CHAPTER 21 EXAMINATION OF THE VISUAL SYSTEM
VISUAL ACUITY
| Red-green males | 8% |
| Red-green females | 0.4% |
| Blue-yellow | 0.005% |
| Achromacy | 0.003% |
VISUAL FIELD EXAMINATION
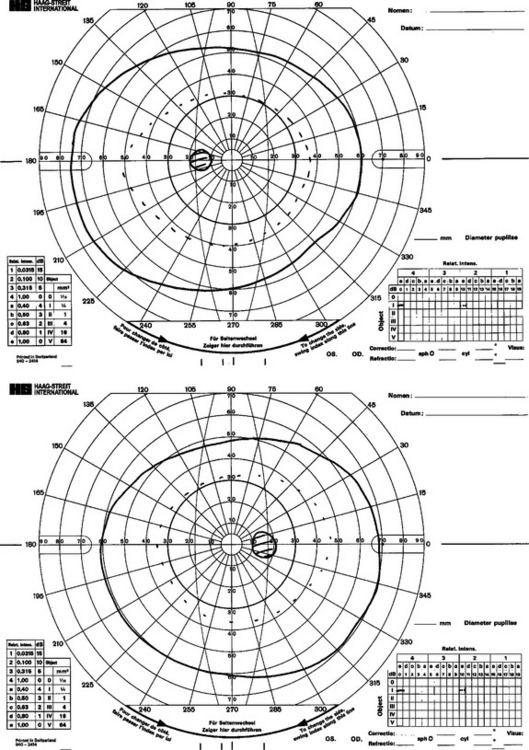
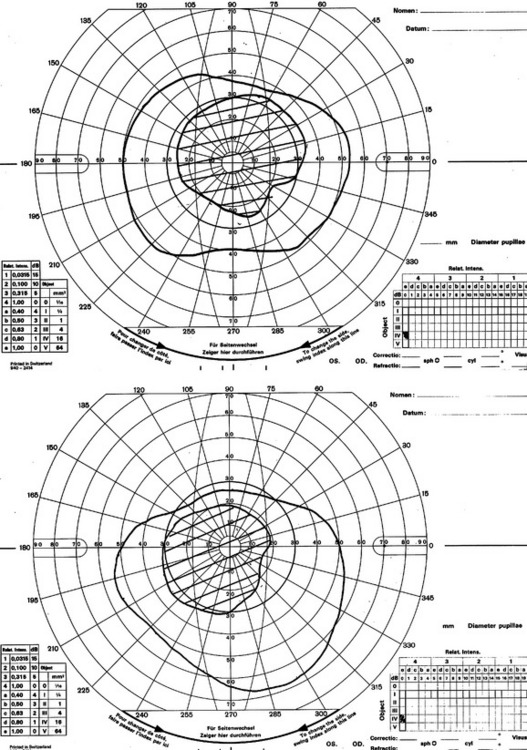
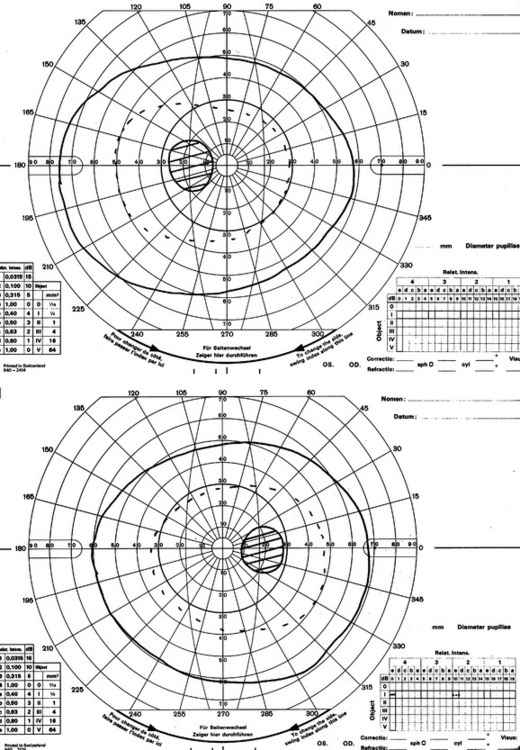
The principle behind dynamic perimetric methods of field analysis such as the Goldman is that the examiner is identifying successive boundaries of vision known as differential light sensitivities (DLSs). These are the thresholds within which it is possible for that part of the retina to identify when a light projected is more bright than the background. The fovea is most sensitive, and this reduces with distance from the fovea. The temporal field changes slowly with distance from the fovea, whereas the DLS on the nasal side reduces abruptly. A normal Goldman field is shown in Figure 21-1. The advantage of this method of field assessment is that the skilled examiner can plot very carefully visual field abnormalities and can return over and over again to check the boundaries of the field.
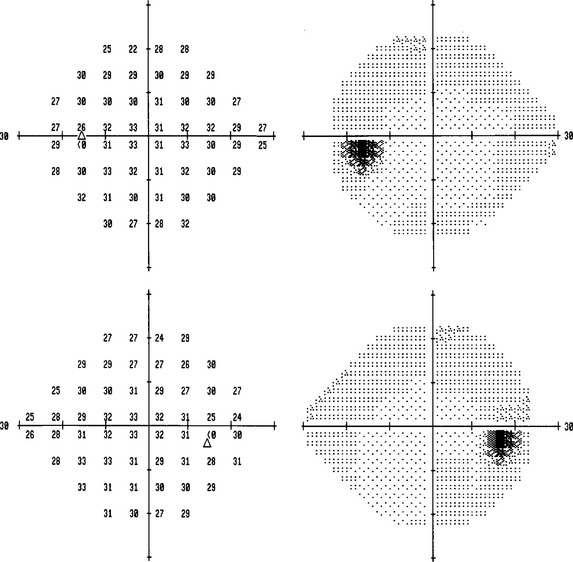
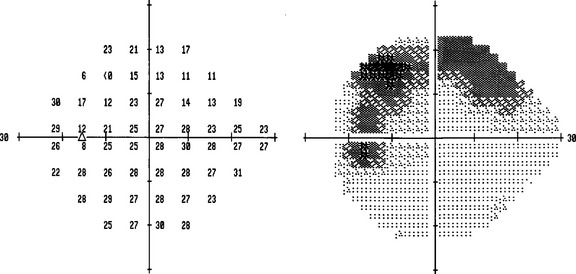
Automated static perimetry is available in all ophthalmic departments, can be carried out in around 10 minutes, is easy to administer, and does not require so much skill to perform. It is less sensitive a measure than the Goldman when the examiner is highly skilled in use of the latter. Automated static field tests identify the threshold of accurate vision within the four visual quadrants within a 10, 24-, 30-, or 70-degree field. Fields can be recorded for comparison with subsequent examinations; reliability can be assessed by noting fixation losses and false-positive and -negative errors. The gray scale indices note the mean or pattern deviation of the patient’s responses to those of age-matched normal controls (Fig. 21-2).
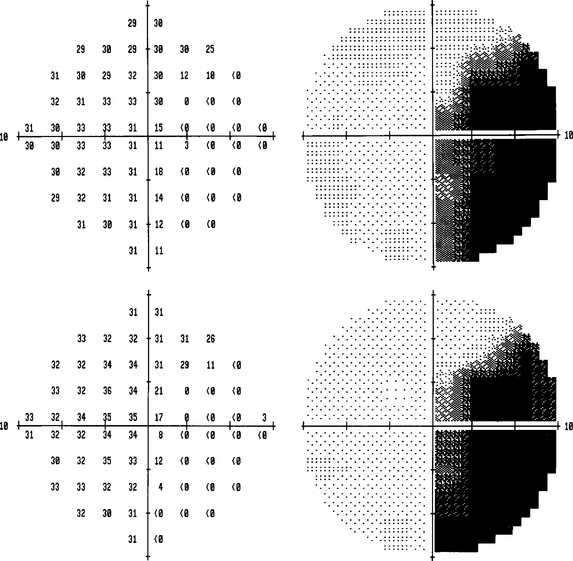
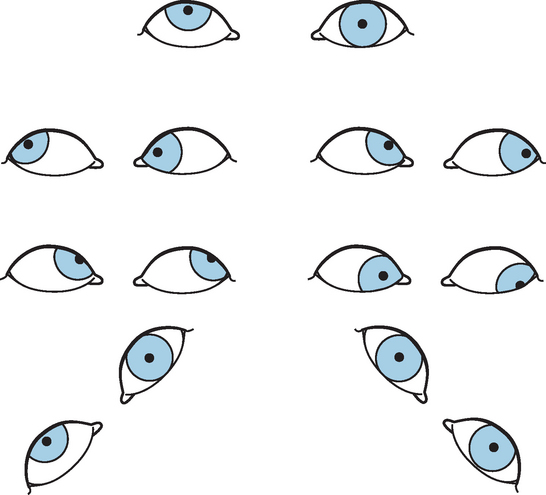
Factors that influence the precision of these field examinations include cognitive function and tiredness, refractive errors, and ophthalmic disorders such as cataract. The field is plotted at a certain level of background illumination because the threshold varies with background luminance up to a certain point and then increases in a linear way with suprathreshold background luminance. Examples of common field defects that are seen are shown in Figures 21-3 to 21-8.
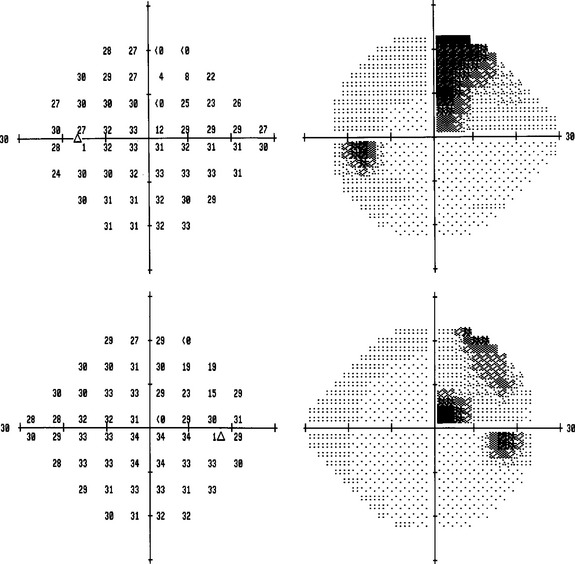
Figure 21-3 Upper quadrantinopia due to a left temporal infarction, left, upper field; right, lower field.
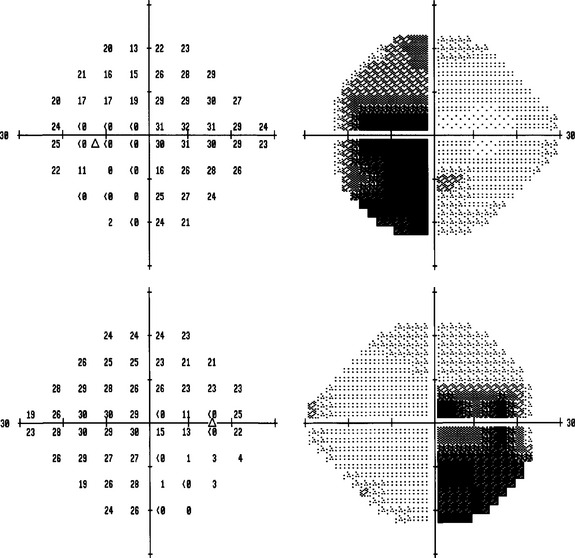
Figure 21-5 Bitemporal hemianopia due to a craniopharyngioma, left, upper field; right, lower field.
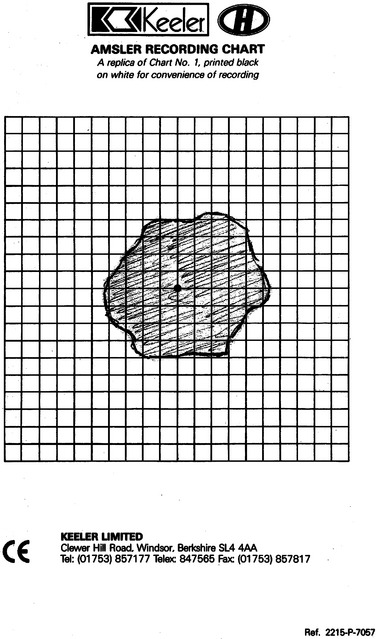
The Amsler grid is useful for plotting central field distortions, such as macular disorders, but also very small central field abnormalities due to, for example, optic neuropathy. The patient plots out the abnormality on the grid himself (Fig. 21-9).
PUPILS
Relative Afferent Pupillary Defect
Everyone knows about this test and medical students believe that they should also perform it, but it is very complicated and requires skill and experience in order to perform it well. The eyes may be covered and uncovered in turn or the swinging light test may be applied. In the latter, the light source is applied in turn to each eye for 3 to 5 seconds repeatedly. The trick is to vary the time taken to move from one eye to the other; often, the relative afferent pupillary defect (RAPD) can be brought out thus. Great care should be taken to not apply the light source to one eye for longer than the other, to apply the light source to the same amount of retina in each eye (this is particularly important if there is ocular misalignment), and to ensure that there is no accommodative meiosis. Provided the test is performed properly, the examiner is able to see that there is pupillary dilatation on the side of a unilateral optic neuropathy when the light source returns to that side. Neutral density filters can be used, first, to measure the severity of the RAPD and, second, to bring it out if by regular testing the result is equivocal. The grading of RAPD is as follows:
| Grade 1: weak initial contraction followed by a greater redilatation | 0.4 log unit |
| Grade 2: a slight stall in movement followed by dilatation | 0.7 log unit |
| Grade 3: immediate pupillary dilatation | 1.1 log units |
| Grade 4: pupillary dilatation during prolonged illumination of the good eye for 6 seconds | 2.0 log units |
| Grade 5: no signs of constriction | no light transmission |
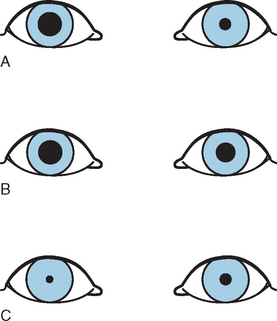
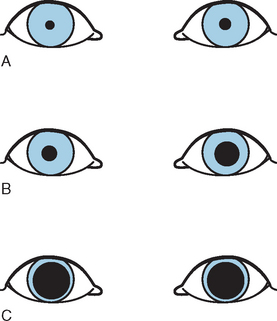
Pharmacological Testing
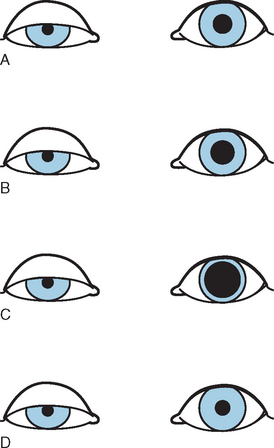
Horner’s syndrome consists of meiosis and ipsilateral partial ptosis, apparent enophthalmos, and absence of sweating of the face ipsilaterally. The anisocoria is more evident in dark than in the light. The direct responses are normal. There is a failure of the affected pupil to dilate with 10% cocaine solution. Hydroxyamphetamine 1% dilates the affected pupil if the lesion is central or preganglionic, and no response occurs if the lesion is postganglionic (Fig. 21-10).
Holmes-Adie syndrome consists of subacute severe mydriasis, which partially resolves over many months. It is associated with absent reflexes and rarely autonomic failure (Ross syndrome). The anisocoria is more marked in light than in dark. Pupils are tonic; denervation is rarely complete so vermiform movements (movements of the parts of the iris that have not been denervated) can be seen on slit lamp examination. Pilocarpine 0.1% constricts the affected pupil more than the normal owing to denervation supersensitivity (Fig. 21-11). Tonic pupils also occur following damage due to trauma and more commonly to inflammation due to viral infections and uveitis.
Finally, a pharmacologically mediated mydriasis will fail to constrict with 1% pilocarpine.
In essential anisocoria, the pupils are usually the same size in light and dark; this may be more apparent in dark but not to the same degree as with Horner’s syndrome. There are normal responses to cocaine (Fig. 21-12).
EYELIDS
OCULOMOTOR SYSTEM
Smooth Pursuit
The patient is asked to fix on a target such as a pen top or hat pin while it is moved slowly and at steady speed from side to side. Those with abnormalities of smooth pursuit show corrective “catch up” saccades and the pursuit becomes fragmented. An optokinetic drum also shows up abnormalities on one side (there will be fewer corrective saccades on that side). In patients with nystagmus, pursuit can be tested by testing for suppression of the vestibulo-ocular reflex; the patient is asked to fixate on the thumb with the arm outstretched while he rotates the head. With abnormalities, there are corrective saccades because the eyes will be taken off track by the slow phase of the vestibulo-ocular reflex.
EXAMINATION OF DIPLOPIA
Alternate Cover Test
The extent of the tropia can be measured in diopters using a prism to correct the diplopia.
Bielschowsky’s Head-Tilt Test
This test is undertaken in four stages:
In the first stage, the patient is examined with the alternate cover test in the primary position of gaze and this reveals a right-over-left hyperphoria; either the depressors of the right (superior oblique and inferior rectus) or the elevators of the left (inferior oblique and superior rectus) are weak (Fig. 21-13). The second stage, in which the patient is examined again with the alternate cover test but in the left and then right gaze, the right-over-left deviation increases on the left gaze. Hence, the oblique muscles, which exert a greater influence on vertical eye movements in adduction, and the recti, which exert a greater influence in abduction, can be differentiated. In this case, the right hyperphoria increases in left gaze, so either the right superior oblique or the left superior rectus must be weak.
Digre KB. Principles and techniques of examination of the pupils, accommodation and the lacrimal system. In: Miller NR, Newman NJ, editors. Walsh and Hoyt’s Clinical Neuro-ophthalmology. 5th ed. Baltimore: Williams and Wilkins; 1998:933-961.
Johnson CA, Keltner JL. Principles and techniques of examination of the visual sensory system. In: Miller NR, Newman NJ, editors. Walsh and Hoyt’s Clinical Neuro-ophthalmology. 5th ed. Baltimore: Williams and Wilkins; 1998:153-237.
Leigh RJ, Zee DS. The Neurology of Eye Movements, 2nd ed. Philadelphia: FA Davis, 1991.