The significance of morphological changes 9
2.2 Theoretical aspects of manipulation therapy
10
2.3 The significance of functional disturbances
12
2.4 Motion segment and joint dysfunctions
13
2.4.2 Joint play and restriction
14
2.4.3 Reflex changes in joint restriction
15
2.4.4 Is restriction an articular phenomenon?
16
2.4.5 The possible mechanism of restriction and manipulation
16
2.4.6 The effect of manipulation
17
2.4.7 The pathogenesis of restriction
17
2.5 The spinal column as a functional unit
19
2.5.1 The spinal column and balance
20
2.5.2 Key regions of the spinal column in dysfunctions
20
2.5.3 The importance of nervous control
21
2.6 Dysfunctions of the spinal column in childhood
24
2.7 Restrictions and their sequelae
26
2.8 The significance of disturbed motor patterns (stereotypes)
27
2.9 Sequelae of disturbed movement patterns
29
2.9.1 Walking and standing
29
2.9.2 Straightening up from a forward-flexed position
29
2.9.3 Raising the arms
30
2.9.5 The effect of respiration on the locomotor system
30
2.10 The significance of constitutional hypermobility
33
2.11 Reflex processes in vertebrogenic dysfunctions
34
2.13 The term ‘vertebrogenic’
37
2.1. The significance of morphological changes
Chapter 1 indicated the great range of application of manipulative therapy and most methods of reflex therapy, which can be used for many different cases of pain in the locomotor system; these often involve pain whose cause and therefore treatment remain controversial. For a long time they were generally considered to be of inflammatory origin, for the simple reason that this provided the easiest explanation for the pain. Indeed we still speak of rheumatic diseases, for example ‘soft tissue rheumatism,’ and many terms ending in ‘-itis’ bear witness to this attitude (spondylitis, arthritis, radiculitis, neuritis, fibrositis, myositis, and panniculitis, for example). Since, however, inflammation is a well-defined pathological condition which
can be demonstrated or disproved, the inflammation theory became untenable and had to be abandoned for lack of evidence.
Pathological anatomy and the use of radiology to examine pathology in living patients (X-rays) played their part by demonstrating degenerative changes. In place of terms ending in ‘-itis’ we speak of spondylosis, arthroses, and ‘diskopathy.’ This approach offers the possibility of explaining the changes in tissues that are sometimes bradytrophic. Vascularization of the intervertebral disk becomes reduced at quite a young age and the nucleus pulposus dries out: the water content decreases from 90% in the first decade of life to 70% in the third decade. According to Schmorl, 60% of women and 80% of men at age 50 show evidence of degenerative changes of the spinal column, while by the age of 70 the figure is 95% for both sexes.
The very abundance of degenerative changes makes it difficult to define their pathogenetic significance. Whereas the number of degenerative changes increases with age, back pain occurs most often between the fourth and sixth decade, to become less common in old age. Subjects with considerable degenerative changes may be completely without clinical symptoms; alternatively they may suffer an attack of acute pain which subsides after a time (while the degenerative changes remain the same) to leave them once more symptom free. There can even be severe pain in young patients with no degenerative changes at all.
The main difficulty is the fact that the term ‘degenerative’ is so poorly defined. It is used on the one hand for destructive lesions typically only found in the hip and knee, and on the other hand for changes of little clinical significance, and which are better described as normal ‘wear and tear.’ Often the change is a compensatory process or adaptation – as in scolioses, in hypermobility, or even instability (for example in spondylolisthesis) which can thus be stabilized. It is often difficult to distinguish between changes resulting from trauma and degenerative ones. When we find degenerative changes, we should begin by asking about their clinical relevance. It is a mistake to draw clinical conclusions without good reason from the mere existence of non-destructive degenerative changes seen on X-ray; they do not in themselves justify speaking of ‘degenerative disease.’
There is certainly some correlation between degenerative changes and herniated disk; with a few exceptions, herniation occurs mainly in disks already showing some degenerative change. The discovery that disk herniation can be a cause of pain was an important step historically, but the success of surgical treatment was often so striking that disk lesions came to be held responsible for most of the many instances of pain related to the spinal column. The principles that applied to radicular syndromes, mainly in the lumbosacral region, were uncritically applied to a whole range of complaints in all parts of the spinal column. ‘Diskopathy’ became the fashionable word for what we now refer to as vertebrogenic (or spondylogenic) disease.
Everyday practice contradicts this view and serves to correct it. Although disk surgery is a routine procedure for radicular syndromes of the lower limbs, it is rarely performed for low-back pain or radicular syndromes of the upper limbs, and not at all for simple neck pain or vertebrogenic headache. Nor is disk herniation the only possible cause of pain in radicular syndromes of the lower limbs: in operation statistics no disk herniation is found in about 10% of the cases; many radicular syndromes resolve without operation, and this is true even of cases in which medical imaging had found a herniated disk. Disk herniation can sometimes persist after the symptoms have disappeared, although resorption is also possible. Not only that; computed tomography (CT) or magnetic resonance imaging (MRI) examination frequently reveals a herniated disk in healthy individuals in whom it is of little relevance. It is only significant when it correlates with clinical findings.
To conclude, in the overwhelming majority of cases of back pain and associated clinical symptoms the morphological changes discussed above do not provide an explanation. For this reason this type of pain is referred to as ‘nonspecific’ (
Jayson 1970) or ‘idiopathic’ (without any morphological diagnosis).
The vast majority of cases of pain are not associated with demonstrable morphological changes in the locomotor system. In effect, therefore, these are patients with ‘no diagnosis.’
2.2. Theoretical aspects of manipulation therapy
The explanation originally given for the effect of manipulative therapy was that it involved ‘repositioning’; the understanding was that what was being treated was an incomplete dislocation, for which ‘subluxation’ became the accepted term. This was what Hippocrates believed, and probably also Still and most practitioners providing manipulative treatment down the ages. Indeed, the sight of a patient with acute lumbago or wry neck, unable to straighten up, who receives successful manipulation treatment and becomes able to stand erect, makes it little wonder that they did see this as the likely explanation. The reason that physicians have had to abandon the subluxation theory lies in the radiographic findings, since X-rays show no change for the individual segments before and after manipulation. The only change is in the abnormal posture, whose cause is muscular.
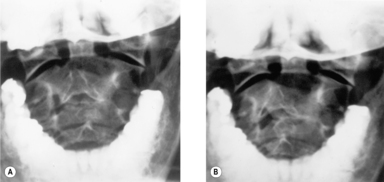
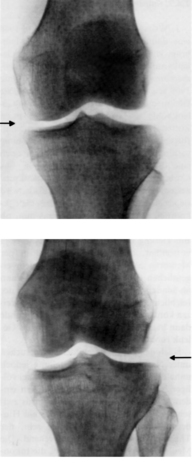
It has been shown by M Berger (personal communication) by means of cineradiography that when the head moves to an extreme position and back, it does not return to the same neutral position as before. We were able to confirm this by means of transoral radiography (see
Figure 2.1).
An analogous effect was demonstrated by
Jirout (1979a) for synkineses of the cervical spine in the sagittal plane on side-bending; when images were taken in the neutral position before and after maximum side-bending, the position of the spinous processes was generally found to be changed.
The conclusion that can be drawn from these observations is that in a structure consisting of such a number of mobile elements there can be
no absolute, fixed
neutral position. The same applies to any changes there may be following manipulation. It will be shown below that manipulation operates only on disturbed function, that is mobility in the affected motion segment. If, however, there is no absolute neutral position, it follows that manipulation enables the motion segments of the spinal column to adopt the position that is most favorable in the particular circumstances.
If the mobility of the motion segments of the spinal column is normal, the spinal column itself knows far better than the person giving treatment which position it should adopt for each particular posture or load.
According to the literature, some authors, such as Cyriax, Maigne, and Stoddard, believe that manipulation exerts some kind of effect on the disks. However, it is difficult to see how manipulation could achieve repositioning of a herniated disk when its exact position can never be known. Another point to consider is that manipulation is also effective in treating other locations, where there are no disks, such as the limb joints, the atlanto-occipital and atlantoaxial joints and the pelvis. Clinical experience supports this: manipulation is most effective in situations where there is no disk herniation, and often fails precisely in cases where there is.
The precise examination techniques used by osteopaths have also provided a clearer idea of the effect of manipulation therapies; these are indicated when we find movement restriction in a joint or a vertebral motion segment, and if manipulation is successful, normal mobility is restored. In other words, manipulation does not achieve a change of structure, as Still thought, but normalization of mobility; that is of function.
This is also true in cases of acute lumbago or acute wry neck: the position of the neck or the back in such cases is not in fact abnormal in itself; it is only the fact that the patient is unable to straighten from a position, such as flexion, or rotation plus inclination, that is pathological. Manipulation (mobilization) simply frees mobility and thus enables the patient to return to the neutral position. Acute lumbago and wry neck are in fact an exception in this regard; in the vast majority of cases the position observed is normal and the finding is simply one of movement restriction in the joint (or vertebral motion segment).
Manipulative techniques are used to diagnose and treat only functional movement restrictions in a joint or vertebral motion segment. The purpose of manipulation techniques is simply to normalize disturbed function.
2.3. The significance of functional disturbances
As the above makes clear, it is above all clinical experience in the use of manipulation for diagnosis and treatment that constantly reaffirms, in countless patients, the principle that treatment, if technically successful, brings normalization of restricted mobility in the joint or motion segment. Normalization goes hand in hand with the restoration of function (bending or rotation to the left or right; in the case of the limbs, symmetrical findings in the left and right limb). Normalization of function also brings relief of pain.
A similar principle applies not only to the passive mobility of joints, but also to active muscle function. Janda in particular demonstrated the significance of muscular stereotypes and showed that faulty movement patterns (disturbances of these stereotypes) produce abnormal stress on passive structures, especially joints.
Closely associated with movement patterns is the matter of body statics. In fact, static overload and its consequences have become an extremely important issue in our modern technologically developed society with its general lack of mobility. Here too we find that correction of faulty posture frequently relieves pain. The contribution made by Brügger is particularly helpful in this connection, since he has made a special study of the hunched sitting posture and its treatment.
Manual functional diagnosis thus served as a model for many other dysfunctions of the locomotor system. The muscle trigger point (TrP) most clearly demonstrates the close connection with pain. In saying so we should stress that morphological lesions are also associated with disturbances of function. This is most clearly the case for herniated disks and may explain spontaneous recovery and recovery after conservative treatment (including manipulation). A similar situation applies to rehabilitation in traumatology, where our primary aim is to improve function despite the presence of irreversible structural changes, where the aim of rehabilitation is to achieve functional compensation.
As will be shown in more detail later, function and its disturbances are rarely confined to one site or structure. Diagnosis must therefore take in the locomotor system as a whole, and consequently the terms ‘vertebrogenic’ or ‘spondylogenic’ will no longer suffice. Even in back pain, muscle function and its nervous control play an important role, as do the functions of the pelvis and lower limbs. Since ‘vertebrogenic’ diseases or lesions include such well-defined pathological conditions as ankylosing spondylitis and osteoporosis, the decisive criterion for the use of manipulation and other measures aimed at restoring function is whether the patient’s complaint is due (mainly or exclusively) to dysfunction, or to structural (pathomorphological) changes.
In many fields of medicine the significance of findings relating primarily to function is now well recognized. In the locomotor system, however, where function is paramount, this aspect finds least acceptance. Yet the functioning of the locomotor system is extremely complex, and diagnosis of disturbed function is correspondingly difficult. Nor is there a specific medical specialty responsible for this area; functional disturbances seem to be the realm of everyone and of no one. There is an additional disadvantage in that, for the most part, the only means of investigating dysfunctions of the locomotor system is by inspection and palpation. Today these are often regarded as ‘subjective’ and dismissed, while instrumental and laboratory methods are regarded as objective.
2.4. Motion segment and joint dysfunctions
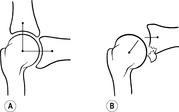
Dysfunctions of joints and vertebral motion segments (see
Figure 2.2) fall into two categories: hypermobility and restricted mobility; manipulative therapy is concerned only with
restricted mobility. Clinical criteria are the decisive factor in identifying such restriction, and are judged from the qualitative point of view as well as quantitatively. A reduced range of motion is easy to recognize and measure in a joint, but much more difficult in motion segments of the spinal column. Qualitative changes are therefore of considerable diagnostic value when dealing with the spinal column.
This is the case when the finding is one of increased resistance, and especially a lack of ‘springing’ at the end of the range of motion, with abrupt resistance encountered in the end position of the joint or motion segment. In a normal joint the extreme position is never reached abruptly, and a slight increase of pressure can always increase the range of motion. In a joint with functionally restricted mobility, this springing or giving way has been lost and we abruptly encounter a hard barrier. This, termed joint ‘restriction’ (sometimes ‘blocking’ or ‘blockage’), is perhaps the most significant sign in diagnosis.
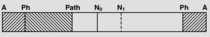
2.4.1. The barrier
The definition of the
physiological barrier given above is not universally accepted. It is defined in an osteopathic publication (
Kuchera 1997) as the limit of active motion. We consider this definition to be of no practical use on the grounds that passive examination of the barrier is used to investigate movement restrictions, both for motion segments and for joint play. The objection applies all the more to soft tissue diagnosis.
In chiropractic, this barrier is defined as the limit of maximum passive motion, the important point being that passive motion has a greater range than active motion. If manipulation were to be performed on a barrier defined in such terms, it would elicit an intense stretch reflex. This would rule out any gentle techniques, let alone relaxation on the part of the patient. Perhaps there is an explanation here for the harshness of technique used by some chiropractors.
The definition we have given above for the physiological barrier must therefore stand. It is useful both in diagnosis and as a principle that underlies our treatment, which produces release. We recognize fully that this does involve subjective evaluation. The first, minute resistance is found by means of palpation, which of course depends on the experience of the practitioner.
2.4.2. Joint play and restriction
There are two types of joint movement, both of which are affected by restriction:
1. Functional movement: movement that can also be performed actively.
2.
Joint play (according to
Mennell 1964): movement of the joint which can only be brought about passively. This comprises a translatory (sliding) movement of one joint surface against the other, sometimes also rotation, and also distraction of the joint facets.
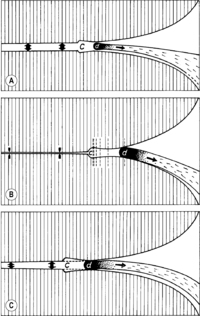
To give an example, actively we can flex, extend, or side-bend a finger, whereas passively it can be shifted against the metacarpal in any direction, rotated, or distracted by axial pull. These movements can not only be sensed by palpation, but can be demonstrated radiographically (see Figure 2.4 and Figure 2.5).
2.4.3. Reflex changes in joint restriction
Restriction in a joint and particularly in a vertebral motion segment produces reflex changes, mainly in the segment concerned, affecting the cutaneous and subcutaneous tissue and muscles.
Korr (1975) speaks of ‘facilitation’ in the segment.
From this we can conclude that, in their role as a brake,
muscles act as a considerable and highly variable impediment to mobility in a dysfunctional joint. Korr continues: ‘The high-gain hypothesis is consistent with, and offers an explanation for, the steeply rising resistance to motion (‘bind’) in one direction and the equally precipitous collapse of resistance (increasing ‘ease’) in the opposite direction … They [the muscles] would also be provoked into stronger and stronger contraction by the exaggerated spindle discharges as motions that tend to lengthen the affected muscles occur’ (
Korr 1975).
This would also explain the hard ‘feel’ in the end position. All the clinical findings encountered in restriction might therefore be explained as the result of muscle activity and not as a disturbance of the joint itself. That is why osteopaths prefer to speak of ‘somatic dysfunction’ (Greenman), a term that includes the dysfunction of the joint, the muscles, and the soft tissues.
The role of shortened muscles in movement restriction is emphasized by Janda. Muscle relaxation techniques are used with much success in order to mobilize joints. It is therefore appropriate at this point to consider the actual role of the joint in restriction.
2.4.4. Is restriction an articular phenomenon?
Clearly the view that passive movement is exclusively the expression of articular function is not one that can be maintained. In fact, as Korr has shown, most clinical findings in joint restriction can be explained by muscle activity controlled by the gamma system. If this is the case, what role is played by the joint itself?
If we are dealing with a reflex response, what is the origin of the stimulus that evokes it? It must surely be more than mere coincidence that techniques which have been found in a purely empirical manner to be effective in manipulation correspond to joint anatomy. The importance of joint play is also consistent with this, as is the fact that the popping sound, or ‘click,’ that is heard on successful manipulation comes from the joint. The hypotonus regularly observed following such manipulation is however a muscular phenomenon.
There are some joints that are not under the direct control of a particular muscle; obvious examples are the sacroiliac, the acromioclavicular and the tibiofibular joints. Yet muscular fixation of these joints (other than the acromioclavicular joint) is regularly found. In the case of the sacroiliac joint, for example, this is caused by the pelvic floor, the ischiocrural muscles, or the piriformis; in the tibiofibular joint by the biceps femoris.
In order to investigate further the role of the joint, we undertook the following experiments: in patients who were about to undergo operation under anesthetic with artificial respiration, the cervical spine was examined shortly before operation. Restrictions were found in ten patients, and the exact location and direction determined. The patients were re-examined under anesthesia, which used mainly thiopental, nitrous oxide and 100g succinylcholine iodide, the patients being in a state of complete muscle relaxation. This involved brief interruption of the intubation. In all cases the movement restriction remained unchanged during narcosis.
2.4.5. The possible mechanism of restriction and manipulation
The importance of the experiment just referred to lies first in demonstrating that the
joint does also play a part in
restriction; and second in showing that there is (also) a
mechanical resistance. It was
Emminger (1967) who first suggested that this might be attributed to a trapping of the meniscoids as previously described by Töndury and others.
Kos & Wolf (1972) showed in addition that these meniscoids do also exist in the limb joints.
The physiological
role of the meniscoids is to fill the changing joint space as it alters during movement, since they are a highly mobile structure. Most joints have very incongruous facets; without the meniscoids to perform this role, gapping of the joint would occur during movement. The meniscoid is intimately connected with the joint capsule. Clearly such well-nigh chaotic-seeming motion must be prone to disturbance. However,
Cihák (1981) points out that the deep layers of the multifidus muscles are linked with the joint capsule and so control this mechanism.
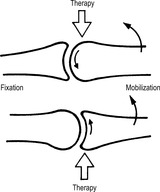
This diagram clearly illustrates the mechanism of manipulative techniques. High-velocity, low-amplitude (HVLA) techniques cause gapping of the joint capsule, as a result of which the meniscoid has only a short constricted area to overcome (Figure 2.9). In repetitive mobilization, the meniscoid is freed during the back-and-forth movement of the joint facets, and all that is apparently needed as we wait for release to occur is the relaxation of the muscles, which widens the joint space.
2.4.6. The effect of manipulation
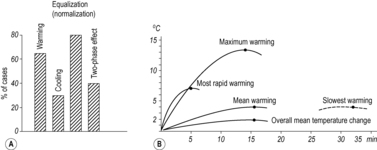
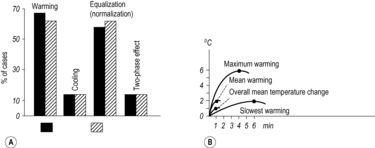
The
effect of successful
manipulation is two-fold:
1. It restores mobility, including joint play.
2. It produces an intense
reflex reaction in all structures where changes had been present before manipulation. This occurs most strongly in the musculature, where a previous state of increased tension (TrPs; occasionally spasm) is replaced following manipulation by hypotonia. The skin, too, becomes easier to fold and stretch, and soft tissues easier to shift against each other. Tension is thus reduced in all tissues, especially in the corresponding segment. Depending on the significance of the vertebral motion segment or the joint concerned, the effect of the manipulation also extends to distant segments; this will be discussed later. The effects referred to here can not only be observed clinically, but can also be objectively demonstrated by physiological methods (see
Figure 2.10,
Figure 2.11,
Figure 2.12 and
Figure 2.13).
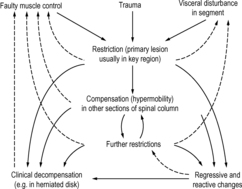
2.4.7. The pathogenesis of restriction
Overload and abnormal load
Modern civilization brings with it very one-sided, unvaried posture and movement, causing muscular imbalance. Lack of movement together with static or postural overload are a characteristic feature of modern life. Disturbed movement patterns and static overload are probably the most frequent causes of reversible restrictions and of their occurrence and recurrence.
Trauma
Trauma is a further potential cause. It is important to point out that the borderline between patient groups suffering from overload and those suffering the effects of trauma can in fact be very fluid, because it is not always easy to say what should and should not be interpreted as trauma. It is usually defined as a force acting on the body and capable of damaging structure or function. However, even under normal conditions the forces acting on the spinal column are considerable. If these forces are suddenly increased because of sudden, unexpected movement, especially if this involves contraction of the powerful muscles of the back, it becomes extremely difficult to distinguish between overload and trauma. The somewhat vague term ‘microtrauma’ is then used.
Reflex processes
A further complex of causes involves
reflex processes within the segment. As has been stated already, the spinal column is routinely involved in disease processes in the body. Vertebral restrictions can therefore occur following – and also as a result of – disease elsewhere in the body. The primary condition creates a stimulus in the segment, which in turn produces a spasm (TrP) in the corresponding region of the erector spinae muscle, in particular in the deep layer. The effect is muscular fixation of the vertebral motion segment: a restriction. This is the same mechanism that, according to
Hansen & Schliack (1962), leads to scoliosis in visceral disease.
Today it is possible to distinguish a number of characteristic patterns related to visceral disease (see
Chapter 7) which points to certain pathogenetic rules. Another characteristic feature of this type of restriction is its recurrence if the internal disease relapses or exacerbates. Admittedly, however, we know more about visceral influence upon the spinal column than about the influence of the spinal column on visceral organs.
2.5. The spinal column as a functional unit
The most important
functions performed by the spinal column are:
• giving support and protection to neural structures
• being the axis of motion for the body
• helping to maintain the balance of the body.
As we can see from the first two functions listed, these roles are contradictory; Gutmann (1965) expressed this succinctly when he said: ‘the spinal column should be as mobile as possible and as firm as necessary.’ The implications of this become clear when we consider the remarkable range of movement of the atlanto-occipital and atlantoaxial joints, and the fact that vital centers of the medulla oblongata are located at this level; these twin facts explain why disturbances of these two basic functions are linked. If a dysfunction produces a pain stimulus, a muscular defense reaction blocks the damaging movement. A spinal column with restricted mobility is no longer properly able to carry out its protective function. The effects extend to the structures of the nervous system, which in turn exerts an effect on the spinal column that is causing the damage to them. Sobotka (1956) demonstrated that damage to a nerve root causes trophic changes of the intervertebral disks. The function of the spinal column affects not only the structures inside the spinal canal, but also the entire locomotor system, including the limbs, and probably also internal organs. The existence of all these functional interconnections means that the spinal column should always also be considered when the object of concern is the pelvis, limbs, or especially the muscles under central nervous system control.
2.5.1. The spinal column and balance
The importance of the spinal column in the
maintenance of balance is usually underestimated. This applies in particular to the
craniocervical junction. It is often forgotten that the labyrinth is not absolutely essential for the maintenance of balance and posture, whereas proprioception is, especially in the spinal column. Clinical evidence confirms this (see
Chapter 7). The experiments carried out by
Norré and coworkers (1976), using
Greiner and coworkers’ (1967) flexible-support chair, are particularly valuable in this respect. The method they used involves keeping the subject’s head fixed in position while turning the trunk from side to side with a pendular motion. They were able in this way to produce nystagmus, purely by stimulation of the cervical proprioceptors (
Greiner et al 1967,
Hülse 1983,
Moser et al 1974,
Norré et al 1976,
Simon & Moser 1976).
The effects are not limited to the cervical spine.
Komendantov, 1945 and
Komendantov, 1948 demonstrated in rabbits that
tonic reflexes can originate not only from the neck but also from the lumbar spine. He distinguishes the lumbosacral-eyes and lumbosacral-head reflexes. On side-bending of the animal’s trunk in the lumbar region around a dorsoventral axis, with the upper body and head fixed, the eyes move in the opposite direction to the trunk. If the head is not held fixed, there is an additional slight turning of the head, also in the opposite direction. Leads from the muscles of the nictitating membrane and the rectus muscles (of the eye) showed this to be a tonic reflex. Komendantov’s experimental design enabled him to make neck and lumbosacral reflexes compete, with the neck reflexes usually proving stronger. However, the effect was dependent on the extent of side-bending; the greater the side-bending, the stronger the effect. Interestingly in the course over time, it was seen that immediately following the effect of a neck reflex, even a relatively weak lumbosacral reflex can also assert itself. This mechanism apparently enables the animal to keep the visual field constant during locomotion, despite the motion of the head and trunk. The reflexes therefore have very short transmission times; changes were still being registered in the activity of the muscles investigated, even at a side-bending frequency of 200 side-bends per minute.
These experiments demonstrate that the spinal column is a
functional unit governed by reflex response; if certain changes in position or function occur at one end of the spinal column, these exert an instant reflex effect along the entire spine. It should be stressed that, in humans, both ends of the spinal column are held relatively constant: in the case of the pelvis this is achieved because of the length of the legs; in the case of the head, through reflex fixation of the plane of the eyes and labyrinth in space. This preservation of the head position is strongly maintained as a movement pattern (motor stereotype).
Ushio and coworkers (1973) demonstrated the deleterious effect of low-back pain on vertigo and the beneficial effect of immobilizing the lumbar spine in lumbago.
2.5.2. Key regions of the spinal column in dysfunctions
So far we have considered restriction and its origins without reference to its effects on the rest of the spinal column. This, however, would be to ignore one of the most frequent causes of restrictions: a restriction or trigger point in another section of the spinal column. These bring about a compensatory increase in mobility in the neighboring segment, which leads to overload and ultimately a further restriction.
Chain reactions therefore come about, which explains why vertebrogenic disturbances tend over time to involve the entire locomotor system. Therefore we should always examine the entire spinal column, at least in terms of screening assessment. It is important to realize, not least in this respect, that not all vertebral segments have the same importance for the overall function. When performing a brief assessment we should therefore focus on ‘
key regions.’ In most cases these are
transition zones from one type of movement to another:
• The cervicothoracic junction: this is the region in which the most mobile section of the spinal column meets the relatively rigid upper thoracic spine. It is also the place where the powerful muscles of the shoulder girdle have their attachment, providing the main connection with the upper limbs and explaining why this region is particularly susceptible to dysfunctions.
• The middle thoracic spine is to some extent the ‘weak point’ of the muscles of the back, since the lumbar and cervical parts of the erector spinae muscles end here, and kyphosis is usually greatest at this point.
• One of the reasons for the considerable load borne by the thoracolumbar junction is that here the mechanism of motion typical of the thoracic spine changes within a short distance (at vertebra T12) to the lumbar pattern. This can be seen from the difference in shape of the upper and lower articular processes. If during walking the pelvis tilts from one side to the other, the lumbar spine side-bends so that the vertex of the scoliotic curve lies at the level of L3, the thoracolumbar junction remaining vertically in line with the sacrum; the thoracic spine then forms a scoliotic curve in the opposite direction. Consequently the thoracolumbar junction does indeed represent a junction.
• The lumbosacroiliac joint region forms the base of the spinal column and is therefore extremely important to spinal column statics. At the same time the sacroiliac joints transmit movement from the legs to the spinal column and act as shock absorbers.
• In humans the feet are the body’s actual base; also the greatest density of proprioceptive, exteroceptive, and nociceptive receptors is found there. Dysfunctions in this region consequently have an effect on the whole of the locomotor system; they should not be overlooked.
2.5.3. The importance of nervous control
The spinal column could not act as a functional unit unless all its reactions were coordinated, under control of the nervous system. Certain kinds of posture and movement sequences play the major role in this respect; these, following the proposal of Janda, are termed ‘motor patterns.’ These motor stereotypes are so characteristic of an individual that we can recognize people by their gait. There is considerable variation in the quality of these patterns, and this goes hand in hand with the susceptibility to disturbance of the locomotor system in the individual case. Any disturbance of function in a single motion segment will have its repercussions throughout the spinal column and must be compensated. The decisive role in this is played by the nervous system, which is similarly important in the matter of pain, for it is the nervous system that determines how intensely the segment will react, and where the threshold of pain lies. In other words, it is the nervous system that determines whether the dysfunction will manifest itself clinically. If the reaction to the nociceptive stimulus is intense, dysfunction in one motion segment will produce an antalgic response and alter the normal movement pattern, causing the dysfunction to become fixed, so that the condition becomes chronic.
It is, therefore, no coincidence that dysfunctions of the motor system are more likely to be found in
subjects with labile nervous regulation, and this tends to be evidenced psychologically as well. The point was emphasized by
Gutzeit (1951), who saw the psychological factor as being characteristic for patients presenting with vertebrogenic disturbances.
Kunc and coworkers (1955) showed that the psychological condition of patients plays a major part in recovery after disk operation. They demonstrated by means of experiment that these patients very easily formed conditioned reflexes to other pain stimuli, and that these reflexes were more difficult to extinguish than in healthy controls.
Šrácek & Škrabal (1975) observed two groups of psychiatric patients: 50 cases of neurosis with symptoms of anxiety and depression, and 25 schizophrenics with blunted affect. Restriction, most frequently in the cervical spine, was absent in only 5 neurotic patients and in 16 schizophrenic patients. This difference is statistically highly significant (
p<0.01). Buran & Novák (1984), studying a group of 105 chronic patients, distinguished constitutionally neurotic and psychopathic patients from those who were psychologically normal. They found a preponderance of the fatigue reaction in the electromyogram (EMG) in the neurotic patients, and more frequent occurrence of positive F-waves, indicating a correspondence between psychological lability and labile nervous regulation. Lisý (1983) found similar results in EMG studies of patients with cervical syndrome.The clinical findings made by
Janda (1978) are also worthy of note: in 100 patients with poor motor patterns, he found:
• minor neurological signs of ‘microspasticity,’ in which movements were not fully coordinated, appearing as clumsiness
• slight sensory impairment, especially of proprioception
• poor adaptation to stress situations and inadequate, ‘uncoordinated’ behavior.
All these clinical signs correspond to ‘minimal brain damage’ (MBD). Found in 10–15% of the child population, this is quietly assumed to disappear without trace in adulthood. However, Janda’s findings suggest that this brain dysfunction is in fact manifested in adult patients in the form of vertebrogenic disorders, poor motor patterns, and a considerable degree of labile nervous and emotional regulation.
Despite the role played by muscular imbalance and faulty neural control, these should not be equated with joint dysfunction or restriction of a vertebral motion segment. Dysfunctions of the joints or vertebral segments do occasionally appear even in subjects with good motor patterns, yet may be absent in patients with neurological disease.
Tilscher and coworkers (1979) found that of 27 spastic subjects, only 18.5% complained of backache. In our experience, most patients with Parkinson’s disease complain of backache; this is clearly associated with the muscle rigidity, which also affects the spinal column.
Faulty neurological and psychological control are among the factors involved in the pathogenesis and clinical signs and symptoms of locomotor dysfunctions. However, they are not identical with them.
The importance of developmental kinesiology
It is no coincidence that Janda associates disturbances of motor pattern in adults with disturbances of the central nervous system in infants. Developmental kinesiology can indeed help us better understand the pathogenesis of dysfunctions, especially the effects that a structure belonging to the locomotor system can exert on distant regions; in other words, on the entire system. In this context we shall attempt to present the essential thinking of
Vojta & Peters (1992) and
Kolář, 1996,
Kolář, 1999 and
Kolář, 2006 on the present subject.
Neurophysiology today has no explanation for the effects exerted on each other by parts of the locomotor system that are situated far apart, which are found as a matter of everyday experience in manipulative therapy; nor can it explain the chains of trigger points. The principles governing these can however be explained by developmental kinesiology.
The
first reflexes in the
newborn (stepping reflex, crossed extension reflex) are spinal cord reflexes. They offer no stability and do not enable posture of any kind. The first postural reflexes arise when the infant begins to observe its surroundings, raising and holding up its head. This is the point when the flexion posture of the newborn (see
Figure 2.14) is brought into balance with the developing extensors. This development is complete roughly at the end of the third month (see
Figure 2.15).
The extensor system is therefore younger in developmental terms than the ‘tonic’ flexor system, and therefore more susceptible to disturbance. This explains why the tonic system always predominates in pathological states, pain, and even in mere fatigue. Both systems are involved in upright posture; it is therefore inappropriate to use the term ‘postural muscles’ for the tonic system alone. The decisive issue is which system is older or younger in developmental terms.
This course of development gives rise to the coactivity of antagonists, which enables balanced, upright posture and can be seen at two levels. As an example, the erector spinae is the antagonist that corresponds to the pectoralis major muscle. The relationship is so specific that certain bundles of fibers of the pectoralis major correspond only to certain bundles of fibers of the erector spinae. The same kind of correspondence applies to adductors and abductors in the limbs, for instance. Clinically this is seen in the localization of trigger points. However, this antagonism applies not only to individual muscles, but to the entire system. This fact is extremely important: stimulation of a muscle that belongs to the extensor system inhibits the whole of the flexor system. The effect can most clearly be seen when stimulation is applied to one of the points where most receptors are located, such as the fingers and toes. To give an example, stimulation of the finger extensors can produce inhibition in the straight-leg raising test.
The coactivity pattern relates to upright posture as a whole. Muscles that maintain the position of the head over the shoulders have their fixed point of attachment in the region of the shoulder girdle, the muscles of the thorax and scapula in the pelvic region, and the muscles of the pelvis in the region of the lower limb, down as far as the foot. As soon as the position of one of these superposed sections changes, the entire system has to react. Control of these reflex processes in the maintenance of human upright posture is located above the brainstem; it has been little researched experimentally.
The long chains of antagonists which subserve upright posture act on the spinal column like ropes stabilizing a mast. However, unlike a stiff mast, the spinal column is formed by 24 vertebrae and the sacrum which, according to
Panjabi, 1992a and
Panjabi, 1992b, are unstable and would buckle under the strain. This is prevented by what is called the ‘deep stabilization system.’
Another system that is developed only in humans is that of the ‘deep stabilizers,’ which serves to maintain the upright posture of the spinal column. It consists of the deep layers of the erector spinae and transversus abdominis muscles, the diaphragm, and the pelvic floor. The last three of these support the abdominal wall. The abdominal cavity and its internal pressure provide the anterior support of the lumbar spine. In humans, the diaphragm plays a significant role as a postural muscle; only in humans is there a close link between respiration and posture, with the diaphragm lying horizontally.
A further function, which develops relatively late in infants (after the sixth month) and which is therefore also susceptible to disturbance, is (active)
rotation of the trunk. This plays a particularly important role in humans, since the most forceful movements, such as throwing a discus or boxing, proceed from a rotation of the trunk. At every step the shoulder girdle rotates in the opposite direction to the pelvis. The significance of this movement can be seen in the rehabilitation of leg amputees and paraplegic patients, because it is this mechanism that enables them to learn to walk. According to
Farfan et al (1996), however, the spinal column is less well adapted to rotation movements in terms of its constituent parts; this applies especially to the intervertebral disks.
2.6. Dysfunctions of the spinal column in childhood
From what has been said it follows that dysfunctions are regarded as primary phenomena in the pathogenesis of vertebrogenic disorders. Hence studies try to investigate them in their pure form, that is
in the absence of degenerative changes, which can be done by studying them in
children and young people.
Schön (1956) and later
Gutmann & Wolff (1959), have shown the average age at which the first symptoms appear to be much earlier than the age when they become evident radiographically. Dysfunctions, however, appear at the same time as clinical symptoms.
The most typical clinical condition in children is cervical myalgia (acute wry neck). Although this usually remits spontaneously, traction and gentle mobilization techniques, if well applied, should give immediate relief. This is particularly true for neuromuscular techniques.
In children with
headache, the cervical spine plays an important role. This is true of various types of headache, including
migraine. In a group of 30 children suffering from vasomotor headache, manipulation produced improvement in 28 cases.
Janda (1959) reported similar success following traction of the cervical spine. In a group of 27 children suffering from migraine, only 3 failed to respond to manipulation treatment (
Lewit 1959). Similar results were reported by
Kabátníková & Kabátník (1966). A particularly important type of headache in children, known as ‘school headache’ and generally believed to be of psychological origin, was proved by
Gutmann (1968) to be due to head anteflexion during school hours, when the children were reading and writing at horizontal desks. This was confirmed by
Lewit & Kuncová (1971).
One clinical manifestation of disturbed function in the lumbosacral and pelvic region frequently found in young girls is dysmenorrhea with negative gynecological findings; this can frequently start as early as the menarche. Patients complain not only of pain in the lower abdomen; they also experience low-back pain. Manipulative therapy is the treatment of choice in such cases. The point should be made here that dysmenorrhea at an early age is frequently the first sign of dysfunction of the spinal column in women.
True lumbago is much less frequent in childhood, but there are rare cases of true disk herniation as early as puberty. With the exception of acute wry neck, dysfunctions in the spinal column tend to be manifested indirectly in the form of referred pain, as headache, and in girls as dysmenorrhea.
We were interested to see how frequently dysfunctions could be found in healthy children of different age groups. The most striking finding in children and adolescents is
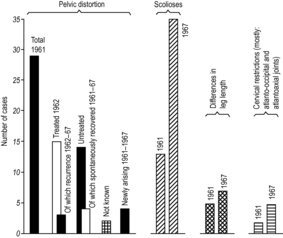
pelvic distortion which is dealt with in detail in later chapters. In serial studies we found this in 11 of 80 children (aged 14–41 months) examined in crèches, in 81 out of 181 children (aged 3–6 years) in nursery school and in 199 out of 459 schoolchildren aged 9–15 years. Statistical evaluation showed no significant difference between the incidence in boys and girls.
Movement restriction in the cervical spine (mainly at the atlanto-occipital and atlantoaxial joints) was found in none of the infants in crèches, in only 8 out of 181 nursery school children examined, and in 73 of the 459 schoolchildren. These investigations were carried out over 40 years ago, when the technique of examination for the upper cervical spine was much less sophisticated than it is today. It has since been found that pelvic distortion in children is generally associated with craniocervical joint restriction, mainly in the C0/C1 segment; there is normalization of the pelvic findings after the C0/C1 joint has been treated. In 1982 we therefore examined a group of 75 nursery school children (aged 3–6 years). We found pelvic distortion in 24, of whom 23 had movement restriction of C0/C1. In 12 of these children manipulation of the craniocervical joints was carried out, following which there was normalization of the pelvic distortion in all cases. There is thus good reason to believe that most of the children in whom we found pelvic distortion in the examination we performed over 40 years ago also suffered from restriction at the craniocervical junction. We also found slight scolioses in 175 of the 459 schoolchildren examined at that time, and in 15 out of the 181 nursery school children. Among the children in crèches, this finding was made in only 1 out of 80 children.
The overwhelming importance of the
craniocervical (
atlanto-occipital and atlantoaxial)
joints in infants was pointed out by
Seifert (1975). In children in whom function is normal, they found that, on turning the head to one side, the pelvis turns to the opposite side. This reaction was absent in 298 of the 1093 infants examined. Over a period of 4–9 months restriction of the
atlanto-occipital and atlantoaxial joints was found in 58% of this group.
Biedermann (1993) described what he termed ‘KISS syndrome,’ characterized by a forced attitude of the head in the side-bending position, often found in association with considerable somatic and autonomic disturbances. These he treated by manipulation. In a study group of 76 children suffering from chronic tonsillitis,
Lewit & Abrahamovič (1976), found restriction of the
atlanto-occipital and atlantoaxial joints in 70 (92%) of the subjects, mainly in the C0/C1 segment.
In evaluating these results we needed to discover whether they were chance findings or represented continuing, constant dysfunctions. In collaboration with Janda we therefore followed up a group of 72 children who started school attendance in 1960, carrying out regular examinations over a period of eight years. Half the number with dysfunctions of the spinal column were treated, and the other half left untreated as controls. In addition to the spinal column, the rest of the locomotor system and particularly the musculature were tested. The results are summarized in
Figure 2.17.
2.7. Restrictions and their sequelae
If a restriction occurs in the intact terrain of the spinal column of a child or an adolescent, for example, the
consequences may seem at first sight to be minor: there may be some transitory pain, which usually disappears quickly as tends to be the case with acute wry neck. The dysfunction is compensated. Of course, a restriction occurring in the rest of the locomotor system, particularly the limbs, becomes clinically evident immediately. In the spinal column, consisting as it does of complex parts (54 intervertebral joints, including the atlanto-occipital and atlantoaxial joints and the sacroiliac joints), the lack of mobility of a single joint or motion segment can go unnoticed. There is, however, a price to be paid for this capacity of compensation: increased demands or abnormal stress on the compensating structures. This becomes especially evident when the restriction occurs in a key region (see Section
2.5.2), because neighboring regions cannot easily compensate. As mentioned previously, restriction of rotation between the atlas and the axis means that their role in the rotation of the head has to be taken on by the rest of the cervical spine, which is far less suited to the task. This may help explain why osteochondrosis of the lower cervical spine is so commonly found.
As a general principle, then, movement restriction in one segment produces
hypermobility in its neighbor, and this is most marked in the case of restrictions in key regions. The most frequent consequence of chronic overload is the formation of osteophytes to stabilize the motion segment. The lack of motion in the restricted segment often leads to disturbances of
trophicity, which particularly affects bradytrophic tissues such as ligaments and disks. This is confirmed by radiographic evidence, which shows osteophyte formation in temporarily hypermobile segments (above block vertebrae). The usual findings in restricted segments are that two adjacent vertebrae form a block with the narrowed disk showing degenerative changes.
Müller (1960) have shown how the hypermobile segment, initially created to compensate for a hypomobile one, stiffens in its turn as a result of osteophyte formation, so that the osteochondrosis spreads from one vertebral segment to the next. The stabilizing role of the osteophytes, which are plate-like in shape, can best be seen in chronic spondylolisthesis.
Degenerative changes in themselves need not produce clinical symptoms. They do, however, make the spinal column more susceptible to disturbance, and the same applies to dysfunctions. Even patients with degenerative changes experience no symptoms as long as function remains compensated, but there is a risk of decompensation. This explains why the sequelae of trauma are usually more severe when degenerative changes are already present. Frequently, what are called degenerative changes are better described as adaptive ones, or an attempt to compensate dysfunction.
One important sequela of degenerative changes can be a herniated disk. Here too there is a close relationship between structural change and dysfunction. With modern imaging techniques we find that disk herniation revealed by CT or MRI need not be accompanied by any symptoms; also that, in cases where the herniated disk does produce pain, the clinical symptoms may disappear despite the fact that the herniation continues to be evident on CT or MRI examination. The relationship between function and structural pathology is clearly very complicated here. Nevertheless, in cases of disk herniation, dysfunction can be treated at joints and trigger points, in soft tissue and in the stabilization system, to produce clinical compensation.
2.8. The significance of disturbed motor patterns (stereotypes)
Disturbed motor stereotypes are perhaps the most important factor in the etiology of functional, reversible restrictions. This would make remedial exercise the treatment of choice and especially the best means of prevention. It is less clear what the actual content of such therapy should be when treating – usually painful – dysfunctions of the locomotor system, since remedial exercise expects to deal with a well-defined lesion (for example paresis), and that is not what we are dealing with here.
It was Janda who first addressed this problem. The main object of remedial exercise in dysfunctions of the locomotor system is the correction of faulty motor patterning (disturbed movement patterns or stereotypes), that is faulty coordination of muscle function due to disturbed central nervous control. The problem here lies in defining what is the norm, since these movement patterns are very different and highly individual, consisting of programs built up by each subject in the course of life on the basis of chains of unconditioned and acquired (conditioned) reflexes. The way each individual moves is so characteristic that we can recognize people by their gait, their gestures, or their handwriting. Ideally, motor patterns should allow movement to be as economical as possible, that is to consume the smallest possible quantity of energy.
As in many other situations, it makes sense for our purposes to take the dysfunction as the starting point. Even a layman will recognize awkwardness of movement, and, more often than not, such movement is uneconomical in energy expenditure; therefore the layman is also able to correct the most obvious aspects – just as sports trainers, for instance, correct the movements of sportsmen and women.
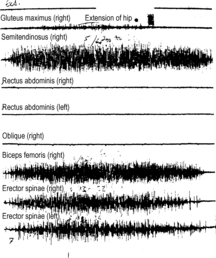
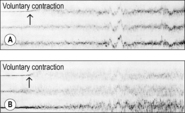
In patients with vertebrogenic pain, Janda systematically applied the classic
muscle test to the individual muscles involved in particular movements. His results revealed that the simple movements used to examine muscle function in fact study a (fairly simple) movement pattern, involving a number of muscles, rather than a particular individual muscle. Examining hip extension by polyelectromyography, Janda showed that it is not only the gluteus maximus muscle which contracts in hip extension, as had been thought, but that the ischiocrural muscles are the first to contract, followed shortly afterwards by the erector spinae. The typical disturbance of movement pattern found in hip extension is the belated and inadequate activity of the gluteus maximus (see
Figure 2.18).
We learned over time to recognize in clinical examination which muscles actually take part in simple test movements, by means of palpation. This enables us to assess not only muscle force, but also quality of performance. This quality may be considerably altered while force remains normal. The strength of hip extension may remain normal, even if it is carried out only by contraction of the ischiocrural muscles and the erector spinae. In this case there is considerable disturbance of the movement pattern, with important consequences for locomotor function, as will be explained later.Regular testing of simple movements using the muscle test revealed a surprisingly
constant pattern: certain muscle groups repeatedly showed a tendency to lesser activity (weakness) and hypotonia, whereas others equally regularly tended to hyperactivity and tension. This resulted in
characteristic patterns of imbalance which are so constant and typical that we can identify them as syndromes with a clinical significance. They are each characteristic of a particular clinical picture: in some cases there is a preponderance of weakness, flabbiness going hand in hand with hypermobility, whereas in others there is increased muscle tension and stiffness.
Table 2.1 sets out those muscles with a tendency to hyperactivity and those that tend to hypoactivity.
Table 2.1 Muscle groups exhibiting a tendency to hyperactivity or hypoactivity
| Hyperactivity |
Hypoactivity |
| On the dorsal aspect of the body |
| Triceps surae |
Gluteal muscles |
| Ischiocrural muscles |
Inferior part of trapezius |
| Lumbar section of the erector spinae |
Serratus anterior |
| Quadratus lumborum |
Supraspinatus |
| Superior part of trapezius |
Infraspinatus |
| Cervical extensors |
Deltoid |
| On the ventral aspect of the body |
| Thigh adductors |
Tibialis anterior |
| Rectus femoris |
Extensors of the toes |
| Tensor fasciae latae |
Peronei |
| Iliopsoas |
Vasti |
| Obliquus externus |
Rectus abdominis |
| Pectoralis major and minor |
Deep neck flexors |
| Subscapularis |
Digastric |
| Scalenes |
|
| Sternocleidomastoid |
|
| Masticatory |
|
| Upper limbs |
| Flexors |
Extensors |
This difference in the behavior of these two muscle groups can be seen under various clinical conditions and is regularly found in painful states: in a painful hip it is always the flexors and adductors that are tense and the glutei weak; in shoulder pain the pectoralis and subscapularis muscles and the superior part of the trapezius are taut whereas the supraspinatus, infraspinatus, and deltoid muscles are weak; in chronic painful conditions of the knee the vasti are atrophic while the rectus femoris is like a tight band.
The findings are similar for fatigue: again the same muscles will be inhibited and their activity frequently taken over by those with a tendency to hyperactivity. This behavior continues to be found in central paresis, when again we find that muscles with a tendency to hyperactivity become spastic, and those with a tendency to hypoactivity become flabby. Neurologically, this kind of muscle imbalance can be termed ‘microspasticity.’
Janda referred to those muscles with a tendency to
hypoactivity as predominantly ‘
phasic,’ and muscles with a tendency to
hyperactivity as predominantly ‘
postural.’ In terms of developmental kinesiology (see Section
2.5.3), those of the first group belong to the younger system and the second group to the older one. It should be stressed that there is no substantial difference between the types of muscle fiber or the biochemistry of these two groups; the physiological reason for the difference between them rests on the
developmental kinesiology. Both systems evidently have a postural function. Examination of simple movements by applying the muscle test is no more than the first step in investigating muscle function; our habitual movements are individually acquired patterns or stereotypes.
The concept of patterning is clearly illustrated by looking at antagonists. For example, the ischiocrural muscles and the quadriceps femoris can be considered as antagonists if we are thinking of the movement of knee flexion and extension. However, during walking both these muscle groups are acting primarily to stabilize the leg. A similar principle applies to the abdominal and back muscles, and to the flexors and extensors of the cervical spine. In fact, in well-coordinated straightening up from a stooping position it is mainly the deep abdominal muscles that provide stability, a point to be remembered in remedial exercise. It should be stressed here that when treating muscle imbalance involving a predominance of the muscles that regularly tend to hyperactivity, the effect of strengthening the weakened (hypoactive) muscle is not only experienced in the particular segment but also influences the overall balance between ‘phasic’ and ‘postural’ muscles. This is particularly important where there is a greater density of afferent nerve receptors, so that afferent stimuli are more strongly felt; it is the case at the fingers and toes, as Brügger has shown. He found that, following stimulation of the extensors of the fingers and toes, the patient finds it easier to resume upright posture; one of the other consequences is improvement in the straight-leg raising test.
The training of different movement patterns involves the interplay of a number of muscles reacting in sequence, whose reaction can be triggered if specific stimuli are employed. For movements of the limbs, stimulation of the periphery is most effective, since receptors are numerous here. To facilitate walking, lifting the big toe is helpful: the patient will then find it easier to dorsiflex the foot; that in turn helps the flexion of the knee and hip. Similarly, flexion of the fingers helps anteversion of the elbow and shoulder. What the fingers and toes are for the function of the limbs, the eyes are for the trunk: looking up facilitates straightening of the body, looking down facilitates bending forward, while looking to the side facilitates rotation. Furthermore, as straightening of the body is connected with inhalation, and bending forward with exhalation, it is enough for the patient to look up to facilitate inhalation (as when sighing). Similarly, directing the gaze downward assists exhalation.
Returning to the question of imbalance between those muscle groups which are older and those which are younger in developmental terms, the problem here is a form of defective coordination. This is particularly so in the interrelationship of antagonists, where the hyperactive muscle generally has an inhibitory effect on its weak antagonist. For example, hyperactive lumbar erector spinae muscles inhibit the abdominal muscles, and hyperactive adductors the glutei. This disturbs the centering of the joints involved, imposing excessive stress on them.
2.9. Sequelae of disturbed movement patterns
Having looked in detail at the nature of disturbed movement patterns, we now turn to the mechanisms by which they impair the locomotor system.
2.9.1. Walking and standing
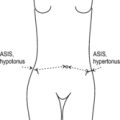
The most frequent findings here are an imbalance between weak gluteal muscles and hyperactive hip flexors, between hyperactive lumbar erectores spinae and weak abdominal muscles, and between hyperactive adductors and weak abductors of the hip. In standing we see increased pelvic tilt, a protruding abdomen, and lumbar hyperlordosis.
The actual pathogenic mechanism in standing is overload of the lumbar spine as a result of increased tension of the erector spinae muscles; in walking, overload results mainly from the fact that pelvic tilt places the hip joints in extension, and also from the weak gluteus maximus. As a result, the extension of the patient’s legs in walking is mainly achieved by extending the lumbar spine still more. This produces hypermobility of the lumbar spine in the sagittal plane. Hyperactivity of the adductor muscles and above all the weak gluteus medius causes instability in the frontal plane, especially when the patient is standing on one leg. The result is increased swaying of the pelvis from side to side while walking; causing, in other words, hypermobility and overload of the lumbar spine in the frontal plane.
2.9.2. Straightening up from a forward-flexed position
If the trunk is imagined as a straight lever with the L5–S1 disk as the fulcrum, calculation of the
stress involved during weight-lifting has produced values of 1000kg and above (Matthiasch 1956, Morris 1973). Such a force is more than the disk could bear. Measuring intradiskal pressure, Nachemson (1959) found that the pressure during weight-lifting from a sitting position was 275% of that when standing upright. The reason, according to Gracovetsky (1988), lies in the role of the lumbodorsal fascia, into which the erector spinae, the glutei, and the ischiocrural muscles fan out. The tension from the ischiocrural muscles enables the spinal column to ‘hook in’ to this fascia, as it were, so that the lever effect is eliminated. This mechanism is further supported by the abdominal muscles, which also fan out into this fascia and in addition draw the thorax toward the pelvis and maintain intraabdominal pressure. The effect is that the correct movement pattern assists this ‘unreeling’ mechanism and avoids the lever effect.
2.9.3. Raising the arms
Here the decisive factor is correct fixation of the shoulder girdle; this is the function of the superior part of the trapezius and the levator scapulae from above, and of the inferior part of the trapezius and the serratus anterior, the first two muscles being attached to the cervical spine and the last two to the thoracic spine.
The faulty movement pattern typically found here is tension in the muscles providing fixation superiorly and weakness of those providing stabilization inferiorly. The effect is to lift the shoulder blades and place excessive load on the cervical spine.
2.9.4. Weight carrying
The key factor here from the point of view of the biomechanics is the position of the shoulder joint: if the shoulder of the weight-bearing arm is behind the line of gravity of the body, the shoulder girdle is fixed at the thorax by the serratus anterior, the inferior part of the trapezius, the rhomboid major and rhomboid minor. If the shoulder is in a raised and forward position, then the muscles providing fixation are the superior part of the trapezius and the levator scapulae, placing undue load on the cervical spine and at the same time to destabilize the lumbar spine. It is the upright positioning of the head that ensures the correct position of the shoulder.
The muscular imbalance involved here is a hyperactive pectoralis major, in particular the clavicular head of the muscle, hypoactivity of the weak rhomboid and serratus muscles and the inferior part of the trapezius, and increased activity of the superior part of the trapezius and the levator scapulae. The hyperactivity of the pectoralis major causes kyphosis in the lower part and hyperlordosis in the upper part of the cervical spine.
These examples illustrate the pathogenic effects of faulty movement patterns on the locomotor system and spinal column. The motor stereotype which leads to the most marked consequences, however, is faulty breathing.
2.9.5. The effect of respiration on the locomotor system
When we think of respiration, we tend to focus almost entirely on the organs of the respiratory system. In doing so, however, we forget that the thorax and diaphragm are essential to the function of the lungs. The locomotor system has to coordinate the specific function of respiratory movement with the function of locomotor activity. This task is so complex that it would be a miracle if disturbances did not occur. The most important issue here is the close link between respiration and the postural function.
Skládal et al (1970) observed on radiographic images that the diaphragm became flatter and contracted when the patient stood on tiptoe during the exposure. They interpreted this as being a postural reaction, and drew the further conclusion that: ‘The diaphragm is a respiratory muscle with a postural function, and the abdominal muscles are postural muscles with a respiratory function.’
The way this is understood today is as follows: the
diaphragm attaches dorsally to the spinal column and laterally to the inferior costal arch, while ventrally the fixed point is provided by the abdominal wall. Here, the co-contraction of the deep layer of the abdominal muscles has a key role.
Kolář (2006) showed radiographically that the diaphragm was angled downward in the ventral to dorsal direction if the abdominal muscles were weak. If the abdominal muscles are functioning normally, contraction of the diaphragm during inhalation is accompanied by eccentric contraction of the deep abdominal muscles. This can be clearly palpated laterally above the iliac crest. The effect is not only to
enable the diaphragm to function in the most efficient way and, as shown by Kapandji (1974), to expand the thorax, but also to fix the thorax to the pelvis and so stabilize the lumbar spine. The activation of the abdominal muscles during inhalation was also described by Campbell (1978) and
Basmajian (1978).
Holding the breath (the Valsalva maneuver) reinforces this postural function.
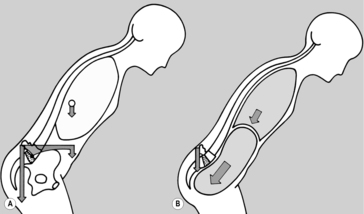
Morris et al (1961) showed that the spinal column is supported on the diaphragm when bending forward (see
Figure 2.19). Experience does indeed show that when we are about to lift a heavy weight using maximum force, or to perform a heavy blow or vigorous throw, we hold our breath. This is such an important mechanism that athletes hold their breath during demanding activity such as sprinting over short distances, sacrificing the respiratory to the postural function.
The most important faulty respiratory stereotype, seen from the point of view of the locomotor system, is that in which
the thorax is lifted during inhalation (
Parow 1954). In this pattern the thorax is lifted in the cranial direction by the scalene and sternocleidomastoid muscles and the superior fixator muscles of the shoulder girdle, but without expansion of the chest. Termed ‘clavicular breathing,’ it involves a reversal of the normal respiratory mechanism, since the scalene muscles, which normally only fix the thorax, raise the lung; resistance is offered by the diaphragm. This is inefficient, not only from the respiratory point of view, in that the volume of the chest increases very little, but also for the locomotor system, because of the chronic overload that this causes to the cervical spine.
A further effect is that fixation of the thorax to the pelvis no longer occurs, causing instability of the lumbar spine. The pattern of lifting the thorax during inhalation, or clavicular breathing, can be asymmetric, if one shoulder is raised more than the other. The stress on the cervical spine is then greater on this side. Clavicular breathing is the disturbance that typically occurs when sitting but not maintaining a straight posture, because this makes expansion of the thorax difficult.
An extreme form of this breathing pattern is paradoxical breathing, in which the patient draws in the abdomen during inspiration.
The effect of respiration is significant above all for the spinal column, which means that it can be employed to outstanding effect in neuromuscular techniques. As a general rule, muscle activity is facilitated during inhalation, and exhalation produces relaxation. The actual situation is a little more complicated: the abdominal muscles are facilitated during active exhalation, especially against resistance, and, as mentioned previously, raising the gaze of the eyes is associated with inhalation and lowering the gaze with exhalation.
It is appropriate at this point to explain the concept of ‘respiratory synkinesis,’ in which movement in one direction is linked with inhalation and in the other with exhalation. Where this is the case, it is difficult to do the reverse. Typical respiratory synkinesis can be observed during forward flexion of the trunk, and when straightening up from forward flexion. The fact that straightening up is usually associated with looking up, and forward flexion with looking down, makes clear why the initial act of looking up facilitates inhalation, and looking down, exhalation. Inhalation facilitates straightening up, not only from forward flexion, but also from side-bending. Side-bending itself is facilitated by looking down while exhaling.
Another very important example of respiratory synkinesis is the opening of the mouth during inhalation, and the closing of the mouth during exhalation. This facilitates first the masticatory muscles, and then in particular the digastric muscle. Inhalation facilitates kyphosis of the thoracic spine, and active exhalation lordosis of the thoracolumbar spine, especially in lordotic posture (
Lewit, Janda, Veverkova 1998). Resistance to traction of the cervical spine increases during inhalation; also during distraction of the hip. The resistance decreases during exhalation. Conversely, resistance increases in the lumbar spine on traction in the prone position, and decreases during inhalation. Clearly, then, these respiratory synkineses are extremely effective in mobilization and relaxation techniques for the spinal column.
One especially remarkable example of
synkinesis is that described by
Gaymans (1980) in the
cervical and thoracic spine. He found that, during side-bending, resistance increases in the even segments (in C0, C2, C4, and C6 and in T2, T4, T6, T8, and T10) during inhalation; it disappears during exhalation. Conversely, resistance increases in the odd segments (C1, C3, and C5 and T3, T5, T7, and T9) during exhalation, and disappears during inhalation. At the cervicothoracic junction, and only here, in the region between C6 and T2, resistance always increases during inhalation and decreases during exhalation. This synkinesis is so effective that during side-bending all that is needed is to take up the slack to the point of initial tension, then (in the case of an even-numbered segment) to ask the patient to inhale, and then to wait during the period of exhalation for mobilization to take place automatically. An exception to this rule is found in the atlanto-occipital segment; here this synkinesis operates not only in side-bending but in all directions. The phenomenon described here is so reliable that it can be used to correct the diagnosis as to the level of the vertebral segment. It is most marked at the cranial end of the spinal column and decreases somewhat in a caudal direction; in particular, the relaxation that accompanies exhalation diminishes in the lower thoracic spine. The reason for this may be connected with the fact that the thorax is stabilized during inhalation, and the diaphragm and quadratus lumborum as well as the deep layer of the abdominal muscles contract. We can therefore refer to inhalation–exhalation segments and exhalation–inhalation segments.
Marked respiratory synkinesis can also be found in trunk rotation; in the upright position, rotation of the trunk (including active rotation) increases during inhalation, while considerable resistance appears on exhalation. In a kyphotic sitting position, in contrast, resistance increases on inhalation and mobilization is therefore performed on exhalation.
Too little attention is paid to the effect of respiration on the locomotor system and vice versa. There is little awareness of the respiratory synkineses, and too little use is made of them by manual therapists, despite the fact that they are physiological methods. Empirically, many of these effects are employed in yoga; these include not only the effects on motor functions but also those on autonomic ones. This is understandable when we remember that respiration is the only ‘autonomic’ function on which we are able to exert any degree of direct influence voluntarily, that is using the voluntary muscles.
Rehabilitation focuses on faulty movement patterns, and their diagnosis and therapy will be explored in more detail in the relevant sections of this book. As we come to understand them, it becomes clear that the methods used in manual medicine, which are predominantly passive ones, are usually only lastingly effective if accompanied by the active participation of the patient.
Faulty muscle control originating from the central nervous system plays a significant part in the pathogenesis of dysfunctions of the locomotor system. Often, however, they are also a consequence of disturbances involving chronic pain. They, in turn, can then perpetuate and intensify the basic disturbance.
2.10. The significance of constitutional hypermobility
Movement restrictions, dealt with in the foregoing sections, are the true focus of manipulation therapy; however, the experienced clinician is well aware that hypermobility is frequently an even more difficult problem. The contributions made by
Sachse (1984,
Sachse et al 2004) have been fundamental in this area. The following categories can be distinguished:
• Localized pathological hypermobility. This may be primary or secondary (it is usually compensatory, occurring in the neighboring segment to a restricted joint). As such it is most frequently found in the spinal column.
• Generalized pathological hypermobility. This is most often found in certain congenital neurological conditions.
•
Constitutional hypermobility. This type is of the greatest interest to us. In essence it is a variant of the norm, but under certain conditions it can be significant for pathogenesis. As a general rule, mobility is greater in childhood than in adulthood, is greater in women than in men and, in the limbs, tends to be greater on the non-dominant side (
Sachse et al 2004).
There are conditions in which hypermobility may be an advantage, for instance in certain sports and in employment where mobility is a requirement. However, it involves the risk of decreased stability, and given the predominance of static load and overload in most occupations today, hypermobility is inappropriate. Individuals with constitutional hypermobility are at a particular disadvantage when working at a computer, as a driver, or in the majority of sedentary occupations, especially if the hypermobility is accompanied by laxity of the ligaments and weakness of the muscles. The situation is still more unfavorable if the hypermobility is accompanied by poor coordination and qualitatively poor movement patterns (Sachse 1984). The problem may even cross the boundary into minimal brain damage (MBD) as described by Janda (1978). In a study of 100 cases in which rehabilitation proved difficult, he distinguishes three types:
1. The first is ‘microspasticity,’ showing mild signs of first motor neuron lesion which is often asymmetrical.
2. The second is characterized by hypotonicity, with asymmetrical tendon and periosteal reflexes, signs of instability and restlessness, and – consistently with the account given by Sachse – severe hypermobility.
3. The third type shows disturbances of proprioception, which become more evident with eyes closed. This is expressed as a certain marked ‘clumsiness’ and accompanied by poor psychological adaptability, which makes rehabilitation more difficult.
Hypermobility in itself is no more than a constitutional characteristic; however, there is a tendency toward instability that is pathological. The most important role here is that played by the deep stabilization system.
So far we have dealt mainly with the locomotor system and dysfunctions of that system, in particular mechanical disturbances (
Figure 2.20).
The dynamic role – usually also the primary role – in the interplay between dysfunction and morphological change is that of function.
2.11. Reflex processes in vertebrogenic dysfunctions
Despite the importance of the mechanical factor for pathogenesis, it is not identical with clinical disease. Patients do not generally tend to complain of disturbances of mobility, but rather of pain, whether in the back, limbs, head, or viscera. They may even be suffering from considerable movement restrictions, yet they do not notice these. Examination may sometimes even reveal signs of nociceptive irritation (latent trigger points or hyperalgesic zones on the skin), yet the patient does not feel pain. The explanation lies in the capacity of the nervous system to react. We now need to know how it is that dysfunction produces pain.
Before presenting an explanation I should stress that it is not the purpose of this book to deal with the purely theoretical aspects of the pathogenesis of pain; we do however need to deal with the theoretical inferences that can be drawn from clinical diagnosis and therapy. Examination before and after therapy enables us to arrive at certain theoretical conclusions, as we might from an experiment, and the findings that are made after therapy not only show a normalization of mobility, but also a reduction of tension in the affected muscles, and that of the soft tissues. The effect is observed after manipulation, local anesthesia, needling, relaxation of trigger points, and massage. In each case, pain too is relieved. If the pain arises as a result of having to maintain an uncomfortable forced position, correction of the position is often enough to bring relief. The same is true of strenuous work; when we work beyond our strength we hardly notice it at first, but eventually pain forces it to our attention and we suspend the activity. After a short while the pain subsides.
The common denominator in all this is the close
connection between
tension and
pain in the locomotor system. Daily evidence of this is seen in the post-isometric relaxation of tense muscles; as the tension reduces, so the pain subsides, not only in the muscle itself but also in its attachments (see
Chapter 6).
Since the locomotor system is controlled by our will – and whim – it has no way of protecting itself other than by causing pain. In this way the voluntary activity of the locomotor system is kept within due bounds by pain. The
locomotor system is therefore by far the
most frequent source of pain in the human body; it is more than mere coincidence that referred pain from other organs or systems is perceived in the locomotor system, and that pain receptors are located in those places where tension in the locomotor system is expressed: in muscles, joint capsules, the attachments of tendons and ligaments, root sheaths, and the anulus fibrosus of intervertebral disks.
Pain is the most common symptom of dysfunction, and functional disturbances of the locomotor system are the most common cause of pain.
The close connection between physical and psychological factors in the production of pain is easy to understand: pain itself is both a physical and a psychological phenomenon. The same is true of tension and also, especially, of relaxation: it would be difficult to imagine psychological relaxation without relaxed muscles, or to imagine relaxing the muscles without being mentally relaxed. This close interrelationship is true for the locomotor system in general, since movement is the effect of voluntary motion that originates in the psyche.
Since movement is an outward effect of psychological activity, it is also true that psychological activity is a factor in motor function.
The nociceptive stimulus produces a reaction in the segment, and the intensity of the reaction can vary enormously. This is clinically significant, because it allows us to estimate the capacity for reaction in the individual case. This applies not only to autonomic reactions, but also to those of the muscles, whose response may take the form of TrPs or spasm. Korr’s concept of ‘segment facilitation’ is therefore appropriate here. There may be considerable differences between patients, and reactions may also vary considerably in the same individual under different circumstances. If, for instance, acute pain has been provoked by a draught, it should not simply be ascribed to the cold air alone, for in such patients we find restrictions in at least one segment, with severe muscle spasm. The restrictions are clinically latent, but produce a skin hyperalgesic zone (HAZ) in the segment. The cold draught striking this HAZ is an additional stimulus which intensifies the patient’s reaction and causes muscle spasm which makes the clinically latent lesions manifest.
It is a mistake to explain the pain as due to mechanical irritation of nerve fibers, as is frequently suggested. It would be a peculiar concept of the nervous system (a system whose purpose is to process information) that would have it reacting, not to stimulation of its receptors, but to mechanical damage to its own structures. Referred pain from the viscera is the typical model, or experimentally-induced referred pain from the infiltration of hypertonic saline solution into ligamentous structures of the spinal column, as performed by
Kellgren (1939) and later by
Feinstein et al (1954) and by
Hockaday & Whitty (1967) and in the zygapophysial cervical joints by
Pi’tha & Drobný (1972).
Just as in these model experiments, pain arising from deep structures (joints, muscles, ligaments, and internal organs) is referred, especially within the affected segment, and also gives rise to corresponding HAZs, sometimes even paresthesia, imitating radicular pain and so leading
Brügger (1962) to refer to it as ‘pseudoradicular.’ Other terms often used,
where there is a combination of pain in the muscles, tendons, and insertions, are ‘myotendinosis’ (Brügger 1962) or ‘myofascial pain’ (
Travell & Simons 1999).
The
soft-tissue changes, such as HAZs in the skin and subcutaneous tissue, have mainly been described as reflex changes or as secondary phenomena. This is usually true in acute cases where there is no long history, and these changes are generally found to subside when the joints and spinal column are treated. However, in the later, chronic stage, these changes – especially in fasciae and muscles – can become chronic; resistance is found in the fasciae, muscles become shortened, and chronic TrPs form. Some authors call this the ‘dystrophic stage’ (
Popelyanski 1983,
Popelyanski 1984). Pathological barriers are also present in such cases, however, and it is possible to achieve release. When dealing with chronic TrPs, this can be done by means of needling. In such cases, even these changes may turn out to be functional and reversible. Nevertheless it is important to note that where there are ‘sticky’ fasciae (which do not shift), shortened muscles, or chronic TrPs, these do not subside following manipulative treatment of joint restrictions. On the contrary, if they do not receive specific treatment, they can cause chronic recurrent restrictions.
The model described here has been that of characteristic painful disturbances within the segment. However, it should not be forgotten that the pain threshold, which is under central nervous control, is only crossed when the nociceptive stimulus has reached a particular intensity. Only then is it actually experienced as pain. So it is that, on careful examination, very frequently we find clinical changes when patients have no sense of pain at all.
It can therefore be seen that dysfunctions of the locomotor system produce
nociceptive stimulation whose effects are felt both suprasegmentally and also at the level of the central nervous system. The entire complex of function-related disturbance can be called the ‘functional pathology of the locomotor system.’
The complex of predominantly mechanical dysfunctions and reflex changes can be termed ‘functional pathology of the locomotor system.’
Unfortunately, so widespread is the lack of knowledge, often combined with skepticism, that the concept of ‘functional pathology’ is viewed as a kind of excuse for ignorance of the true causes or the true pathology in most cases of pain affecting the locomotor system and spinal column. Yet what other explanation is there for the fact that, following manipulation, not only does the pain cease, but mobility is restored to clinical normality and muscle TrPs and HAZs instantly disappear? These are not mere coincidence; careful clinical examination can predict the rapid appearance of the effect. If these were pathomorphological changes they would need to heal, and this requires time.
The situation can best be explained by comparing it to the working of a car: it may break down because of a burst cylinder or a damaged ball bearing (a pathomorphological change), but another reason for it to fail may be that the ignition is out of order, or the carburetor needs adjusting; the structure is intact, and the disorder is a functional, reversible one. Following a simple adjustment, the problem is instantly resolved.
One of the reasons for the failure to recognize that dysfunction is the most frequent cause of pain in the locomotor system is that the evidence is simply based on clinical findings, often relying on palpation, and this is rejected as ‘subjective.’ Connected to this we see a systematical underestimation of clinical diagnosis as a scientific discipline, and neglect accorded to it in practice. Much the same applies to the solving of the ‘puzzle of pain’ in dysfunctions of the locomotor system: pain is closely linked to tension and the release of tension to relief of pain, and the key to understanding this lies in palpation.
In differential diagnosis of conditions affecting the locomotor system, the fundamental distinction to be made is therefore between conditions due primarily to pathomorphological changes and those caused by dysfunction. Yet even where a morphological lesion is present, dysfunctions may still play a significant role and should be treated accordingly; rehabilitation is included here.
2.12. Radicular pain
The point having clearly been made that pain in the locomotor system is due to nociceptive stimulation of pain receptors, we must proceed to look at how and why
pain arises in cases of
root compression. The mechanical compression of a nerve does not itself cause pain but anesthesia, paresthesia, and paresis. However, we should bear in mind that the herniated disk causing the compression
cannot impinge on the nerve fibers until after it has affected the dura and the dural sheaths, which are richly supplied with pain receptors (Wyke 1980), and that with every movement of the legs and trunk the dura is being rubbed against the disk. Nor should it be forgotten that Lasègue’s sign indicates meningeal involvement, even in root compression syndromes. This is in keeping with the clinical course: first of all there is usually severe pain, and the signs of neurological deficit appear later. Other clinical observations support this.
Cerný (1948), using autodermography to study patients with radicular pain, found that this method was more reliable in localizing the disk herniation to the particular segment than the typical signs of neurological deficit. This can be understood anatomically in that spinal nerves do not contain fibers from one segment only; they also carry many transitory fibers from neighboring segments. As a result, the failure of a single spinal nerve does not usually lead to signs of deficit. There is an overlap of the areas of nerve roots.
Hanraets (1959), however, demonstrated that this is not always the case. He frequently found, during neurological surgery, that spinal nerves vary considerably in thickness: if one is very thick, its neighbor is likely to be much thinner, because of the number of transitory fibers in individual spinal nerves. If a thin spinal nerve is compressed or even severed, deficit will not be observed, because the transitory fibers in the neighboring nerve roots are able to compensate sufficiently, but if a thick root is severed, the consequences are quite different. Most thin neighboring roots have very few transitory fibers that can provide compensation. When
Hanraets (1959) stimulated such a spinal nerve during operation (at that time his operations were still being performed under local anesthetic), his patients also felt paresthesia in the neighboring segments.
Our own findings (1958), working together with Starý, are also consistent with this. We examined patients following intervertebral disk operations. At that time, in cases where no disk herniation was found, the neurosurgeon cut the sensory spinal nerve. Most of these patients experienced little effect, but some complained of permanent numbness and especially disturbances of proprioception following the procedure. In these cases a thick nerve root had evidently been cut, as described by
Hanraets (1959).
The pain resulting from irritation of dural receptors is referred pain, which corresponds precisely to the segment affected. It is this projection pain that is shown by Cerný’s autodermography. We can conclude that radicular pain is a combination of referred pain originating from dural receptors, and signs of neurological deficit. This explains why autodermography, in which patients themselves draw their projection pain, produces the most accurate clinical localization of a herniated disk.
There is yet another observation that points to a functional factor in root compression: this is the frequent immediate improvement of muscle strength in weak muscles and sometimes even of tendon reflexes, immediately after manipulation and even after traction. This has been demonstrated by electromyography (see
Figure 2.12 and
Figure 2.13), and also shown by the work of
Drechsler (1970) and
Hanák et al (1970). They showed that, even in true radicular syndromes with muscle weakness, the speed of nerve conduction may be normal. In the light of this they interpreted the weakness as reflex inhibition. Drechsler also concluded that decreased conduction speed indicates a poor clinical prognosis.
Radicular compression syndrome is a mixture of root compression and reflex phenomena. The decisive factor for localizing the cause of pain is referred pain produced by stimulation of receptors.
2.13. The term ‘vertebrogenic’
Once the terms ‘degenerative disease’ and ‘diskopathy’ had been abandoned as inappropriate, ‘vertebrogenic’ became widely adopted as a concept. It too is not quite appropriate: it includes pathological conditions such as ankylosing spondylitis, and does not cover dysfunctions that lie outside the spinal column. The term is therefore acceptable only if it is used as a pars pro toto. So long as it is used for back pain and very closely related disorders, there can be little objection to it; the term becomes controversial if the attempt is made to apply it to pain deriving from the internal organs, as might particularly tend to happen if treatment of the pain is successful.
As will be seen in further chapters, vertebrovisceral relations are very complex; the term ‘vertebrogenic’ should therefore be applied with caution. In many cases pathogenesis is due to more than one factor, and it is then better to speak of disease with a vertebrogenic factor. Migraine is a good example, since the true cause is unknown, although it is usually accompanied by findings in the locomotor system that do cause significant pain. We should reserve the term vertebrogenic for those conditions in which the spinal column (the locomotor system) is the decisive factor, for example when we describe a case of vertigo as vertebrogenic.
As Junghanns (1957) has pointed out, the role of the vertebrogenic factor may change over the course of time. It may trigger the disease process, but once this has started it may develop independently.
Gutzeit (1953) very aptly characterized the spinal column as being sometimes the ‘initiator,’ sometimes the ‘provoker,’ and in yet a third way as being the ‘multiplier’ of a disease state.
We should speak of vertebrogenic disturbance only when we wish to say that the spinal column is the primary and decisive factor in pathogenesis in a given case of disease.
2.14. Conclusions
• Morphological changes cannot explain pathogenesis in the great majority of painful conditions of the locomotor system. These changes often have the role of a locus minoris resistentiae.
• The most frequent cause of pain in the locomotor system is dysfunction, in a joint, muscle, soft tissue, body statics, or dynamics (the movement patterns or motor stereotypes).
• The most important cause of dysfunction is overload caused by overexertion, faulty movement patterns or body statics, trauma, or visceral disease. This includes joint restrictions, muscle TrPs, and soft tissue lesions, especially of fasciae and active scars. All these cause an increase in tension.
• When dysfunctions in the segment persist for a long time they eventually lead to degenerative (adaptive) changes, and do not remain confined to the segment concerned but affect the entire system.
• The locomotor system and the spinal column together make up a functional unit which has to compensate for any dysfunction, so that equilibrium is always maintained. In other words, the ‘motor program’ is reprogrammed. This gives rise to compensatory movement patterns, often designed to reduce pain. These can persist even when the primary cause is no longer present.
• Mechanical disturbance of function alone is insufficient to cause pain. However, it does represent a nociceptive stimulus which produces reflex changes, especially within the segment. If these are of sufficient intensity to pass the pain threshold, they are experienced as pain. The specific nociceptive stimulus in the case of dysfunctions is understood to be increased tension.
• Pain in the locomotor system is primarily a warning signal of harmful functioning, which should cause us to correct this before it causes permanent morphological damage. It is the type of pain that occurs most frequently in the human body.
• If the patient is able to describe and localize the pain, and if on clinical examination we find corresponding changes, above all reflex signs, then the diagnosis (once we have excluded gross pathology) must be the relevant dysfunction. Undiagnosed dysfunctions are the most frequent cause of pain in the locomotor system, and treatment which is directed only at the symptom of pain, without a thorough understanding and analysis of the dysfunction causing that pain, will be frustrating and ineffective.
• The complex of changes in function of the locomotor system and the reflex effects caused by these changes constitute what may be called the ‘functional pathology of the locomotor system.’