditions can be applied in formally structured programs or in one-on-one sessions. Exercise testing and training are primary components of comprehensive physical therapy management, which is detailed in Chapter 31. This chapter describes these principles. Structured cardiac and pulmonary rehabilitation programs are therapeutic multidisciplinary programs that encompass the essentials of the best physical therapy practice (Box 24-1). The distinctions among structured programs lie in the primary patient populations they serve rather than in the principles of physical therapy management, which are comparable when applied on a one-to-one basis. The general principles of comprehensive care include teamwork, patient education, exercise testing and training, long-term sustainable lifestyle change, and follow-up, and these are common across patient groups. This chapter extends the basic principles of exercise testing and training outlined in Chapter 19. The chapter highlights state-of-the-art literature and the physical therapist’s central role as clinical exercise physiologist and health educator in addressing the needs of individuals with primary cardiovascular and pulmonary conditions.
Over the past decade, an extensive number of position statements, clinical practice guidelines, and consensus statements have been published to guide contemporary practice in cardiac and pulmonary rehabilitation programs. The major goal of these programs is to improve quality of life and tolerance of daily activities. An overriding objective is to institute lifelong healthy practices, including secondary prevention.1 The application of these principles is central to the management of cardiovascular and pulmonary conditions, whether they are primary or secondary conditions. In general practice today, patients (including children) presenting to the physical therapist with musculoskeletal or neuromuscular complaints have a high probability of having underlying cardiac or pulmonary pathology, or one or more associated risk factors (see Chapter 1). Established guidelines for cardiac rehabilitation programs do not replace the expert clinical judgment of rehabilitation professionals and goal-directed, patient-centered service delivery.2 Consistent with the World Health Organization’s definition of health (see Chapter 1), both cardiac and pulmonary rehabilitation programs focus on the enhancement and maintenance of cardiovascular and pulmonary health through individualized programs designed to optimize physical, psychological, social, vocational, and emotional status overall. In addition, they promote secondary prevention through risk-factor identification and modification in an effort to prevent disease progression and the recurrence of cardiovascular and pulmonary events.2
A criticism of conventional cardiac and pulmonary rehabilitation programs is that they are structured with little individualization.3 The physical therapist, who is uniquely qualified as an applied clinical exercise physiologist and health coach, needs to ensure that all components—in particular, exercise—are prescribed to meet the specific needs and comorbidities of each individual. For reference purposes, we include elements of international standards and guidelines for cardiac and pulmonary rehabilitation programs in Appendixes A and B. We caution, however, that these elements need to be tailored to an individual (based on a detailed history, assessment, and examination, and ongoing evaluation) and that such standards may change as new evidence emerges. Nonetheless, they will provide useful guidelines to physical therapists involved with setting up facilities related to cardiac and pulmonary rehabilitation.
This chapter extends the information in Chapter 31 concerning the management of chronic, primary cardiovascular and pulmonary dysfunction. In the review of the state-of-the-art literature,  was often reported in studies and was used to mean
was often reported in studies and was used to mean  (see Chapter 18 for elaboration of this physiological distinction). Despite this, we have retained the term used by the original investigators in each study in our summary of these studies.
(see Chapter 18 for elaboration of this physiological distinction). Despite this, we have retained the term used by the original investigators in each study in our summary of these studies.
Cardiac and Pulmonary Rehabilitation: Evidence Base, Efficacy, and Practicalities
Although an interprofessional team approach is fundamental to both cardiac and pulmonary programs, individuals who regularly participate in moderate exercise experience greater control of symptoms and increased functional capacity than do those treated with drugs alone.4 Self-management strategies learned in a pulmonary education program also contribute to perceived control of symptoms and to self-confidence.5 This sense of control is perhaps the single best argument supporting the exploitation of noninvasive interventions for the management of chronic conditions. This component may be singularly important in determining long-term outcomes, such as reduced demands for health care and lower health care costs.6
The effectiveness of cardiac and pulmonary rehabilitation has been established at the highest level of evidence2,7–19 and this is true irrespective of stage of disease.20,21 With the aging of the population, cardiac rehabilitation has been shown to benefit octogenarians as well as younger people. Because of the issues associated with exercise testing older people, the use of a mobility index, such as the Rivermead Mobility Index, to evaluate exercise performance has been proposed even in absence of a formal exercise test.22 Because of common lifestyle behaviors, ischemic heart disease as a primary lifestyle-related condition will remain prevalent for the foreseeable future.
These interprofessional programs have internationally recognized standards that are well described and are recommended for all patients with cardiovascular and pulmonary conditions. They specialize in patient education (including smoking cessation, nutrition and weight control, and promotion of self-management and training) that has sustained, lifelong, positive effects on cardiovascular and pulmonary status and sense of well-being.23–26 The term end stage needs to be revisited, given the efficacy of rehabilitation in severely compromised individuals.27 Considering these benefits and the enormous economic implications of keeping people healthy and out of hospitals and physicians’ offices, rehabilitation can be supported as a primary intervention rather than a secondary priority after suboptimal effects of pharmacotherapy or surgery.28
Noninvasive cardiac and pulmonary rehabilitation is more cost-effective than medical and surgical treatments, and it offers long-term health benefits and reduced risk. However, there is a significant discrepancy between the actual provision and practice of cardiac rehabilitation and that advocated in published guidelines. These evidence-based, noninvasive, cost-effective interventions are being grossly underused, and participation rates are low.29 Referral to cardiac rehabilitation has been reported to reflect selected groups, namely, younger age groups, those who have participated previously, those admitted to hospital with outpatient cardiac rehabilitation services, and those having a discharge diagnosis of myocardial infarction or coronary artery bypass surgery.30,31 Significant barriers also have been reported to exist with respect to availability, referral, and utilization of these programs; payment issues are another factor.32 Only a small proportion of individuals are referred, and of those, only a small proportion can access the programs.33–35 Phase I inpatient cardiac rehabilitation has been reported to be a declining trend.36 Physicians and surgeons may not have knowledge and awareness of the effectiveness of noninvasive approaches to health problems that have been managed primarily with drugs and surgery, so suitable candidates are not always referred.37 In addition, there are psychosocial reasons for underutilization of these resources. Women are referred less commonly than men, and their drop-out rates are higher.38,39 Thus there is a selection bias in the individuals sampled for studies of cardiac rehabilitation.40 The participation of women is associated with insurance, level of education, bypass surgery, and transportation availability.41 Cost containment and increasing accessibility are two primary barriers to participation in cardiac rehabilitation.42 Low participation rates (particularly by women, minority group members, and older people) and means of increasing access have become primary areas of interest.43
Of the multiple facets of a cardiac rehabilitation program, different components may have different effects on individual heart health. In addition, physiological distinctions between men and women affect the incidence and manifestation of cardiovascular conditions between the two sexes and, in turn, their responses to cardiac rehabilitation. Women tend to have lower systolic blood pressure and pulse pressure than men and to have more favorable lipid and homocysteine levels.44 However, the compliance of women’s small blood vessels tends to be lower, which may reflect female sex hormones and the higher mortality rates of premenopausal women hospitalized for myocardial infarction. Women also tend to have more “silent” ischemic heart disease than men, which is more often associated with sleep disturbance in women. The results of one descriptive study also showed that women were less likely to adhere to diet and exercise modification guidelines compared with regimens for smoking cessation, medication, and stress management.45
Special attention needs to be paid to motivating individuals to participate in rehabilitation programs (identify facilitating factors and barriers to participation), to generalize their new skills to home activities and the community, and to continue their new lifestyle behaviors beyond formal enrollment in the program.4 Given that education and exercise are core components of cardiac and pulmonary rehabilitation, physical therapy is uniquely positioned to implement care for individuals with cardiac or pulmonary conditions as primary or secondary diagnoses and to mobilize an interprofessional health care team for a given individual if no formal program exists. Education materials should be individualized to the learner’s needs and capacities; otherwise, resources will be wasted. A marked disparity exists between the average American’s reading ability (eighth grade level) and the readability levels of cardiac rehabilitation materials.46 The large number of polysyllabic words is a primary factor.
Cardiac and pulmonary rehabilitation programs are typically conducted in formal centers in large communities. The vast majority of patients, however, do not have access to cardiac and pulmonary rehabilitation. Furthermore, long-term participation and adherence to the principles of the program have been disappointing, particularly for women.47 The principles of these programs reflect fundamental physical therapy practice, which can be implemented on a one-to-one basis in a private practice (in a large or small community) or in a hospital that does not have a formal program in cardiac or pulmonary rehabilitation; in such settings, the outcomes are comparable to those in formal programs.48–50 A close-to-home philosophy of care is emerging in the field of health care, including cardiac rehabilitation, in an effort to improve access to underserved people and groups.51 When well constructed, a home-based cardiac rehabilitation program can have long-term outcomes comparable to those of a center-based program—for example, improved total cholesterol, smoking reduction, anxiety reduction, and self-reported improved physical activity and diet.52 Patients who are stable after bypass surgery do as well (in terms of improved exercise capacity and risk reduction) in an individualized detailed home program as those participating in a supervised center-based rehabilitation program.53
As patients become more active, their pharmacokinetics change. Medications must be reviewed on an ongoing basis and prescriptions modified accordingly.54 These changes reflect the long-term metabolic effects of exercise, in addition to improved health and potential weight loss. Close teamwork is needed to monitor a patient’s medications and ensure that drug prescriptions are changed so that they promote weaning from medication commensurate with the benefits of noninvasive intervention, including education and exercise. Eliminating or reducing the needs for medication and pharmacological support is an important physical therapy outcome consistent with the philosophy of exploiting noninvasive care as much as possible.
Formal exercise testing and training—primary physical therapy skills—are warranted in patient diagnosis, evaluation, and exercise prescription. Early intervention with exercise for heart and lung conditions has become an established practice to counter the deleterious effects of deconditioning and the loss of cardiac and pulmonary function and to maximize remaining oxygen-transport reserve.55
Addressing the psychosocial components of care in cardiac and pulmonary rehabilitation is an element of the internationally accepted definition of rehabilitation. Psychosocial factors, however, constitute few, if any, aspects of the workup and assessment of an individual with heart or lung disease. A structured assessment tool to assess and monitor psychosocial factors and changes in patients with heart disease has been proposed.56 Guidelines concerning the psychosocial component of cardiac rehabilitation are the sole focus of a position paper currently being developed in Europe. This position paper is designed to promote active psychological as well as physical well-being.57 Given the aging of the populations of high-income countries, cardiac rehabilitation programs must pay particular attention to the needs of older adults with respect to nutrition, physical activity and exercise, program adherence, smoking cessation, psychological issues, and methods of teaching the older learner.8 Doing so will help to reduce the high exclusion rate of this cohort of the population from cardiac rehabilitation programs.
Finally, with the advent of databases and outcome measures, projects such as the Wisconsin Society for Cardiovascular and Pulmonary Rehabilitation (WISCVPR) Web-based Outcomes Project, which focuses on outcomes for cardiac rehabilitation, are being used to develop benchmarks and further refine best practice guidelines.58 Outcomes of pulmonary rehabilitation include quality of life, which for those with chronic lung disease, is reflected in the St George’s Respiratory Questionnaire and the 36-item Short-Form Health Survey. A simple linear analog quality-of-life scale has also been shown to be valid in evaluating disease-specific, health-related quality-of-life issues in older individuals with chronic lung disease.59 With databases and outcomes evaluation, physical therapists will be able to individualize programs to promote more immediate, more effective, and more long-lasting effects.60 In addition, programs are being evaluated that will enhance the quality of prevention strategies initiated by health care providers through hospital-based programs for patients at risk.
Quality-improvement initiatives are becoming a focus in the literature. In 2008, one such initiative that used interactive training of hospital teams with Web-based teaching tools, enhanced adherence to prevention guidelines in hospitalized patients with cardiac disease.61 From baseline to 1 year, this initiative reported marked improvements in smoking cessation, lipid control, blood pressure control, and cardiac rehabilitation referral. Quality-improvement initiatives for activities related to cardiac rehabilitation produce marked benefits. In addition to structured exercise, cardiac rehabilitation focuses on counseling and teaching about risk reduction in order to promote lifelong health; however, long-term studies are needed to address the issue of deterioration with respect to risk factors and lifestyle behaviors over time.62 In 1998, a multistate outcome program for cardiovascular and pulmonary rehabilitation was shown to be feasible; it was possible to benchmark data across programs.21 Outcomes included the SF-36 Health Survey, a patient knowledge test, and a 6-minute-walk test distance. All outcomes improved in both cardiac and pulmonary rehabilitation programs. Such outcomes are needed to systematically evaluate the effects of cardiac and pulmonary rehabilitation programs.
Although cardiac rehabilitation reduces cardiac deaths, it remains unclear whether exercise alone or the comprehensive range of interventions associated with cardiac rehabilitation is responsible.63 The answer to this question is singularly important in refining the principles and practices of cardiac rehabilitation programs.
Studies of the efficacy of cardiac rehabilitation have been methodologically marred by selection bias: subjects tend to be low-risk, middle-aged men, whereas those who might benefit most are often excluded, namely, those who are older, at high risk, and have multiple comorbidities.63 Those individuals who do not attend cardiac rehabilitation programs tend to be older, less aware of their cholesterol values, and less likely than attenders to believe their condition was controllable and that their lifestyle may have contributed.64 Attention to exercise and motivational profiles has been proposed as a means of enabling rehabilitation program participants to continue with exercise.65 Promoting self-efficacy should therefore be an important focus in tailoring cardiac rehabilitation programs. Finally, the ethnicity of program participants is rarely reported. Given the needs of the aging population, the number of people with multiple conditions, and the increasing ethnic diversity in the United States and Canada, the reports on the effects of cardiac rehabilitation, to date, have relatively limited generalizability.
As a handy reference for clinicians, key points in the assessment, evaluation, and exercise testing and prescription of patients with primary cardiovascular and pulmonary conditions are summarized in Appendix C.
Patients with Chronic Cardiac Dysfunction: Exercise Responses
Cardiac dysfunction includes a range of types of pathology, causes (acquired or congenital), and severity that may be managed medically, surgically, or in both ways (see Chapter 31 for the principles of comprehensive physical therapy management). The most common cause is ischemic heart disease and myocardial infarction. The muscle that is infarcted never recovers, so remodeling of the heart occurs, and that alters the heart’s electrical functions (as shown on an electrocardiogram [ECG]) and mechanical functions (evidenced by ECG and echocardiogram). Remodeling takes place over time and with exercise. Ejection fraction (right ventricle) at rest is a poor indicator of cardiac function and exercise capacity.66 In fact, heart failure can occur in the presence of a normal ejection fraction,67 a form of disorder that typically occurs in women who have histories of hypertension and increased left ventricular mass.
Patients can range from being asymptomatic and having risk factors to being in severe distress and having minimal functional capacity, requiring high levels of supplemental oxygen and pharmacological support, and awaiting heart transplantation. Patients with extremely severe disease may require mechanical ventilation. To be able to classify patients’ functional capacity in a semi-quantitative manner, the New York Heart Association classification of function is commonly used (see Box 31-2). Exercise is now considered an essential component in the management of individuals with stable heart failure and in those who have undergone transplantation.68 Surgical options include keyhole surgery, open-heart surgery (e.g., coronary artery bypass surgery, valve repair, and aneurysm repair), and heart transplantation.
There is an interaction between circadian rhythms and the pathogenesis of heart rate and blood pressure variability. These rhythms are under the influence of adrenal, autonomic, hypothalamic, and pituitary activity. Thus physical exertion, sleep deprivation, emotional stress, and high-fat meals are major triggers of myocardial ischemia, angina, infarction, sudden cardiac death, and stroke, which have a higher incidence in the second quarter of the day, between 0600 and 1200.69 Heart rate and blood pressure variation have been implicated in the pathogenesis and progression of atherosclerosis, heart failure, and thrombosis, and are independent risk factors. During this period, vitamins C and E are lower than during the rest of the day; it has been postulated that regulating the intake of these vitamins and exercising may minimize the variability of heart rate and blood pressure. Whether such regulation can then modulate cardiovascular events warrants further study.
Although dyspnea is a common limiter to exercise in cardiac failure, the other factors that contribute to exercise limitation are multiple. In addition to central hemodynamic impairments, exercise capacity is affected by impaired ventilatory control, lung function, peripheral circulation, and skeletal muscle function.70 Exertional dyspnea has been attributed to the regulation of arterial pH during exercise.71 Pulmonary hypertension and systemic hypotension can also limit exercise performance.72 Explanations for these limiters include baroreceptor dysfunction, beta-receptor downregulation, abnormal vascular adaptation, and poor cardiac output in relation to elevated right ventricular afterload. The delayed  responses (delayed oxygen kinetics or time constant for this variable) are associated with lactate production and early anaerobiosis.73 Maladaptive gait changes have been ruled out as a factor influencing ventilation in patients with chronic heart failure.74
responses (delayed oxygen kinetics or time constant for this variable) are associated with lactate production and early anaerobiosis.73 Maladaptive gait changes have been ruled out as a factor influencing ventilation in patients with chronic heart failure.74
The physiological capacity of patients with cardiac dysfunction to adapt to exercise depends on the type and severity of impairment in the heart and in other steps in the oxygen transport pathway. Reduced alveolar-capillary membrane-diffusing capacity75 and a ventilation to perfusion mismatch have been proposed76 and may reflect chronically elevated pulmonary capillary pressure. A primary ventilation-perfusion mismatch defect in patients with heart failure may explain their increased ventilatory response to exercise, but this theory has been questioned.77 Patients with severe left ventricular dysfunction enhance their aerobic capacity primarily by improving oxygen extraction at the tissue level rather than by means of central adaptation. Similarly, with aerobic exercise, these patients improve the collateralization of peripheral capillaries so as to improve blood flow to working muscles and increase nitric oxide production in the blood vessels, which mediates endothelium-dependent relaxation.78 This effect is correlated with functional capacity. Thus evaluation of vasomotor reactivity has been proposed as a means of explaining the effects of interventions, including exercise and medications. Aortic wall elasticity modulates left ventricular function and coronary blood flow. Pulse wave velocity is a marker of arterial stiffness and is an independent predictor of  .79 The exercise intolerance observed in individuals with dilated cardiomyopathy may be explained by an increase in arterial stiffness.
.79 The exercise intolerance observed in individuals with dilated cardiomyopathy may be explained by an increase in arterial stiffness.
Although guidelines for exercise prescription have been commonly adopted for people with uncomplicated heart disease, the optimal prescription is still being refined. Moderate aerobic exercise performed alternate days for 20 to 40 minutes is generally accepted. Nonetheless, despite the general health benefits that are associated with this level of exercise, more moderate levels including brisk walking have been reported to be equally protective.80 Such findings are important particularly for individuals who are disinclined to formally exercise at the recommended level for cardioprotection. Brisk walking is more easily integrated into daily life hence likely to be adhered to.
Individuals with Chronic Cardiac Dysfunction and Failure
The cardiac dysfunction managed by physical therapists can range from mild to severe. With increasing severity of disease, an individual’s response and adaptation to exercise are altered markedly, which has major implications for exercise testing and training. Today, patients with even severe heart dysfunction may be able to participate in some level of exercise.19 However, this needs to be done under the supervision of a competent health care team to ensure the benefits are maximized and the risks minimized.
Chronic heart failure is usually hallmarked by left ventricular dysfunction. In health, normal left stroke volume coupled with increased heart rate leads to greater cardiac output and greater metabolic demand, as during exercise. As the left ventricle becomes increasingly compromised, the individual with heart failure depends more on heart rate to increase cardiac output and peripheral oxygen extraction. Left ventricular ejection fraction during exercise is not consistently associated with resting ejection fraction,81 even in people with objective signs of myocardial ischemia and increased heart rates during exercise. Thus the left ventricular ejection fraction at rest must be interpreted cautiously in the context of exercise and predicted exercise responses.
Determining which patients will benefit from a rehabilitation program has been the subject of debate. Goebbels and colleagues (1998)82 reported that patients with depressed left ventricular function benefit, whereas patients whose left ventricular function has been preserved, such as may occur after myocardial infarction and coronary artery bypass surgery, tend to improve spontaneously within 3 months.83 Proponents of selecting patients for cardiac rehabilitation however, have failed to address the past history of patients, their comorbidities, access to rehabilitation, return to work, and secondary prevention strategies to maximize their care and long-term outcomes. Noninvasive practices need to be exploited before, during, and after a myocardial event or surgery to maximize long-term gains, including reduced recurrence of the problem and need for doctor- and hospital-based care, reduced risk factors and morbidity, and prolonged quality of life. Physical therapy has a commitment to long-term outcomes, including reduced doctor- and hospital-based care, reduction or elimination of medications, and reduced probability of repeat surgeries.
Conservative management of patients with heart failure who utilize physical therapy has emerged as a major focus in the literature, in part because of the cost of surgery and an inadequate supply of organ donors. The benefits include reduction of deconditioning, including restoration of normal autonomic balance and, potentially, some primary effects on the underlying pathology.84 Patients with chronic heart failure respond to aerobic exercise favorably, showing improvement in functional class as defined by the New York Heart Association.85 Both  and anaerobic threshold improve. In addition, there is a reduction in the exaggerated ventilatory response at maximal and submaximal work rates that is usually observed in these patients. As a result, symptoms are reduced. Exercise benefits persist after patients shift from a supervised center-based to a home-based program. This finding has important practical and economic implications.
and anaerobic threshold improve. In addition, there is a reduction in the exaggerated ventilatory response at maximal and submaximal work rates that is usually observed in these patients. As a result, symptoms are reduced. Exercise benefits persist after patients shift from a supervised center-based to a home-based program. This finding has important practical and economic implications.
Over recent years attention has turned to exercise training of patients with cardiac failure and the role of ventilatory changes in exercise-induced dyspnea. The periodic breathing of patients with cardiovascular disease is well known clinically; however, the mechanism underlying the cycling hyperpnea and hypopnea is not clear. Fluctuations in pulmonary blood flow have been proposed as a mechanism for this periodic breathing.86 With respect to other ventilatory correlates of heart failure, ventilatory efficiency, the ratios of  and
and  , have yielded important prognostic information.87 When used in combination with
, have yielded important prognostic information.87 When used in combination with  (≥15 mL/kg/min),
(≥15 mL/kg/min),  (≥50 L/L) can be useful in defining a high-risk group that should be prioritized for heart transplantation.88
(≥50 L/L) can be useful in defining a high-risk group that should be prioritized for heart transplantation.88
At rest, individuals with more severe heart failure have more restrictive lung pathology and impaired gas exchange.89 During exercise, these patients have increased dead space, impaired gas exchange, and greater submaximal ventilatory responses than individuals whose disease is less severe. Exercise limitation in patients with chronic heart failure correlates with reduced FEV1 and FVC, implicating airway resistance in the increased work of breathing in exercise intolerance.90 In addition, an exercise-induced diffusion defect has been identified.91 Alveolar-capillary membrane conductance has been identified as the best lung function predictor of  in patients with chronic heart failure.92 The impairment in ventilatory efficiency is associated with reduced exercise tolerance and pulmonary artery pressures.93 Pulmonary vasoconstriction has been implicated in leading to pulmonary hypertension and alveolar hypoperfusion. Overall, exertional dyspnea observed in patients with heart failure is not the result of abnormal ventilatory function.94
in patients with chronic heart failure.92 The impairment in ventilatory efficiency is associated with reduced exercise tolerance and pulmonary artery pressures.93 Pulmonary vasoconstriction has been implicated in leading to pulmonary hypertension and alveolar hypoperfusion. Overall, exertional dyspnea observed in patients with heart failure is not the result of abnormal ventilatory function.94
Ventilatory exercise parameters, including  ,
,  , and
, and  , are strong predictors of mortality.95,96
, are strong predictors of mortality.95,96  , however, may be underestimated, given the slowed O2 kinetics in this population.97 Gas exchange, therefore, should continue to be monitored throughout recovery. Submaximal respiratory gas indexes have been proposed as being more sensitive than peak
, however, may be underestimated, given the slowed O2 kinetics in this population.97 Gas exchange, therefore, should continue to be monitored throughout recovery. Submaximal respiratory gas indexes have been proposed as being more sensitive than peak  for assessing functional impairment98 and for predicting survival in ambulatory patients with chronic heart disease.99 Nonetheless, ventilatory capacity is not likely to limit exercise performance in patients with stable chronic heart failure.100 Ventilatory and heart rate responses are, however, strong and powerful predictors of mortality in these patients, and they are superior to the use of
for assessing functional impairment98 and for predicting survival in ambulatory patients with chronic heart disease.99 Nonetheless, ventilatory capacity is not likely to limit exercise performance in patients with stable chronic heart failure.100 Ventilatory and heart rate responses are, however, strong and powerful predictors of mortality in these patients, and they are superior to the use of  .101 Inspiratory capacity varies inversely with pulmonary capillary wedge pressure in individuals with chronic heart failure, and it is a strong independent predictor of functional capacity.102
.101 Inspiratory capacity varies inversely with pulmonary capillary wedge pressure in individuals with chronic heart failure, and it is a strong independent predictor of functional capacity.102
Patients with severe chronic heart failure often have high ventilatory demands during exercise, and they have respiratory alkalosis, which is consistent with significant wasted ventilation on exertion,103 and increased respiratory drive;104 only a relatively small effect is attributed to ventilation-perfusion mismatch. However, increased ventilatory drive, as evidenced by the ventilatory equivalent of carbon dioxide ( ), has been reported to occur infrequently.105 Knowledge and understanding of which patients exhibit this response and which do not would be clinically useful.
), has been reported to occur infrequently.105 Knowledge and understanding of which patients exhibit this response and which do not would be clinically useful.
Patients with severe chronic heart failure have a reduced ratio of increase in  to increase in work rate during incremental exercise.106 The reduced DO2 due to severely compromised cardiac output is not fully compensated by an increase in oxygen extraction. These patients do tend to show improved exercise response through improved peripheral oxygen extraction. Changes in cardiac performance may reflect the Frank-Starling effect rather than changes in contractility.107 Low cardiac output, particularly in less intense exercise, does not necessarily result in lower exercise capacity.108 This phenomenon has been attributed to a unique mechanism that regulates arteriovenous oxygen content difference to optimize DO2 to the tissues in patients with severe heart failure. At peak exercise, fractional oxygen extraction in the muscle is greater in patients with chronic heart failure than in healthy people in proportion to the level of the patient’s impairment.109 This observation supports the importance of peripheral adaptation to aerobic training in patients with heart failure.
to increase in work rate during incremental exercise.106 The reduced DO2 due to severely compromised cardiac output is not fully compensated by an increase in oxygen extraction. These patients do tend to show improved exercise response through improved peripheral oxygen extraction. Changes in cardiac performance may reflect the Frank-Starling effect rather than changes in contractility.107 Low cardiac output, particularly in less intense exercise, does not necessarily result in lower exercise capacity.108 This phenomenon has been attributed to a unique mechanism that regulates arteriovenous oxygen content difference to optimize DO2 to the tissues in patients with severe heart failure. At peak exercise, fractional oxygen extraction in the muscle is greater in patients with chronic heart failure than in healthy people in proportion to the level of the patient’s impairment.109 This observation supports the importance of peripheral adaptation to aerobic training in patients with heart failure.
Heart failure can be categorized as either diastolic or systolic; the former may be the dominant form in elderly people.110 In stable outpatients, mortality due to diastolic failure is about half that of mortality due to systolic failure. However, when patients are hospitalized, the rates are comparable. Because of its strong prevalence among the elderly, diastolic failure exceeds systolic failure in being the cause of mortality. In diastolic failure, the Frank-Starling mechanism is impaired, causing reduced maximal cardiac output, heart rate, stroke volume, and left ventricular filling pressure. Vascular stiffness is also increased. Acute exacerbations result in pulmonary edema and are associated with hypertension, sodium intake, and lack of adherence to medication schedule. A primary goal is to reduce blood pressure, which improves symptoms and reduces exacerbations.
Exercise testing is an important means of establishing the prognosis of an individual with chronic heart failure with respect to treatment response, morbidity, and mortality. Peak  pulse, (
pulse, ( rate), and lean body mass adjusted for O2 pulse are useful prognosticators.111 Postexercise blood pressure response has shown to be a reliable and valid predictor of adverse cardiac events in individuals with dilated cardiomyopathy.112 The postexercise blood pressure response is defined as the ratio of systolic blood pressure at 3 minutes postexercise to that at peak exercise, with a criterion of 0.79 or greater to predict complications. The 6-minute walk test has been reported not to replace
rate), and lean body mass adjusted for O2 pulse are useful prognosticators.111 Postexercise blood pressure response has shown to be a reliable and valid predictor of adverse cardiac events in individuals with dilated cardiomyopathy.112 The postexercise blood pressure response is defined as the ratio of systolic blood pressure at 3 minutes postexercise to that at peak exercise, with a criterion of 0.79 or greater to predict complications. The 6-minute walk test has been reported not to replace  as a prognosticator in individuals with advanced heart failure.113
as a prognosticator in individuals with advanced heart failure.113
Prediction of the prognosis of individuals with chronic heart failure can be improved with a two-step exercise-test protocol.114 This test combines maximal and low-intensity exercise to improve accuracy and reproducibility. In addition, a distance of less than 300 meters walked in the 6-minute walk test (see Chapter 19) has been reported to be a useful prognostic marker of subsequent cardiac death in individuals with mild to moderate heart failure.115 Exercise testing has also been reported to provide good prognostic value in determining postoperative outcomes (mitral and aortic regurgitation).116 An important role for exercise testing in prognosis is emerging.
Although tests of  can be used to stratify patients with cardiac failure according to risk factors, these tests can be invalid as a result of premature termination by the tester or lack of motivation by the patient. Tests of anaerobic threshold may be less influenced by these factors in such a potentially compromised group.117 Rather, the combination of a
can be used to stratify patients with cardiac failure according to risk factors, these tests can be invalid as a result of premature termination by the tester or lack of motivation by the patient. Tests of anaerobic threshold may be less influenced by these factors in such a potentially compromised group.117 Rather, the combination of a  at an anaerobic threshold (gas exchange threshold) of less than 11 mL/kg/min and a
at an anaerobic threshold (gas exchange threshold) of less than 11 mL/kg/min and a  versus
versus  slope of more than 34 is a better predictor of mortality at 6 months than is
slope of more than 34 is a better predictor of mortality at 6 months than is  , and it may provide a guide when prioritizing patients for heart transplantation. Submaximal and endurance tests and determining the anaerobic threshold have been advocated over maximal tests for clinical evaluation of patients with heart failure because they are relatively easy to perform, are associated with less risk, and are more valid indexes of a patient’s capacity for daily activity.118,119
, and it may provide a guide when prioritizing patients for heart transplantation. Submaximal and endurance tests and determining the anaerobic threshold have been advocated over maximal tests for clinical evaluation of patients with heart failure because they are relatively easy to perform, are associated with less risk, and are more valid indexes of a patient’s capacity for daily activity.118,119
Individuals with heart failure have a higher incidence of glucose intolerance compared with healthy individuals (20% lower).120 After an aerobic exercise program, glucose uptake can increase by 25%. The mechanism of the reduction in glucose tolerance in individuals with heart failure and the remediating effects of aerobic exercise have yet to be elucidated. Whether secondary improvement in insulin sensitivity from aerobic exercise occurs in these individuals comparable to that in healthy people warrants clarification.
Body position may be an important factor to consider when exercising patients with chronic heart failure who often complain of orthopnea. However, when exercise responses in the erect and supine positions were compared in one study, no change was reported in breathlessness, and no change occurred in  . However,
. However,  was greater in the upright position.121
was greater in the upright position.121
Patients with chronic heart failure can benefit from aerobic training. Exercise training of patients with impaired left ventricular function is associated with improved ventilatory function.122 In addition to improved cardiac output, long-term high-intensity exercise resulted in reduced ventilatory dead space and improved ventilatory efficiency. In men with reduced left ventricular function, high-intensity exercise (2 hours of walking daily in combination with high-intensity, monitored cycle ergometry at 70% to 80% of peak capacity for 40 minutes, four times a week for 8 weeks) has been reported to result in marked increases in  secondary to increased cardiac output and widening of the A-aO2 difference.123 No improvement in myocardial contractility tends to be observed in these patients after such an exercise program. High-intensity exercise does not impair hemodynamic status or lead to further myocardial damage. Low-intensity exercise in individuals with chronic heart failure has been shown to improve autonomic tone and reactivity to vagal and sympathetic stimulation.124
secondary to increased cardiac output and widening of the A-aO2 difference.123 No improvement in myocardial contractility tends to be observed in these patients after such an exercise program. High-intensity exercise does not impair hemodynamic status or lead to further myocardial damage. Low-intensity exercise in individuals with chronic heart failure has been shown to improve autonomic tone and reactivity to vagal and sympathetic stimulation.124
The effects of exercise training on pulmonary function in individuals with heart failure are becoming better understood. After training, individuals with coronary artery disease have been reported to show no change in pulmonary function, with the exception of the respiratory exchange ratio at peak exercise.125 Also, alveolar-capillary diffusing capacity may contribute to improvement in exercise tolerance after training.126 Pretraining pulmonary function is not correlated with improvement in exercise performance.
With aerobic exercise training, respiratory muscle endurance improves, and that contributes to improved overall exercise capacity.127 Breathlessness is also reduced. The reverse occurs too—that is, respiratory muscle training can improve  , as well as respiratory muscle endurance in patients with chronic heart failure. The combination of muscle and endurance training is superior to endurance training alone in this patient cohort with respect to improved left ventricular function,
, as well as respiratory muscle endurance in patients with chronic heart failure. The combination of muscle and endurance training is superior to endurance training alone in this patient cohort with respect to improved left ventricular function,  , and strength.128,129
, and strength.128,129
An understanding of skeletal muscle function in individuals with chronic heart failure is important because improvements in aerobic capacity may be largely dependent on maximizing peripheral oxygen extraction. Strength training in combination with aerobic training improves walking distance in the 6-minute walk test, which is an independent prognosticator in individuals with chronic heart failure.130 Regular endurance exercise increases oxidative enzymes in the working muscles and is associated with a shift from type II to type I fibers.131 These skeletal muscle adaptations are independent of peripheral circulatory adaptations.
Adaptation to resistance muscle training reflects changes in the myosin heavy chain of peripheral skeletal muscle and a shift from slow aerobic to fast glycolytic and fast oxidative characteristics.132 These findings are associated with  , O2pulse, and tidal volume. Reduced strength of the knee flexors and extensors in patients with chronic heart failure is associated with impaired ventilatory response to exercise; thus muscle dysfunction has been proposed as a contributing factor to symptoms.133 Improved functional outcomes, increased walking distance, and reduced muscle area with increased interstitial space after exercise training support the theory that these effects are mediated by improved capillary density and flow reserve to exercising muscle.134
, O2pulse, and tidal volume. Reduced strength of the knee flexors and extensors in patients with chronic heart failure is associated with impaired ventilatory response to exercise; thus muscle dysfunction has been proposed as a contributing factor to symptoms.133 Improved functional outcomes, increased walking distance, and reduced muscle area with increased interstitial space after exercise training support the theory that these effects are mediated by improved capillary density and flow reserve to exercising muscle.134
Peripheral myopathy in individuals with chronic heart failure may contribute to exercise intolerance and training capacity.135 Features include reduced proportion of type I fibers, shift to type II fibers, biochemical shift consistent with increased muscle fatigability, reduced mitochondrial density, and reduced capillary density.136 However, some of these changes, such as altered capillary density, appear to be gender-specific, which may have implications for training.137 Skeletal muscle appears to adapt to central impairment of oxygen transport in heart failure. There is histochemical and gas exchange evidence showing that physiological recovery is delayed in patients with heart failure.138 Interestingly, markers of skeletal muscle oxygenation, including myoglobin and its derivatives, are reduced during incremental aerobic exercise to maximum, and during the recovery. As the capacity for aerobic exercise declines, patients may have greater reliance on anaerobic metabolism (but this cannot be sustained/attained in the same way), which is consistent with increasing reliance on anaerobic pathways for metabolism during exercise. Inflammatory cytokines have been implicated in the myopathy associated with heart failure.132 However, the possibility that this outcome reflects deconditioning cannot be ruled out because patients typically are unable to achieve high exercise intensities.139
The recovery process in patients with heart failure has important implications for optimizing exercise training parameters and, thereby, training effects. However, further study of differences in exercise recovery characteristics between patients with heart failure and healthy people is warranted.140,141 Evidence supports the idea that exercise intolerance in these patients is characterized by slower adaptation to acute exercise and recovery and to reduced maximal exercise capacity compared with healthy people.142
After angiography, positioning and mobilization have important roles after several hours of bed rest.143 Limiting restricted mobility after cardiac catheterization to 2 hours from 6 hours has been reported to be safe, and it may limit complications.144
Different types of exercise stress (aerobic or resistance) have differential effects on the heart and circulation.145 In health, for example, static exercise exerts a pressure load on the heart that can be distinguished from the normal hemodynamic response to dynamic exercise, which involves a volume load on the heart. Static exercise leads to concentric cardiac hypertrophy (left ventricular), and dynamic training is associated with eccentric hypertrophy. Static exercise can produce effects that have been associated with aerobic training. Isotonic exercise using hand weights has been reported to be associated with increases in systolic and diastolic blood pressure, rate pressure product, serum norepinephrine, and perceived exertion.146 Pulmonary capillary wedge pressure, incidence of dysrhythmias, and ST-segment changes do not differ from rates recorded at rest. Generally, isotonic exercise is tolerated well by individuals with heart failure, and no angina or dyspnea occurs.
Low to moderately intense strength training may cause fewer cardiovascular complications than aerobic exercise training in individuals who have undergone myocardial infarction.147 Resting blood pressure can be reduced, albeit to a lesser extent, suggesting reduced sympathetic and baroreceptor activity. In addition, lipid profiles may improve. These benefits can be observed in patients with cardiac and circulatory pathology without adverse effects. Even older, frail patients may tolerate weight training at 40% to 60% of maximal voluntary contraction. Qualitatively similar hemodynamic responses occur in response to resistance exercise, as in aerobic exercise in individuals with heart failure.148 In general, resistance training with multiple repetitions of moderate weight produces the most beneficial effects. To ensure that a patient is able to perform optimally the activities of daily living, which require a certain degree of muscle strength, strength training is considered an integral component of a cardiac rehabilitation program.
The effect of cardiac dysfunction on regional circulation has been of interest, particularly with respect to cerebral perfusion. A recent study has shown that patients with left ventricular dysfunction can have impaired cerebral perfusion. During exercise, the adequacy of cerebral perfusion is dependent on the adequacy of cardiovascular and pulmonary function; it is compromised in patients whose cardiac output fails to increase appropriately in response to exercise.149
Some individuals with chronic heart failure have been reported to have sick euthyroid syndrome, in which serum-free triiodothyronine is reduced in the presence of normal free L-thyroxin and thyrotropin.150 Sick euthyroid syndrome is a sign of poor prognosis in individuals with chronic heart failure. Exercise, however, can normalize the free triiodothyronine levels and reverse the syndrome, in turn improving exercise capacity.
Individuals with persistent life-threatening cardiac rhythms may require artificial pacemakers. Advances in this area have included biventricular pacing for individuals with systolic left ventricular failure with prolonged duration of the QRS complex. Preliminary reports suggest that these pacemakers are safe and effective.151 Further, biventricular pacing can improve symptoms and quality of life by improving walking times and ejection fraction.152 These effects persisted at the 6-month follow-up, and the 2-year survival rate was excellent. There are few specific guidelines for these individuals with respect to exercise testing and prescription. Similarly, there are few guidelines for individuals with automatic implantable cardioverter defibrillators.153 Preliminary reports suggest that exercise and lifestyle recommendations are needed for individuals with pacemakers and implanted cardioverter defibrillators and that with due modification, exercise testing and training are feasible.
Ventricular dysrhythmias contribute to a significant number of deaths. Despite improved survival, this cohort of high-risk individuals may be considered inappropriate for cardiac rehabilitation. With careful patient screening and monitoring, however, some patients with ventricular dysrhythmias may safely participate in cardiac rehabilitation.154
Individuals after Heart Transplantation
Heart transplantation has become an accepted therapy for end-stage heart failure over the past 20 years, with its ultimate goal being the return of function and a good quality of life (see Chapter 17). Postoperatively, the resting heart rate for heart transplant recipients is higher than normal. In the early postoperative period, the peak  and work rate of people who have had heart transplants are 50% of those of healthy people.155 At ventilatory threshold, the
and work rate of people who have had heart transplants are 50% of those of healthy people.155 At ventilatory threshold, the  and work rate were also 50% of normal. Peak heart rate, which increases for up to 3 minutes after peak exercise, is also significantly lower. This evidence supports the need for mandatory rehabilitation so as to maximize the benefits of this high-risk surgery, including optimizing functional work capacity, return to work, and life satisfaction.
and work rate were also 50% of normal. Peak heart rate, which increases for up to 3 minutes after peak exercise, is also significantly lower. This evidence supports the need for mandatory rehabilitation so as to maximize the benefits of this high-risk surgery, including optimizing functional work capacity, return to work, and life satisfaction.
Without training, exercise tolerance remains severely limited over the first 16 months postoperatively. This has been explained by the reduced capacity to respond to the Frank-Starling mechanism and the residual low cardiac index.156 Rehabilitation begins preoperatively and continues for 1 year after discharge.157 The principles of cardiac rehabilitation are applied; however, response of the denervated heart to exercise requires extended warm-up and cool-down periods and limits the maximal heart rate and  that can be achieved. Reinnervation of the sympathetic nerves to the heart is associated with improved heart rate response to exercise and contractile function.158 Hemodynamic responses to exercise are initially dependent on exogenous catecholamines rather than on the fast-responding sympathetic release from nerve endings. Systolic blood pressure is more appropriate than heart rate for assessing exercise response and recovery.159 Anaerobiosis is achieved early. The degree to which neuroplasticity can be influenced by exercise training to promote autonomic reinnervation to the heart after transplant has yet to be established.
that can be achieved. Reinnervation of the sympathetic nerves to the heart is associated with improved heart rate response to exercise and contractile function.158 Hemodynamic responses to exercise are initially dependent on exogenous catecholamines rather than on the fast-responding sympathetic release from nerve endings. Systolic blood pressure is more appropriate than heart rate for assessing exercise response and recovery.159 Anaerobiosis is achieved early. The degree to which neuroplasticity can be influenced by exercise training to promote autonomic reinnervation to the heart after transplant has yet to be established.
When compared with patients after bypass surgery in postoperative cardiac rehabilitation programs (phase II; up to 3 months postoperatively), patients with heart transplants have comparable functional outcomes.160 However, after graduation from this program and being on a home-based program for 9 months, patients with transplants had lower  and were significantly more limited at the 1-year follow-up. Thus phase I only, combined with recommendations for a home program, may be inadequate for patients after heart transplantation; they may benefit from long-term supervised training programs.
and were significantly more limited at the 1-year follow-up. Thus phase I only, combined with recommendations for a home program, may be inadequate for patients after heart transplantation; they may benefit from long-term supervised training programs.
Persistently low  after transplant reflects in part intrinsic skeletal muscle abnormalities.161,162 In addition to intensive aerobic exercise, resistance muscle training has an important role in countering the effects of corticosteroid-related osteoporosis and peripheral myopathy. With respect to predicting the prognosis of patients with heart failure who undergo heart transplantation,
after transplant reflects in part intrinsic skeletal muscle abnormalities.161,162 In addition to intensive aerobic exercise, resistance muscle training has an important role in countering the effects of corticosteroid-related osteoporosis and peripheral myopathy. With respect to predicting the prognosis of patients with heart failure who undergo heart transplantation,  is considered a superior indicator of submaximal indexes of exercise capacity.163
is considered a superior indicator of submaximal indexes of exercise capacity.163
Isometric exercise and activities requiring postural stabilization are largely avoided in people who have had heart transplants because of potential hemodynamic stress. Light isometric exercise (handgrip) attenuates increases in heart rate, blood pressure, and systemic vascular resistance. Whole-body isometric exercise also attenuates these hemodynamic variables.164 At rest, heart rate, blood pressure, and rate pressure product are higher in individuals who have had transplants than those rates in healthy people.
Some patients who receive heart transplants have low pulmonary diffusion capacity, and this is associated with lower exercise tolerance than is found in patients who do not have this impairment.165 Poor diffusion capacity, however, is not associated with exercise-induced hypoxemia and thus is not considered a primary contributor to impaired exercise tolerance.
Individuals with Left Ventricular Assist Devices
Left ventricular assist devices have become more common as an interim intervention for an individual awaiting heart transplant. The donor pool is small, so many individuals may not survive the wait for surgery. The Jarvik heart is a left ventricular device designed as a long-term solution for heart failure. In an initial case study describing a patient with a Jarvik heart, exercise tolerance, myocardial function, and end-organ function all improved 6 weeks after surgery.166 The Jarvik heart shows some promise for the management of end-stage heart failure; however, its success will depend on its mechanical dependability.
Individuals with Intermittent Claudication
Intermittent claudication (IC) is the symptom of exercise-induced muscle ischemia of peripheral arterial disease. IC is a systemic complication of atherosclerosis with or without overt ischemic heart disease. The disabling pain during walking results from muscle ischemia. The risk for cardiovascular morbidity and mortality far exceeds that of severe limb ischemia or limb loss.168 A patient with IC must be managed as a patient with heart disease as well as one with peripheral arterial disease. Conservative management is a priority and should include physical activity and exercise programs, smoking cessation, weight loss and optimal nutrition, and stress management.
Claudication symptoms may mask cardiac symptoms. In addition, a comorbidity such as arthritis can complicate the clinical picture in such a way that the underlying vascular condition is neither manifested peripherally nor centrally. During exercise testing and training, arthritis may limit the capacity of the patient who may have well been restricted by claudication pain.169 Even in this cases, exercise training can improve exercise tolerance in the absence of improved peripheral blood flow.169 Exercise effects include reduced submaximal heart rates and oxygen cost and reduced postexercise lactate levels. In addition, lipid profiles can be improved.
The exercise responses of patients with IC also exhibit a slowed  response related to impaired muscle perfusion.170 The associated delayed ventilatory response has been associated with the hyperemic response in the exercising muscle rather than with ischemia.
response related to impaired muscle perfusion.170 The associated delayed ventilatory response has been associated with the hyperemic response in the exercising muscle rather than with ischemia.
Outcome measures, including ankle-brachial index performed in a vascular laboratory to assess changes in peripheral stenoses with exercise training, are useful.171 Ultrasound can be used to assess pulses, particularly when they are weak. Palpation of skin temperature is a crude indicator of perfusion in that skin is highly sensitive to ambient temperature. Using the back of the hand, however, and scanning bilaterally down the legs, so that skin temperature can be compared in the legs, may have some utility for identifying gross differences in blood supply.
Individuals with Anemia
The exercise responses of patients with anemia have not been well described. The capacity of the blood to transport oxygen is determined by the hemoglobin concentration and the binding characteristics of the hemoglobin. Patients who develop acute anemia are more likely to complain of dyspnea than patients who develop anemia gradually. Rather than a primary cardiac, pulmonary, or muscle compensatory mechanism, this adaptation is mediated by increased diphosphoglycerate, which decreases the affinity of hemoglobin for oxygen in the tissue. Patients with sickle cell anemia have a low  and a low anaerobic threshold in the presence of a high heart rate reserve but no gas exchange abnormalities.172 The disease is characterized by restrictive lung pathology, increased alveolar dead space, and hypoxemia.173 Increased dead space may reflect impaired pulmonary capillary perfusion due to the sickle cells. Exercise hyperventilation is thought to be associated with increased anaerobiosis.
and a low anaerobic threshold in the presence of a high heart rate reserve but no gas exchange abnormalities.172 The disease is characterized by restrictive lung pathology, increased alveolar dead space, and hypoxemia.173 Increased dead space may reflect impaired pulmonary capillary perfusion due to the sickle cells. Exercise hyperventilation is thought to be associated with increased anaerobiosis.
Individuals with Hypertension
Hypertension remains the silent killer for which effective nonpharmacological interventions are underused. Hypertension is associated with sedentary lifestyle, diet, obesity, smoking, and stress. Further, hypertension has long been linked to type 2 diabetes mellitus as well as vascular changes typically seen with aging.174,175 Modifying one or more of these factors can reduce high blood pressure and its lethal sequelae and eliminate, or at least reduce, the need for medication. Chronic sympathetic overdrive associated with hypertension promotes left ventricular hypertrophy, cardiac dysrhythmias, and atherogenesis.176 Further, inhibiting sympathetic overactivity may help reduce cardiovascular risk. Regular physical activity and a formal exercise program reduce the risk for hypertension or modify it. This effect is likely mediated through a decrease in total peripheral vascular resistance. African American men are particularly at risk for hypertension, and this risk can be detected by an exaggerated blood pressure response to exercise.177 Endurance training reduces this exaggerated response and thereby may reduce the risk for developing hypertension. Along with eating a healthy low-salt diet and not smoking, exercise is a potent noninvasive intervention that can prevent, as well as control, high blood pressure. Despite the efficacy of many antihypertensive medications, potential deleterious effects of low perfusion to the vital organs with intensive blood pressure control cannot be overlooked clinically.178
Individuals with Type 2 Diabetes Mellitus
Type 2 diabetes mellitus is a strong risk factor for coronary artery disease and sudden cardiac death. This condition is associated with reduced baroreceptor sensitivity and heart rate variability, which are also risk factors for morbidity and mortality. Exercise training improves baroreceptor sensitivity in people with type 2 diabetes as well as glucose sensitivity, exercise tolerance, and muscle strength.179 Prognosis may well be improved with exercise.
Type 2 diabetes mellitus results in multiple deficits to exercise capacity, both central and peripheral. Muscle blood flow may be impaired at the level of microcirculation in the absence of overt peripheral vascular disease.180 In patients with chronic diabetes, exercise capacity is compromised by reduced oxygen delivery. A reduction in the arteriovenous oxygen difference may contribute to a reduction in  .181 When smoking is controlled, individuals with diabetes mellitus who are insulin dependent and have complications have been reported not to exhibit impaired pulmonary gas exchange during exercise despite thickening of the alveolar basal lamina.182 Individuals with non–insulin-dependent diabetes mellitus have reduced glucose transport in skeletal muscles, and this may contribute to exercise intolerance.
.181 When smoking is controlled, individuals with diabetes mellitus who are insulin dependent and have complications have been reported not to exhibit impaired pulmonary gas exchange during exercise despite thickening of the alveolar basal lamina.182 Individuals with non–insulin-dependent diabetes mellitus have reduced glucose transport in skeletal muscles, and this may contribute to exercise intolerance.
Diabetes mellitus is an independent risk factor for reduced left ventricular ejection fraction during exercise, as is severity of coronary artery disease.183
Role of Medications: Augmenters and Attenuators of Outcome
Among the factors that can confound exercise responses of patients are medications. Medications can enhance, limit, or have no effect on exercise performance. Patients with cardiovascular dysfunction, particularly those under a physical therapist’s care, are likely to be taking one or more potent medications. The timing of their ingestion of these medications in relation to their performing an exercise test should be recorded in order to standardize testing procedures from one time to the next; at the very least, it is important to be aware of the confounding effects of a medication that could explain improved or worsened responses. Beta blockers are commonly taken by patients with cardiac dysfunction to improve the rhythm and contractile force of the heart. Long-term use of beta blockers causes no significant improvement in delayed heart rate recovery, which is a predictor of mortality in patients with heart failure.184 These drugs can contribute to fatigue and exercise intolerance. Many patients are taking angiotensin-converting enzyme (ACE) inhibitors to enhance cardiac function. This classification of drug improves diffusion capacity and exercise capacity, an effect mediated through prostaglandin activity. However, this activity can be mitigated by aspirin, another drug commonly taken by patients with heart failure.185 Thus a change in aspirin administration in combination with ACE inhibitors can worsen exercise tolerance. Captopril, a commonly prescribed ACE inhibitor, has a demonstrable beneficial effect on exercise responses in patients after myocardial infarction.186 Ventilatory efficiency is improved, as is evidenced by a reduction in  at submaximal workloads. Reduced perception of exertion and improved capacity to perform the activities of daily living may result from a reduction in ventilatory demand. Concurrent with physical therapy management, an inventory of the patient’s medications and medication changes should be maintained and considered when conducting an exercise test or interpreting exercise test data.
at submaximal workloads. Reduced perception of exertion and improved capacity to perform the activities of daily living may result from a reduction in ventilatory demand. Concurrent with physical therapy management, an inventory of the patient’s medications and medication changes should be maintained and considered when conducting an exercise test or interpreting exercise test data.
Individuals with Chronic Pulmonary Dysfunction: Exercise Responses
Of individuals who participate in pulmonary rehabilitation programs, the largest proportion is made up of those with emphysema. Smoking is the primary cause of emphysematous changes in the lungs and the associated systemic complications (see Chapter 5). Patients with moderate or severe pulmonary distress may be referred to pulmonary rehabilitation. Other groups that may be referred are individuals with cystic fibrosis, asthma, interstitial lung disease, and alpha1-antitrypsin deficiency. Patients with lung cancer are typically underrepresented in rehabilitation programs and warrant being targeted as a group that could benefit.
Individuals with Chronic Obstructive Lung Disease
Deconditioning in patients with chronic lung disease is an anticipated consequence of the downward spiral of pathophysiological compensation for the structural and functional damage to the lungs. In individuals with severe disease, exercise intolerance may reflect limited peripheral perfusion and oxygen extraction due to the disproportionate demand on the respiratory muscles.187 These individuals are unable to exercise at an intensity that induces a high level of aerobic conditioning, and they experience early onset of dyspnea. On experiencing dyspnea with exercise, a person with chronic obstructive pulmonary disease (COPD) reduces his or her activity level, which leads to deconditioning. With impaired aerobic capacity, anaerobic glycolysis has an increasingly important role in supporting physical activity. This leads to increased blood lactate, which needs to be buffered with bicarbonate, thereby producing additional carbon dioxide. This further increases ventilatory load and dyspnea and leads to further inactivity and deconditioning. These individuals frequently have secondary cardiac and hematological changes. The goal of physical therapy is to relieve dyspnea and increase exercise tolerance, hence, quality of life. After smoking cessation, exercise is the single best intervention for controlling dyspnea in individuals with COPD.
Exercise testing has become an established component of the workup of an individual with impaired functional capacity, including patients with chronic lung disease. Although estimating the ventilatory capacity of patients with COPD on the basis of whether a patient can climb one or two flights of stairs is no longer considered a tenable test, symptom-limited stair climbing can be used to evaluate cardiovascular and pulmonary reserve.188 Stairs climbed in a symptom-limited stair-climbing test correlate with  ,
,  , heart rate, and respiratory rate in response to a maximal cycle ergometer test.
, heart rate, and respiratory rate in response to a maximal cycle ergometer test.
During acute exercise, patients with COPD have elevated heart rates and blood pressures and show increased hypoxemia and desaturation with incremental or prolonged constant work-rate exercise. Impaired exercise capacity reflects physical damage to the lungs, including impaired pulmonary vasculature189 as well as cardiac and skeletal muscle abnormalities. Exercise capacity is marked by a disproportionate ventilatory response and differences in FEV1, but these responses explain only a fraction of the variability in  .190 Variability in the ventilatory response to exercise is a primary determinant of variability in the exercise capacity of patients with COPD. In the absence of right heart failure, right ventricular end diastolic volume is highly correlated with
.190 Variability in the ventilatory response to exercise is a primary determinant of variability in the exercise capacity of patients with COPD. In the absence of right heart failure, right ventricular end diastolic volume is highly correlated with  and cardiac index in patients with COPD, suggesting that right ventricular end diastolic volume compensates optimally.191
and cardiac index in patients with COPD, suggesting that right ventricular end diastolic volume compensates optimally.191
As in other conditions, in the management of patients with COPD, individualized training programs based on heart rate as the gas exchange threshold (anaerobic threshold), as opposed to standard protocols based on 50% of heart rate reserve, produce superior therapeutic outcomes; that is, they reduce ventilatory requirements and are safer.192 Supervised training of individuals with COPD has been reported to have advantages over self-monitored exercise programs.193 When two to eight programs were compared, the supervised treadmill program was superior to a community-based walking program with respect to training intensity in terms of improved  ,
,  ,
,  , and heart rate in response to moderate-intensity workloads. Research is needed to design home-based programs for selected patients in order to maximize these programs’ effectiveness.
, and heart rate in response to moderate-intensity workloads. Research is needed to design home-based programs for selected patients in order to maximize these programs’ effectiveness.
The 6-minute walk test is useful in the assessment and management of patients with COPD, for whom the test was originally developed. The discriminating capacity of the test can be increased by considering factors in addition to walking distance. Four factors based on an evaluation of 15 variables accounted for 78% of the variances in distance walked:194
Based on a walking-distance test, the effect of an exercise program can be predicted on the basis of low pretraining walking distance and higher FEV1.195
Symptom-limited tests are used to estimate the effects of training on patients with COPD. In patients with low functional work capacity, objective submaximal indexes of training effects are useful. With respect to oxygen kinetics during constant work rate, the time constant of  after training is reduced, and it reverts after detraining.196 The O2 pulse similarly increases and decreases with training and detraining, respectively, and serum lactate decreases with training and increases with detraining.
after training is reduced, and it reverts after detraining.196 The O2 pulse similarly increases and decreases with training and detraining, respectively, and serum lactate decreases with training and increases with detraining.
Rigorous training (80% of peak work rate, for 45 minutes, 3 times a week, for 6 weeks) results in significant training responses in individuals with severe COPD.197 Peak work rate and exercise endurance increase. In response to constant work rate, the kinetics of O2 uptake, CO2 production,  , and heart rate are reduced. Improved exercise tolerance may reflect changes in breathing pattern, specifically, increased tidal volume and reduced respiratory rate.
, and heart rate are reduced. Improved exercise tolerance may reflect changes in breathing pattern, specifically, increased tidal volume and reduced respiratory rate.
Compared with healthy people matched for activity level, individuals with COPD have less muscle strength (70% to 80% of age-matched healthy people), which may be explained by deconditioning, a disease-related myopathy, or both.198 In addition, mechanical efficiency may be impaired. Patients have large numbers of less efficient type II muscle fibers, but cross-sectional fiber area, capillarization, and mitochondrial density are comparable or reduced.135,199 Although metabolic capacity is unchanged, differences in fiber type in COPD may explain the reduced mechanical efficiency.
Systemic factors contributing to exercise intolerance have been identified in individuals with chronic lung disease, and they appear to resemble those observed in individuals with chronic heart disease.200 Some individuals with COPD have impaired peripheral perfusion and oxygen extraction, which may be explained by the redistribution of cardiac output from the peripheral to the respiratory muscles during increasing work rates.187 This may be a primary exercise limiter in these patients. In a study designed to distinguish central from peripheral limitations in the exercise responses of patients with COPD, central factors rather than peripheral muscle limitations were reported to be responsible (although not wholly) for their exercise intolerance.201 Endurance training is associated with increased skeletal muscle activity and recruitment of slow-twitch fibers.202
Individuals with Primary Pulmonary Hypertension
Patients with primary pulmonary hypertension have impaired exercise responses that may resemble those of patients with COPD and secondary pulmonary hypertension. During incremental exercise, the lungs become less efficient as gas exchangers because of impaired lung perfusion.203
Individuals after Lung Volume Reduction Surgery
Lung volume reduction surgery has become a topic of increasing interest as an invasive means of correcting the hyperinflation in the lungs of patients with COPD. A good quality of life is correlated with reduced lung hyperinflation after surgery,204 and these improvements have been maintained for at least 18 months on follow-up.205 A commensurate reduced work of breathing appears to facilitate performance of activities of daily living. Improvement in functional capacity after surgery has been attributed to improved breathing mechanics during exercise, as well as at rest,206 and to improved respiratory muscle strength.207 Specifically, higher maximum levels of tidal volume and  are achieved; in turn, these lead to improvements in
are achieved; in turn, these lead to improvements in  and
and  .
.
Individuals with Interstitial Lung Disease
Performing exercise testing in individuals with interstitial lung disease can elucidate the extent of the pathology and its functional consequences—diffusing capacity and alveolar arterial oxygen tension difference.208 These patients have less ability than healthy people to recruit the pulmonary capillary bed during increased exercise stress, so they can desaturate readily.209,210  is correlated with impairment of gas exchange and circulation, rather than with ventilatory impairment. Thus the pathophysiology of the pulmonary vasculature is considered more important than impaired ventilatory mechanics in patients with interstitial lung disease.211 Abnormal exercise responses in individuals with pulmonary sarcoidosis may reflect subclinical right heart dysfunction.212
is correlated with impairment of gas exchange and circulation, rather than with ventilatory impairment. Thus the pathophysiology of the pulmonary vasculature is considered more important than impaired ventilatory mechanics in patients with interstitial lung disease.211 Abnormal exercise responses in individuals with pulmonary sarcoidosis may reflect subclinical right heart dysfunction.212
One study that examined the contribution of diffusion limitation to exercise performance in this patient group showed evidence of a ventilatory impairment that was manifested by a decrease in alveolar oxygen tension.213 Cardiac impairment such as impaired diastolic filling may occur secondary to pulmonary fibrosis during exercise or restriction of the pleurae and thoracic cavity. Changes in gas exchange during exercise may be the most sensitive indicator of physiological limitation in patients with subclinical evidence of interstitial lung disease.214,215 However, in terms of prognostic capability, the results of an exercise test for evaluating gas exchange do not appear to augment standard pulmonary function testing.216
Individuals after Lung Transplantation
Lung transplantation improves pulmonary function and quality of life in individuals such as those with cystic fibrosis. When exercise responses before and after bilateral lung transplantation are compared, exercise capacity remains low, although improved.217 This observation has been explained on the basis of poor oxygen extraction.218 Exercise conditioning is required in these patients postoperatively to maximize their functional capacity. However, maximum oxygen consumption may remain below that of healthy peers matched for age and gender, and anaerobiosis during exercise is achieved earlier. These responses reflect inadequate adaptation of cardiac output in these patients, as well as deconditioning.
Individuals with Asthma
There are several specific aspects to consider when testing and training individuals with exercise-induced asthma.219 For those who are managed with medication, a low-intensity warm-up before exercise can optimize its therapeutic effect. A longer cool-down may also be beneficial. Individuals with asthma are taught to monitor their unique responses to their medication and its coordination with physical activity and exercise. They also monitor the ambient air (humidity and temperature) to anticipate the potential for bronchoconstriction and respiratory distress. With good knowledge of conditions and medication, individuals with asthma can participate in high-intensity exercise safely.
Individuals with Cystic Fibrosis
General health and wellness have become primary goals for individuals with cystic fibrosis (CF) Twenty years ago, management of people with this condition, primarily children, was based largely on passive removal of excessive secretions by means of postural drainage and vigorous percussion. Now people with cystic fibrosis are living longer, and comprehensive physical therapy management, including a regular program of exercise, is recognized as a central component of promoting general health and airway clearance.220,221
Although life expectancy continues to improve in people with CF, end of life usually results from respiratory infection, so exacerbations have to be prevented. With a basis of good health resulting from proper nutrition and exercise, exacerbations may occur less often and last for a shorter time. The exercise program is adjusted during these times and then ramped up afterwards. Medications, including bronchodilators, are coordinated with exercise to produce the best effects both during sessions and over the long term.222
Cardiac and Pulmonary Rehabilitation: Common Components
Definition, Purpose, Goals, and Outcomes
Most individuals with heart or lung disease can benefit from the principles of healthful living that underlie the philosophies of conventional cardiac and pulmonary rehabilitation programs. In comparing patients participating in these programs with nonparticipants, cardiovascular deaths are reduced by 20% and sudden death by 37% in the year after infarction.223 Those who meet the criteria for admission and are within access of a center that offers these programs are evaluated by a multidisciplinary team that establishes the patient’s short- and long-term goals and sets up an overall program that includes exercise prescription, a nutritional plan, a smoking cessation program (if required), and life-skills and stress-management instruction. These programs are patient-focused, and the health care team, including the physical therapist, serves largely as health coaches and advisers. Fundamental to that program’s success is establishing an individual’s readiness to change lifestyle behaviors and participate in a lifelong program of health (see Chapter 1). The health education component of the program is then targeted to shift the individual to a higher level of readiness or to engage the individual immediately in an active rehabilitation program.
The preadmission workup for cardiac rehabilitation includes a complete history and a questionnaire related to current status and health behaviors and the individual’s goals (Figure 24-1). Because of the interdependence of heart and lung function, these questions are relevant to individuals being considered for admission to a pulmonary rehabilitation program, as well as to a cardiac rehabilitation program.
The relative benefit of structured programs as opposed to community and home-based programs is being debated. Maximizing the potential benefits of the program is key, so the program has to be optimal in terms of the individual’s needs, including the setting that will produce the best short- and long-term outcomes. Exercise gains have been demonstrated in healthy middle-aged people when programs are home-based.224 This evidence supports the idea that individuals with cardiovascular and pulmonary dysfunction who are being managed one-on-one by a physical therapist may also demonstrate benefits when the exercise program is home-based. However, further study is needed to determine the safety and effectiveness of home-based programs for candidates for cardiovascular and pulmonary rehabilitation.
The core components of cardiac and pulmonary rehabilitation programs are shown in Table 24-1; they reflect the skills and expertise of the multidisciplinary team in addressing each individual’s needs in a comprehensive manner. These components include awareness of the patient’s condition and health education overall, nutrition and weight control, smoking cessation, general physical activity and exercise, and stress management. Psychological support is important with respect to the patient’s adjustment to his or her condition; the management of anxiety, anger, hostility, and depression; and the maximization of adherence to recommendations and guidelines related to nutrition, physical activity and exercise, smoking cessation, and a lifelong health plan. Such support is elicited from the individual’s family and friends, as well as health care providers.
Table 24-1
Core Components of Cardiac and Pulmonary Rehabilitation
| Assessment | |
| History |
Present illness (medical and surgical details of management to date) Multisystem review (e.g., cardiovascular, peripheral vascular, pulmonary, musculoskeletal, neuromuscular, gastrointestinal, endocrine, renal, liver, immune) Lab tests and investigations: blood work, ECG, x-rays and scans, exercise test Learning assessment (education level, preferred learning styles, self-efficacy, and behavioral readiness to change. |
| Goals | |
| Interventions | |
| Outcomes (monitored over the short and long term and consistent with the individual’s goals) | |
| Structure and Function |
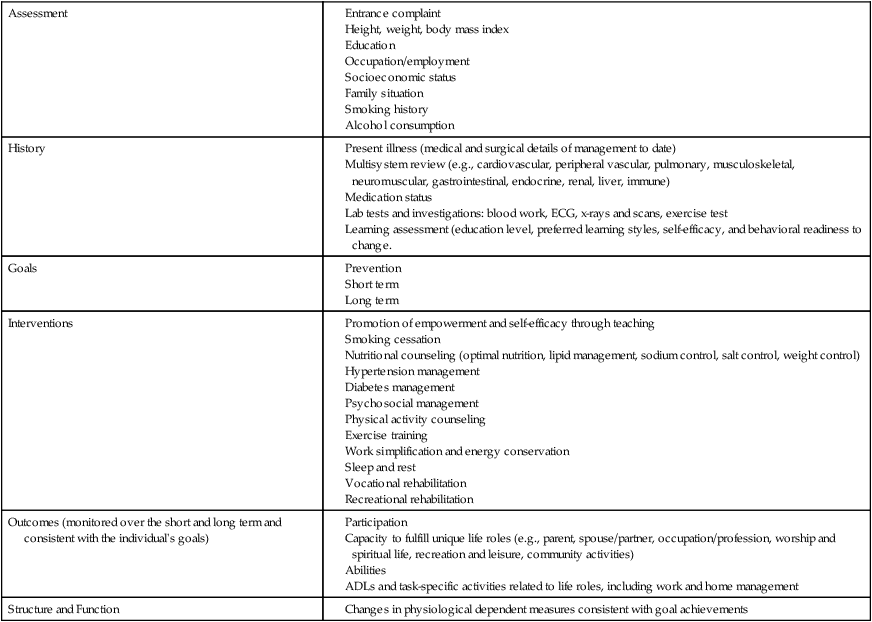
Modified from Balady GJ, Ades PA, Comoss P, et al: Core components of cardiac rehabilitation/secondary prevention programs, A statement for healthcare professionals from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation, Circulation 102:1069-1073, 2000.
Health education is a major component of cardiac rehabilitation and constitutes a skill in its own right. The patient requires knowledge about health and the incentive to translate this information into his or her own life. Each learner’s knowledge deficits are different and learning style is unique; these should be evaluated so that health education can be properly targeted to be the right type, the right level, the right format, and delivered at the right time (see Chapter 28). Knowledge deficits need to be established so that education can be targeted specifically to meet each deficit. For instance, individuals with coronary artery disease typically have little awareness of some of the major risk factors. Generally, their knowledge about cholesterol, use of lipid-lowering medications, and achievement of cholesterol levels consistent with consensus-based guidelines is minimal.225 Participation in structured cardiac rehabilitation programs improves knowledge related to heart disease, signs and symptoms, and self-management strategies. However, the learning and homework must be evaluated on each visit to determine how well the knowledge has been internalized and put into practice in daily life. Lifestyle recommendations should be suitable for application to daily living. For example, healthy food choices should be described specifically. Energy utilization should be translated into terms that are meaningful for the individual, such as 1000 kilocalories (kcal) of energy per week (although 1500 kcal/week has been identified as the threshold for reducing all-cause mortality risk226). People least likely to achieve the latter threshold include women, those with a body mass index of 30 or higher, and those who are 70 years of age or older. Weekly kilocalorie energy expenditure should be a component of the exercise prescription in order to ensure that maximum health benefits are achieved. The physical therapist’s capacity to communicate and educate effectively will determine the long-term outcome of the program.
Chronic disability is often associated with clinical depression, so management of depression alone may improve functional capacity. With respect to pulmonary disease, 45% to 63% of deaths are attributable to advanced lung disease itself.227 Other factors that explain mortality include nutritional deficits, impaired exercise tolerance, functional performance, and social factors, including marital status. Thus nutrition and exercise are essential elements of cardiovascular and pulmonary rehabilitation. Similar findings have been reported for cardiac disease. A negative emotional state is associated with high long-term mortality. Addressing the individual’s psychological status may improve functional status.228
Specific rehabilitation goals include the following:
 To serve as a health promotion resource for the individual, community, and health care providers
To serve as a health promotion resource for the individual, community, and health care providers
 To increase aerobic capacity and muscle strength and endurance consistent with overall health and well-being
To increase aerobic capacity and muscle strength and endurance consistent with overall health and well-being
 To improve capacity to perform the activities of daily living and maintain gainful employment
To improve capacity to perform the activities of daily living and maintain gainful employment
 To promote self-efficacy in healthy lifestyle behaviors for long-term health and well-being, as well as for secondary prevention
To promote self-efficacy in healthy lifestyle behaviors for long-term health and well-being, as well as for secondary prevention
 To shift an individual to a lower risk classification
To shift an individual to a lower risk classification
 To reduce risk for revascularization procedures, medical intervention, and physician and hospital visits
To reduce risk for revascularization procedures, medical intervention, and physician and hospital visits
 To promote health and well-being in the patient’s family and community
To promote health and well-being in the patient’s family and community
 To reduce direct and indirect health care costs over the short and long term
To reduce direct and indirect health care costs over the short and long term
Setting and Team Members
In addition to the physical therapist, the team consists of physicians, nurses, a psychologist, a social worker, a pharmacist, and in some centers, an exercise physiologist. Typically, the physical therapist is involved with exercise testing and training, program modification and progression, and eventual discharge. Additional roles involve education and risk-factor modification. A physical therapist applies the principles and practices of cardiovascular and pulmonary rehabilitation to any patient in any setting and to patients who have cardiovascular and pulmonary dysfunction or its risk factors as a primary or secondary diagnosis or concern. The guidelines and standards for assessment and exercise testing and training must be adhered to if the best service and the best and safest outcomes are to be achieved.229
Components of Physical Therapy
Assessment
Central to comprehensive physical therapy management is focusing on the individual rather than on the condition. Although this chapter emphasizes exercise testing and training in individuals with primary cardiovascular and pulmonary conditions, in reality, people present with comorbidities. Thus individuals with secondary cardiovascular and pulmonary dysfunction (see Chapters 25 and 32) are likely to have a high incidence of primary cardiovascular and pulmonary dysfunction or risk for it (in comparison with the general population). For this reason, underlying risk factors and disease must be examined in all patients, irrespective of their primary presenting diagnoses.
Predictors of long-term survival of myocardial infarction include several factors that need to be identified so that patients can be stratified according to risk. These factors include age, left ventricular ejection fraction, diabetes, hypertension, and elevated resting heart rate.230 Attention to these factors may help to detect changes in status early and prevent adverse exercise effects by judicious modification of an exercise program. Individuals who develop late-onset heart failure have a tenfold increased risk for mortality. Glucose abnormalities (hyperglycemia and hyperinsulinemia) in those who do not have diabetes are common in individuals with heart failure (43%).51 Further, these findings are associated with greater functional deterioration than that found in individuals with heart failure without glucose abnormalities. Thus knowledge of an individual’s glucose tolerance is essential at baseline and over time within the rehabilitation program.
Clinical depression is associated with ischemic heart disease in two ways. First, depression is an independent risk factor for cardiovascular disease and related increased morbidity and mortality.231 Second, up to 45% of individuals exhibit symptoms of major depression after acute myocardial infarction. Thus individuals referred to cardiac rehabilitation need to be screened for depression, and psychotherapy, counseling, or pharmacotherapy may be indicated. Remediation of depression associated with chronic disease may augment functional capacity independent of physical rehabilitation. Depression and peak aerobic capacity have been reported to be the best independent predictors of patient-reported physical function scores in older individuals with heart disease.232 These findings suggest a role for depression management that is independent of exercise training but augments functional capacity.
The general assessment must also include an assessment of the individual’s learning style (see Chapter 1 and 28). Prochaska’s Transtheoretical Model of readiness to change has important implications for rehabilitation programs that are formalized (e.g., cardiac and pulmonary rehabilitation), as well as for individual rehabilitation programs. In addition to the goal of shifting an individual into a lower risk category, another objective is to shift an individual into a higher readiness-to-change category. An individual’s readiness to change health-related behavior is assessed, along with his or her intention to engage in the recommended risk-reduction behaviors, including dietary changes, physical activity and exercise, smoking cessation, and relaxation. Readiness to change may differ for each behavior. Barriers include time management, psychological adaptation, and laziness.233 Another component of the education is the assessment of the individual’s knowledge deficits regarding his or her condition.
Education
Education is the central component of cardiovascular and pulmonary rehabilitation. The patient is taught the basics of anatomy and the physiology of heart and lung health, basic nutrition, physical activity and exercise, analysis of lab tests, effects of smoking, effects of medications, and so on. In this way, the patient is empowered and, it is hoped, well motivated to be an agent of change in his or her own life. Lifestyle recommendations need to be reinforced regardless of phase of the program. One report estimated that after a coronary event, 50% of smokers resume smoking on discharge from the hospital.234 With respect to modifying dietary habits, participants in rehabilitation programs may not understand the distinction between the benefits of eating a healthy diet versus simply cutting out certain types of foods from their diets, even after standard instruction about the role of healthy eating to their overall health.235 Thus tailoring health education information to the needs of program participants is essential if true behavior change is to be effected over the long term.
Like exercise, education can be tailor-made to suit the learning needs of each person (see Chapter 28). Individualization of the education considers age, literacy, preferred learning style, ethnic and cultural issues, and readiness to change. Smoking cessation is the most important intervention for patients with heart disease and pulmonary disease.236,237
Promoting self-efficacy and perceived control are central to education strategies developed by physical therapists. Follow-up is needed, however, to ensure self-treatment is sustained over time.238 Inadequate self-treatment behavior at follow-up suggests that new teaching and learning strategies should be developed to ensure that the quality of self-treatment is maintained.
Exercise Program
A reduction in respiratory rate in patients with chronic heart failure improves pulmonary gas exchange, reduces dyspnea, and increases exercise performance. Such improvement was reported in one study in which respiratory training in these patients involved 1 month of training to breathe at a rate of 6 breaths per minute.239 Slowing breathing rate may have some application for patients with chronic heart failure who have impaired gas exchange and breathlessness during exercise as well as at rest.
Goals: Long Term
Long-term goals and outcomes are as important as the short-term physical therapy goals and outcomes. Intervention (drugs and surgery) has short-term benefits, as is evidenced by the apparently high number of repeated revascularization procedures performed, compared with the lifestyle behavioral changes inherent in physical therapy management, including education, smoking cessation, optimal nutrition, and exercise. At the point of entry into physical therapy (acute, subacute, or chronic, with cardiovascular dysfunction as a primary or secondary diagnosis), a long-term plan with goals, outcomes, and follow-ups is integral to the management plan overall (Table 24-2).
Table 24-2
Comprehensive Physical Therapy Management and Lifelong Health Plan
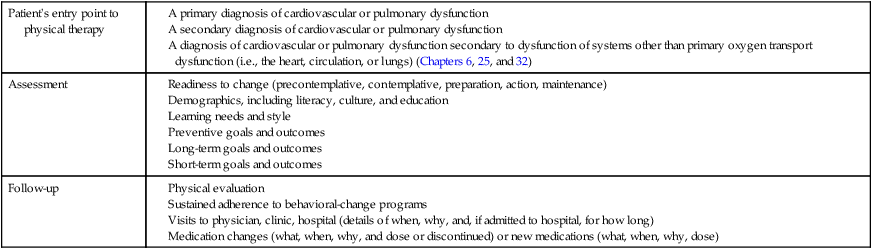
Cardiac Rehabilitation: Specific Components
Phases
Patients are referred to cardiac rehabilitation for management and secondary prevention of myocardial insufficiency and after revascularization procedures, including cardiac surgery.240 People can also benefit if they have significant risk for disease but are asymptomatic.
The phases of cardiac rehabilitation appear in Table 24-3 (with the exception of phase I, inpatient management, which is described in Chapter 29). Phase I refers to inpatient care (medical and surgical) and the predischarge exercise test.
Table 24-3
Rehabilitation Phases of Cardiac and Pulmonary Rehabilitation
| Phase | Cardiac Rehabilitation | Pulmonary Rehabilitation |
| I* | ||
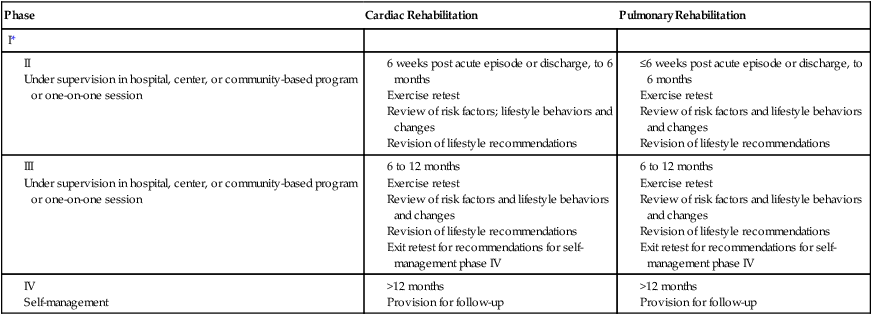
*Phase I is described in Chapter 29, the management of Individuals with Acute Medical Conditions.
Phase II refers to a supervised exercise program lasting 3 to 6 months. Phase II usually takes place in a community center where the patients can be monitored during exercise and education by the rehabilitation professions can be ongoing. However, a trial of home-based phase II programs for high-risk patients after cardiac surgery produced the same results as were found in the control group, which received general guidelines to increase activity levels.241 Further study is needed on the short- and long-term effectiveness of home-based phase II programs as opposed to center-based programs with respect to symptom recurrence, indications for revascularization procedures, and risk-factor reduction.
Nutrition and Weight Control
Optimal nutrition and weight control are priorities. Individuals with cardiovascular dysfunction are at risk for fluid and electrolyte imbalances and related ECG irregularities, so these aspects of nutrition need to be included. In addition, patients with chronic heart failure have some special considerations. These patients rely more on fat substrate during exercise than on carbohydrates, which may contribute to increased catecholamines and free fatty-acid levels.243 These changes may compensate to protect muscle glycogen stores. However, given that fat metabolism is not energy-efficient, this shift may contribute to exercise intolerance.
Risk Reduction
Prevention and rehabilitation programs aim to reduce an individual’s cardiac risk factor category. Figure 24-2 shows an example of a scale for assessing cardiac risk and identifying an individual’s category of risk. Using such a scale provides objective markers for risk factor modification, and evaluating the degree of risk reduction with health behavior change, an important physical therapy outcome. Table 24-4 shows the distinctions among low, intermediate, and high risk for cardiac disease.244
Table 24-4
| Low risk |
Severely depressed left ventricular function (ejection fraction <30%)
Resting complex ventricular dysrhythmias (low-grade IV or V)
Premature ventricular contractions appearing or increasing with exercise
Exertional hypotension (≥15 mm Hg)
Recent myocardial infarction (<6 months) complicated by serious ventricular dysrhythmias
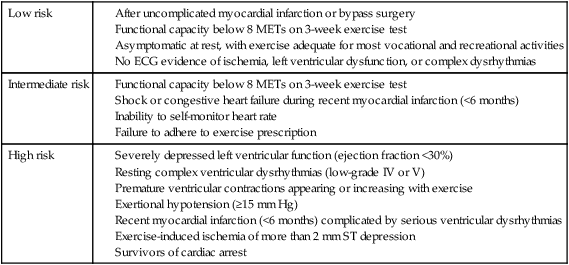
Modified from American College of Sports Medicine: ACSM’s guidelines for exercise testing and prescription, ed 8, Philadelphia, 2010, Lippincott Williams & Wilkins.
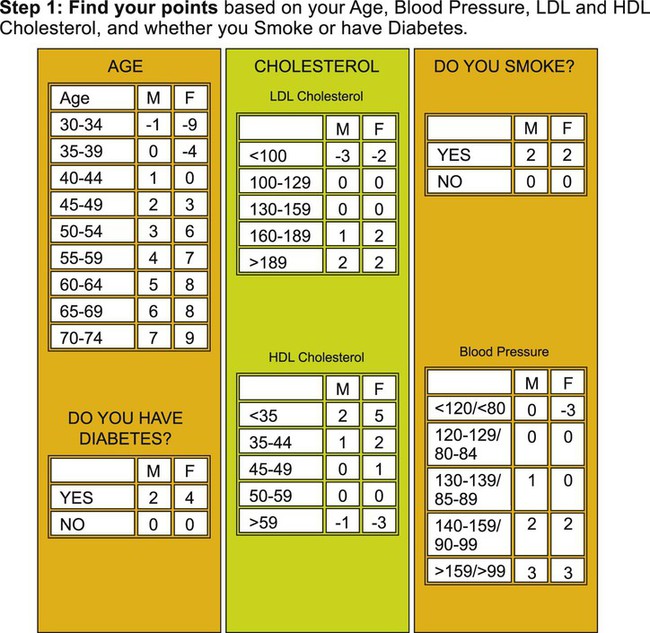
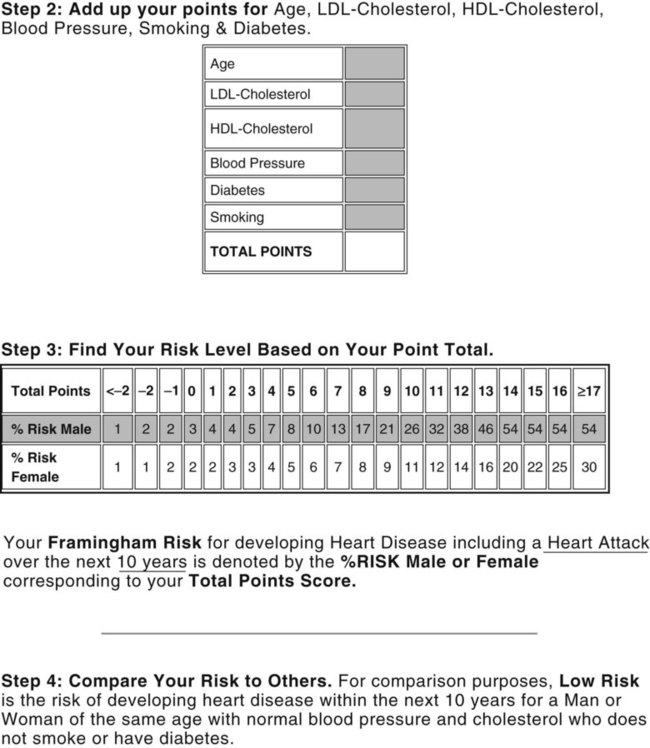
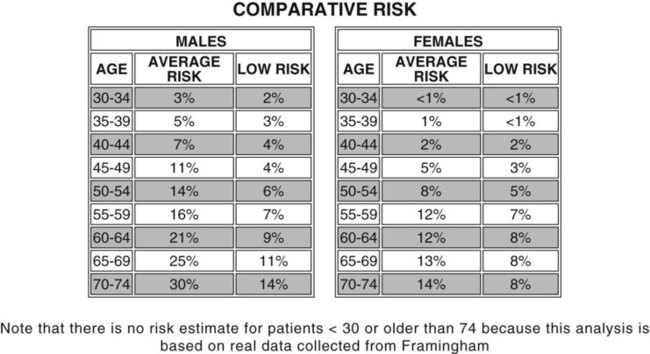
After angioplasty, bypass surgery, and medical therapy for fixed obstructions, individuals remain at risk, as judged by the proportion of patients who require further pharmacological and surgical management. Risk-reduction interventions are priorities in this cohort of individuals; they can extend survival, improve quality of life, reduce the need for further invasive procedures such as angioplasty and bypass surgery, and reduce the incidence of myocardial infarction.245 Secondary risk reduction is as important as primary risk reduction, and it should be a routine component of both medical and surgical management.
Physical Activity and Exercise: Special Considerations
The principles and practice of exercise prescription are described in detail in Chapter 19. However, special considerations for individuals with chronic heart conditions with respect to monitoring, exercise testing, and exercise training are detailed here.
Monitoring
Assessment and monitoring considerations for the individual with heart disease are described in Part Two and Chapter 31. At the onset of the program, a baseline assessment is made of the patient’s subjective sense of well-being, including health-related quality of life, impact of sickness and disability, quality of life, and life satisfaction. Related assessments are made throughout the program to observe the program’s effects on these outcomes and to assess the impact of the program at its completion.
An individual with primary cardiovascular dysfunction or its risk factors requires particular attention to his or her hemodynamic status. Risk factors, however, do not necessarily predict complications during supervised exercise.246 Serial lipid profiles, blood pressure, resting heart rate, and body weight are monitored regularly, and interventions are modified accordingly.247 Blood pressure, however, can be abnormal in individuals with exercise-induced left ventricular systolic dysfunction, which leads to unstable hemodynamic status.248 Blood pressure may not be a valid measure of exercise stress in such individuals. Further study is needed before exercise risk stratification guidelines can be used with any assurance to monitor supervised rehabilitation programs.
The absolute and relative changes in heart rate, blood pressure, rate pressure product, arterial saturation, and perceived exertion are particularly important. ECGs may be performed intermittently throughout exercise or continuously, as indicated. Recent evidence has questioned the conventional guideline of an ST-segment depression of greater than 1 mm in favor of a more conservative guideline, greater than 0.5 mm during or after exercise.249 This value is associated with risk for myocardial infarction, requiring bypass surgery, and risk for cardiac mortality.
Exercise-induced silent myocardial ischemia is an important indicator of increased risk for cardiovascular disease (3.5-fold) and stroke (2.2-fold) in men when they are compared with those without silent ischemia. Other risk factors include smoking, hypercholesterolemia, hypertension, and being overweight.250
Recovery data are important components of the exercise testing assessment and interpretation. Delayed heart rate recovery is a predictor of mortality,184 irrespective of angiographic evidence of disease severity.251 Heart rate recovery is calculated as the difference in heart rate from peak exercise to that recorded at 1, 2, and 3 minutes after exercise. Women have been reported to be more susceptible to postexercise hypotension than men; an active cool-down period may offset postexercise hypotension.252 Signs and symptoms of overexertion must be monitored (Box 24-2).
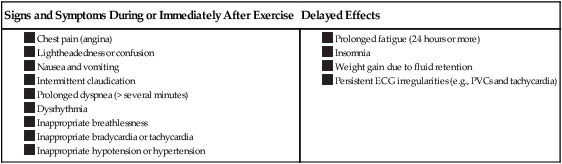
Exercise Testing
Exercise testing is used for diagnosis, assessment of functional work capacity, assessment of the outcome of one or more interventions, including a training program, and prognosis. A poor response to exercise after percutaneous transluminal coronary angioplasty can identify restenosis.253 The graded exercise test, or maximal stress test, is usually a short (8 to 12 minutes, ideally), progressively ramped, symptom-limited exercise test conducted on a treadmill or cycle ergometer. Several established cardiac stress test protocols, such as the Bruce and the Balke, are available. In some situations, a submaximal test is preferred because a maximal test may be risky or difficult to conduct in a valid manner because of a secondary problem. Recently, the prognostic superiority of a two-step exercise test that combines a low-intensity, steady-work-rate phase and a maximal exercise phase has been reported.114 An exercise test may answer questions about an individual’s status and thus obviate or reduce the need for more invasive and costly testing.254
The exercise testing protocol is designed to stress the patient’s oxygen transport system—ventilation, heart, circulation, and muscles—progressively and in an integrated manner. Exercise is the single best way to assess the integrated function of these systems and their capacity for oxygen transport. For detailed evaluation and prognosis of a patient with advanced heart failure, assessment of  is preferable to the use of submaximal exercise tests such as the 6-minute walk test.113 Walking on a treadmill has been reported to have greater diagnostic sensitivity than cycling in asymptomatic men with coronary artery disease.255
is preferable to the use of submaximal exercise tests such as the 6-minute walk test.113 Walking on a treadmill has been reported to have greater diagnostic sensitivity than cycling in asymptomatic men with coronary artery disease.255
Valid testing of functional capacity in individuals with cardiac failure is necessary because of the discordance of the results of various tests in the same individual.256 The 6-minute walk test distance has been reported to be highly reproducible in patients with heart failure.257 Distance walked is somewhat correlated to the New York Heart Association functional classification and quality of life, and this correlation is stronger for individuals with mild and moderate disease severity (New York Heart Association classifications II and III).256 Compared with more sophisticated and more invasive testing, the 6-minute walk test can serve to stratify individuals in terms of functional status, which is of therapeutic and prognostic importance.
Chapter 19 describes indications for conducting an exercise test, as well as the relative and absolute contraindications to the test. That chapter also notes the importance of maximizing test validity and reliability by adhering to strict standards for pretest conditions in the patient, including medications, testing standards, and monitoring recovery data. In addition, the chapter describes basic and advanced measures that can be taken, depending on the needs of the patient and the specific purpose of the test. In most individuals with cardiac dysfunction, an ECG is monitored continuously, along with heart rate. Blood pressure and ratings of perceived exertion and dyspnea (PE) are monitored intermittently. Additional measures are taken as indicated. For example, a patient may be limited by arthritic pain, so it is important to monitor discomfort and pain using a standardized scale (see Chapters 15 and 19). Medications must be reviewed and the time at which they were last taken must be noted in order to determine their impact on responses during the exercise test and to establish which measures will be most valid in terms of assessment of exercise response.
Potential complications that could occur during exercise in patients with heart failure must be anticipated and appropriate monitoring instituted to maximize the safety of exercise testing and training. Adverse responses include dysrhythmias and hypotension.258
Individuals with unexplained dyspnea are at risk for ischemia and cardiac events. Exercise echocardiography provides independently derived information that identifies patients at risk.259 Dyspnea requires investigation in individuals with suspected or known heart disease.
Exercise testing has a role in predicting surgical outcomes.  and exercise duration are good parameters for evaluating functional class and postoperative status in people who have undergone valve repairs or valvuloplasty.116 Patients who have a
and exercise duration are good parameters for evaluating functional class and postoperative status in people who have undergone valve repairs or valvuloplasty.116 Patients who have a  of at least 19 mL/kg/min preoperatively achieve a higher functional class 1 year after surgery.
of at least 19 mL/kg/min preoperatively achieve a higher functional class 1 year after surgery.
Exercise Training
The parameters of exercise training are based on the assessment and on the short- and long-term objectives of the exercise program, and these differ for each individual. The training session begins with a warm-up defined by a work rate intermediate between the target training zone and rest. Warm-up exercise has a protective effect against left ventricular dysfunction in individuals with angina.260 In a repeat test 30 minutes after the first test, the threshold for angina and ST-segment depression has been reported to increase along with the rate pressure product. No threshold intensity has been identified for aerobic training in individuals with cardiac disease.261 Even though a lower limit of 45% of  reserve is commonly reported in the literature, intensities below this level cannot be ruled out, particularly in extremely deconditioned people. The absence of such a limit supports the need to consider individual differences and to prescribe exercise on an individual basis (Table 24-5).
reserve is commonly reported in the literature, intensities below this level cannot be ruled out, particularly in extremely deconditioned people. The absence of such a limit supports the need to consider individual differences and to prescribe exercise on an individual basis (Table 24-5).
Table 24-5
Guidelines for Exercise Prescription for Individuals with Heart Conditions
| Type | Area of Focus | Intensity | Duration | Frequency |
| Aerobic exercise (walking, ergometry, rowing, running) | Large muscle groups |
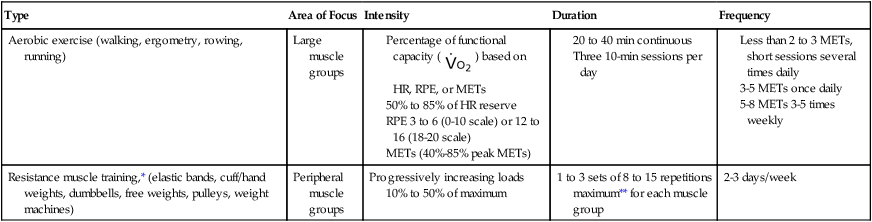
HR, Heart rate; MET, metabolic equivalent; RPE, rating of perceived exertion.
*According to American Association of Cardiovascular Pulmonary Rehabilitation (AACVPR) Guidelines for Pulmonary Rehabilitation Programs (ed 4), “to prevent soreness and minimize the risk of injury, the initial load should allow 12-15 repetitions comfortably. If 1 RM pretest is used, this load would be approximately 30-40% 1 RM for the upper body and 50-60% for hips and legs. Low-risk stratified, well-trained patients may progress to higher loads depending on program goals.”
**Repetition maximum is the maximum number of times a load can be lifted before fatigue.
Modified from American College of Sports Medicine: ACSM’s guidelines for exercise testing and prescription, ed 8, Philadelphia, 2010, Lippincott Williams & Wilkins; and AACVPR: Guidelines for Pulmonary Rehabilitation Programs, ed 4, Champaign, Ill, 2011, Human Kinetics.
Many types of exercise can be considered in the exercise prescription. Improvement in walking tolerance and distance is a primary goal because it is a hallmark of independence and mobility, particularly with advancing age, and it is coupled with the upright position and its associated gravitational stress. Walking has multiple physiological benefits in individuals with coronary artery disease262 as well as in healthy people. Decisions are made based on the specificity principle. If the goal is to improve the patient’s functional needs, activities that are closest to those needs are chosen. If improving aerobic fitness and maximum functional capacity is the goal, exercise that involves more limbs would be the best choice.
The use of hydrotherapy and aquacise have been prominent in Europe. Another application that has been reported to have beneficial effects on the exercise responses of individuals with chronic heart failure is thermal hydrotherapy, which involves the passive application of heat and cold.6 A 6-week program of home-based hydrotherapy was reported to improve resting and submaximal heart rates, in addition to reducing symptoms and improving quality of life. These effects were attributed to physiological adaptations to alternating hot and cold body stimulation. Further study of this application and its mechanisms is necessary; its indications may prove to be positive in individuals challenged by even minimal amounts of exercise.
Conventionally, the exercise intensity for patients with heart disease is set at a proportion of oxygen uptake reserve or heart rate reserve, which suggests a critical threshold for training effects. However, no intensity threshold for aerobic training has been identified, so intensities below the accepted standard probably provide training stimulus, particularly for patients with low functional capacity.261
It has been suggested that interval training leads to more marked improvement in hemodynamics in individuals with heart failure than does steady-rate work.263 Another suggestion is that steady-rate aerobic exercise contributes to greater well-being and quality of life. Further study is needed to examine the effects of various parameters in training protocols in this cohort.
Peak functional capacity depends on muscle strength and endurance in individuals with chronic heart failure.264 Improvement in subjective symptoms reported in daily activities, especially dyspnea on exertion, however, depends largely on muscle endurance.
Resistance muscle training has an important role in cardiac rehabilitation programs; it allows a patient to regain lost strength, and it facilitates avocational activities and return to work soon after a cardiac event.265 Resistance muscle training in the form of circuit weight training can be integrated into the cardiac rehabilitation program. Muscle training can be safe and therapeutic even at relatively high workloads in properly selected individuals, including older adults.266 The hemodynamic response depends on the isometric and postural stabilization component, in addition to the load or resistance used, the muscle mass activated, the number of repetitions in the set, and the duration of each contraction, as well as the involvement of the Valsalva maneuver. Upper-body work has been viewed conservatively as an exercise option for individuals with cardiac problems, and it warrants greater emphasis.267 Despite caveats regarding isometric exercise for individuals with coronary artery disease, one study compared the hemodynamic responses of brief and sustained isometric exercise and dynamic exercise in individuals with heart disease and healthy people.268 The incidence of myocardial ischemia was reported to be lower during isometric exercise than during dynamic exercise in patients at the same level of perceived exertion. The investigators postulated that isometric exercise generates high perfusion pressure in the coronary arteries and prolongs perfusion, thereby potentially protecting the myocardia from ischemia. Further study is needed to examine this hypothesis.
Lengthening (eccentric) muscle contractions and shortening (concentric) muscle contractions have distinct energetic and metabolic properties that may make one or the other better suited for certain patient populations.269–271 Eccentric muscle contractions are associated with higher muscle tension and less metabolic demand. For low-risk individuals who have ischemic heart disease without angina, inducible ischemia, or left ventricular dysfunction, eccentric exercise can be recommended; these patients can perform high-load resistance exercise with minimal cardiovascular stress.272
Electrical stimulation of the quadriceps has been examined as a form of exercise for individuals with chronic heart failure.273 Although the improvement in muscle performance and exercise capacity was comparable to that of individuals in an ergometer exercise program, the use of electrical stimulation should be considered in the overall context of the individual’s needs. Active exercise has many multisystem benefits that electrical stimulation does not provide. In addition, electrical stimulation is a more passive modality than active exercise, which may be counter to the goal of self-efficacy that cardiac rehabilitation promotes.
Hydrotherapy in a home-based program has shown some interesting applications to individuals with chronic heart failure.6 In a study of individuals with mild heart failure, an intensive 6-week program of home-based repeated brief cold stimuli appeared to improve peripheral circulation and, in turn, to improve heart-failure symptoms, heart rate response to exercise, and quality of life.
Pulmonary Rehabilitation: Specific Components
Phases
The phases of pulmonary rehabilitation can generally be considered comparable to those of cardiac rehabilitation, although they are less well defined in terms of a formal inpatient phase after an acute episode followed by progressively less closely supervised phases (see Table 24-3). A patient with chronic lung disease is more likely to be referred when stable than in conjunction with an acute event. The first graded exercise test may be in the supervised program rather than in the hospital before discharge after an admission for acute symptoms.
Nutrition and Weight Control
The connection between nutrition and lung health has become a focus of research interest, and that research supports the role of good nutrition (in particular, the consumption of fruits, vegetables, and fish) in optimal lung health.274,275 Diet may be an important cofactor in the development of COPD. Whether good nutrition improves damaged lungs has not been substantiated, but good nutrition improves general health and thus should be a primary recommendation when managing these patients.
Risk Reduction
Lifestyle modification and risk factor modification are fundamental components of the pulmonary rehabilitation program; these modifications include smoking cessation, nutrition and weight control, and stress management, in conjunction with physical activity and exercise. Optimal nutrition is encouraged as a lifelong change in patients with COPD, whose nutritional status is often suboptimal.276 Carbohydrate-rich foods, known to increase carbon dioxide production, have been targeted as a food group that should be limited in patients with COPD. Small changes in the carbohydrate constituents of diet have been reported to have a major effect on  , exercise tolerance, and breathlessness.277 Smoking cessation is essential to limit further lung damage and has the potential to reverse impaired pulmonary function, improve oxygen transport capacity, and reduce or reverse smoking-related risk factors as the period of nonsmoking lengthens. Reduction of pulmonary and cardiac risk factors in an individual with primary lung dysfunction is essential.
, exercise tolerance, and breathlessness.277 Smoking cessation is essential to limit further lung damage and has the potential to reverse impaired pulmonary function, improve oxygen transport capacity, and reduce or reverse smoking-related risk factors as the period of nonsmoking lengthens. Reduction of pulmonary and cardiac risk factors in an individual with primary lung dysfunction is essential.
Physical Activity and Exercise: Special Considerations
The principles and practice of exercise prescription are described in detail in Chapter 19. However, special considerations for this patient group, with respect to monitoring, testing, and training, are detailed here.
Exercise Testing
The indications for and contraindications to testing are established (see Chapter 19). The goals of an exercise test are determined beforehand for each given individual. The exercise test may be selected to evaluate aerobic capacity or the strength and endurance of peripheral or respiratory muscles. The demands of upper-body work may compete with breathing demands in some patients, so upper-body work is integrated into the overall program judiciously and monitored accordingly. Upper-body strength tends to be lower than lower-body strength in patients with chronic obstructive lung conditions. Upper-body strengthening can reduce rating of perceived exertion and breathlessness and thus warrants being assessed and trained.278
The exercise test to assess cardiovascular and pulmonary conditioning may be maximal or submaximal and may involve a modality such as a treadmill or ergometer, depending on the device’s suitability for the patient and on the best means of maximizing the test’s validity and reliability. Depending on the purpose of the test, a decision is made beforehand about the patient’s medications and when they are taken in relation to the timing of the test. Some patients may be tested with oxygen or purposely without oxygen, or with or without bronchodilators, depending on whether the effect of such interventions is being evaluated. It is essential to monitor dyspnea in these patients and to correlate the dyspnea rating with objective measures. Some patients may have invasive blood work done before, during, and after the test to monitor serial arterial blood gases. Pulse oximetry is routinely monitored along with heart rate and blood pressure. Some patients may require ECG monitoring. Invasive procedures such as arterial blood gas measurement are done as indicated. Respiratory muscle testing and training are based on similar principles. (Detailed descriptions appear in Chapter 26.)
Exercise testing can be used to diagnose exercise-limiting factors. For example, exercise testing in a patient with pulmonary fibrosis can distinguish cardiovascular and pulmonary limitations. Exercise-induced hypoxemia in this cohort has been closely related to survival.279
Choice of exercise testing and training modalities is determined by the indications for the test and for training. Patients with COPD show different responses to walking and to cycling.280 Aerobic capacity in walking is less than in cycling and is associated with excessive ventilatory demand during peak exercise supported by increased ventilatory dead space, reduced ventilatory efficiency, and arterial hypoxemia. Arm ergometry is associated with greater dyssynchronous breathing than is leg work, so it may be an inappropriate modality for patients with severe disease.281
Low-flow oxygen is a common intervention for hypoxemia in patients with severe COPD. Although long-term oxygen therapy improves survival,282,283 there remain many unanswered questions regarding the use of the modality and its efficacy during exercise training.284 Further study is needed to establish its efficacy in improving exercise capacity in patients with hypoxemia, as well as without hypoxemia, and to establish the characteristics of responders versus nonresponders, which will allow for the refinement of exercise prescription in this patient cohort. A study of patients with cystic fibrosis showed that supplemental oxygen speeded recovery after a short bout of maximal exercise and preserved subsequent exercise performance.285
In individuals with COPD and mild exercise hypoxemia, relief of breathlessness with supplemental oxygen has been explained by a commensurate reduction in ventilatory demand and reduced blood lactate levels.286 Short-term use of oxygen before or after exercise has not been supported.287
Exercise Training
Training involves flexibility and strengthening, as well as aerobic exercise. Although patients learn to self-monitor and pace their exercise based on their responses, many have had long-term physical therapy and instruction in breathing control because of continued altered breathing pattern, even during ADL.288,289 Walking in conjunction with breathing control is particularly useful for patients with pulmonary dysfunction. Pulse oximetry may have to be used to guide the training session.
Lengthening (eccentric) muscle contractions are associated with reduced energy cost, so such exercise has important therapeutic implications for individuals with poor aerobic capacity.270 However, eccentric muscle work in the form of downhill walking or cycling on a negative-work ergometer alters breathing patterns toward a tendency to breathe rapidly and shallowly.269,271 Thus patients require stringent monitoring when performing this type of energy-efficient exercise.
Cardiac and Pulmonary Rehabilitation: Future Directions
Based on epidemiological indicators, behavioral strategies have the greatest potential for long-term improvement in the abilities and participation of individuals with lung conditions (see Chapters 1 and 5). When effectively administered and adhered to, these interventions are not associated with the risks of invasive management, which must be minimized as much as possible commensurate with the individual’s functional improvements. On the contrary, these noninvasive interventions help to ensure reduced long-term morbidity and increased health overall, thus reducing health care needs and potentially increasing individual longevity.
Finally, research is needed to establish how best to structure the principles of cardiac and pulmonary rehabilitation on an individual basis to maximize sustainable benefits for life. Some have argued for inclusion and exclusion criteria to maximize the success of the program.290 Identifying and reducing barriers to access and participation and maximizing adherence through motivational interviewing and cognitive therapeutic interventions may maximize the impact of these services on society.
Summary
Based on state-of-the-art literature, this chapter extends the general exercise testing and training principles described in Chapter 19 to specific considerations in relation to the principles of best physical therapy practice in cardiac and pulmonary rehabilitation programs, regardless of whether delivered in a structured group format or in one-on-one sessions. Structured formal programs are often available only in large urban areas and thus have low access rates. The same principles, however, are fundamental to physical therapy practice overall and can be readily applied in a one-on-one setting in private practice or in a health care facility. These principles should be applied not only to patients with primary heart and lung conditions but also in the physical therapy management of patients being treated for musculoskeletal and neuromuscular conditions who have secondary diagnoses of chronic heart and lung conditions or who have associated risk factors. In these cases, the physical therapy program must be adapted to the requirements of these underlying conditions (or these conditions may need to be managed independently if they have not been previously identified as a priority). In this way, the patient’s more serious underlying cardiovascular and pulmonary problem is addressed and the interventions, including exercise prescribed for the musculoskeletal or neuromuscular problems, are modified according to the more serious life-threatening condition. Exercise testing and training are only part of the management of individuals with chronic, primary cardiovascular and pulmonary dysfunction; the comprehensive approach to management is described in Chapter 31.
The principles of exercise testing and training in individuals with cardiovascular and pulmonary dysfunction secondary to conditions other than primary cardiovascular and pulmonary dysfunction are described in the following chapter, Chapter 25.



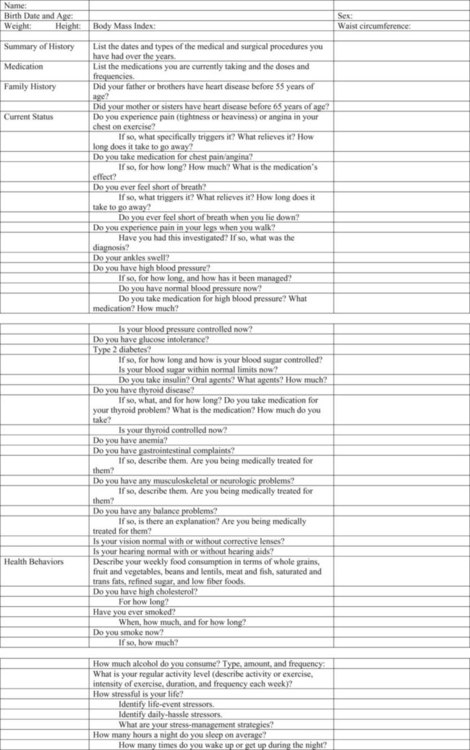













 ) based on HR, RPE, or METs
) based on HR, RPE, or METs can be examined, along with their physiological and clinical correlates. The ventilatory efficiency can be determined on the basis of the ventilatory equivalent of CO2 (minute ventilation [
can be examined, along with their physiological and clinical correlates. The ventilatory efficiency can be determined on the basis of the ventilatory equivalent of CO2 (minute ventilation [ ] divided by CO2 production [
] divided by CO2 production [ ]). The limitation of oxygen consumption studies is the difficulty of ensuring a valid and reliable test. The test requires that a face mask or mouthpiece be worn, either of which can distort the patient’s breathing. The patient may feel anxious when wearing such devices or may alter his or her breathing pattern because of the increased dead space in the expiratory hose.
]). The limitation of oxygen consumption studies is the difficulty of ensuring a valid and reliable test. The test requires that a face mask or mouthpiece be worn, either of which can distort the patient’s breathing. The patient may feel anxious when wearing such devices or may alter his or her breathing pattern because of the increased dead space in the expiratory hose.


