CHAPTER 30 EVALUATING ABNORMAL LIVER TESTS
INTRODUCTION
Thrombocytopenia in the context of liver disease suggests hepatic fibrosis and impaired liver function with concomitant portal hypertension.
APPROACH TO THE PATIENT WITH ABNORMAL LFTs
A detailed drug history is important including:
Liver injury may manifest several weeks after drug cessation.
Risk factors for viral hepatitis must be elicited such as injecting drug use.
INTERPRETING PATTERNS OF LIVER TEST ABNORMALITIES
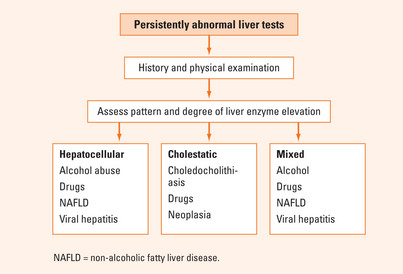
The degree and pattern of liver tests’ elevation may provide clues as to aetiology (Figure 30.1). A practically useful classification is provided below.
Liver test abnormalities are designated as:
In the vast majority of patients with liver disease, the serum ALT exceeds the AST. Exceptions include those with alcoholic liver disease and those with cirrhosis from any aetiology.
Disorders associated principally with elevations in aminotransferase levels
Common causes of liver enzyme abnormalities according to the pattern of enzyme elevation are presented in Table 30.1.
| Hepatocellular | Cholestatic |
|---|---|
| • Excessive alcohol consumption | • Drug-induced liver injury |
| • Drug-induced liver disease | • Choledocholithiasis |
| – Chronic hepatitis B and C | • Primary biliary cirrhosis |
| – Non-alcoholic fatty liver disease | • Primary sclerosing cholangitis |
| – Haemochromatosis | • Pancreatic carcinoma |
| • Autoimmune hepatitis | • Neoplastic infiltration |
| • Wilson’s disease | • Sarcoidosis |
| • Alpha1-antitrypsin deficiency |
Additional laboratory tests useful in identifying specific disorders are listed in Table 30.2.
TABLE 30.2 Laboratory tests to clarify the cause of liver test abnormalities
| Laboratory test | Diagnosis |
| • Hepatitis C antibody | • Positive test suggests chronic hepatitis C infection |
| • Hepatitis B surface antigen | • Positive test suggests chronic hepatitis B infection |
| • Hepatitis B e antigen | • Positive test suggests active viral replication |
| • Serum ferritin, transferrin saturation | • Iron overload suggests haemochromatosis |
| • Antimitochondrial antibodies | • Detected in primary biliary cirrhosis |
| • Antinuclear antibodies, anti-smooth muscle antibodies | • Detected in autoimmune hepatitis |
| • Serum caeruloplasmin | • Reduced in Wilson’s disease |
| • Serum alpha1-antitrypsin | • Decreased in alpha1-antitrypsin deficiency |
Causes of elevated aminotransferase levels
Alcohol-related liver disease (ALD)
Drug-induced liver disease
TABLE 30.3 Commonly prescribed medications causing abnormal liver tests
| Class of medication | Examples |
| • Antibiotics | • Flucloxacillin, minocycline |
| • Antiepileptics | • Carbamazepine, phenytoin |
| • Antipsychotics | • Chlorpromazine |
| • Antituberculotics | • Isoniazid, rifampicin |
| • Lipid-lowering medications | • HMG-CoA reductase inhibitors (statins) |
| • Non-steroidal antiinflammatory drugs | • Ketoprofen, naproxen |
| • Oestrogens | • Oral contraceptive pill |
Chronic viral hepatitis
Chronic hepatitis C
Chronic hepatitis B
Results when immune elimination does not occur following acute infection and the hepatitis B virus (HBV) continues to replicate (see Chapter 36).
Non-alcoholic fatty liver disease (NAFLD)
Haemochromatosis
Autoimmune hepatitis
Wilson’s disease
Other liver test abnormalities
Alkaline phosphatase levels
Gamma-glutamyltransferase levels
Hyperbilirubinaemia
Assessment of a patient with ‘cholestatic’ liver tests
SUMMARY
Liver enzyme abnormalities may be physiological or pathological. Persistent elevation of liver tests must be investigated. Eliciting a detailed history and performing a thorough physical examination is mandatory (Figure 30.1).
Dunn W, Angulo P, Sanderson S, et al. Utility of a new model to diagnose an alcohol basis for steatohepatitis. Gastroenterology. 2006;131:1057-1063.
Keegan A. Abnormal liver function test results. In: Talley NJ, Martin CJ, editors. Clinical gastroenterology: a practical problem-based approach. 2nd edn. Sydney: Elsevier; 2006:373-423.
Sherlock S, Dooley J. Diseases of the liver and biliary system, 11th edn. Oxford: Blackwell Science; 2002.