Chapter 1 Ethics, law and communication
Ethics and the law
Ethics: an introduction
Ethical practice: sources, resources and approaches
To engage with an ethical issue in clinical practice depends on:
Ethical theories and frameworks
Key ethical theories are summarized in Box 1.1.
![]() Box 1.1
Box 1.1
Key ethical theories
Deontology: a universally applicable rule or duty-based approach to morality, e.g. a deontologist would argue that one should always tell truth irrespective of the consequences.
Consequentialism: an approach that argues that morality is located in consequences. Such an approach will focus on likely risks and benefits.
Virtue ethics: offers an approach in which particular traits or behaviours are identified as desirable.
Rights theory: assesses morality with reference to the justified claims of others. Rights are either ‘natural’ and arise from being human, or legal, and therefore enforceable in court. Positive rights impose a duty on another to act whilst negative rights prohibit interference by others.
Narrative ethics: an approach that argues morality is embedded in the stories shared between patient and clinician and allows for multiple perspectives.
1. Autonomy: to allow ‘self-rule’, i.e. let patients make their own choices and to decide what happens to them
2. Beneficence: to do good, i.e. act in a patient’s best interests
The law
As it pertains to medicine, the law establishes boundaries for what is deemed to be acceptable professional practice. The law that applies to medicine is both national and international, e.g. the European Convention on Human Rights (Box 1.2). Within the UK, along with other jurisdictions, both statutes and common law apply to the practice of medicine (Box 1.3).
![]() Box 1.2
Box 1.2
European Convention on Human Rights
Substantive rights which apply to evaluating good medical practice
 Prohibition of torture, inhuman or degrading treatment or punishment (Article 3)
Prohibition of torture, inhuman or degrading treatment or punishment (Article 3)
 Prohibition of slavery and forced labour (Article 4)
Prohibition of slavery and forced labour (Article 4)
 Right to liberty and security (Article 5)
Right to liberty and security (Article 5)
 Right to a fair trial (Article 6)
Right to a fair trial (Article 6)
 No punishment without law (Article 7)
No punishment without law (Article 7)
 Right to respect for private and family life (Article 8)
Right to respect for private and family life (Article 8)
 Freedom of thought, conscience and religion (Article 9)
Freedom of thought, conscience and religion (Article 9)
![]() Box 1.3
Box 1.3
Statutes and common law
Statutes
 Primary legislation made by the state, e.g. Acts of Parliament in the UK, such as the Mental Capacity Act 2005
Primary legislation made by the state, e.g. Acts of Parliament in the UK, such as the Mental Capacity Act 2005
 Secondary (or delegated) legislation: supplementary law made by an authority given the power to do so by the primary legislation
Secondary (or delegated) legislation: supplementary law made by an authority given the power to do so by the primary legislation
 Implementation (or statutory) guidance, e.g. the Mental Health Act Code of Practice
Implementation (or statutory) guidance, e.g. the Mental Health Act Code of Practice
Respect for autonomy: capacity and consent
Capacity
Capacity is at the heart of ethical decision-making because it is the gateway to self-determination (Box 1.4). People are able to make choices only if they have capacity. The assessment of capacity is a significant undertaking: a patient’s freedom to choose depends on it. If a person lacks capacity, it is meaningless to seek consent. In the UK, the Mental Capacity Act 2005 sets out the criteria for assessing whether a person has the capacity to make a decision (see Ch. 23, p. 1191).
![]() Box 1.4
Box 1.4
Principles of self-determinationa
 Every adult has the right to make his/her own decisions and to be assumed to have capacity unless proved otherwise.
Every adult has the right to make his/her own decisions and to be assumed to have capacity unless proved otherwise.
 Everyone should be encouraged and enabled to make his/her own decisions, or to participate as fully as possible in decision-making.
Everyone should be encouraged and enabled to make his/her own decisions, or to participate as fully as possible in decision-making.
 Individuals have the right to make eccentric or unwise decisions.
Individuals have the right to make eccentric or unwise decisions.
 Proxy decisions should consider best interests, prioritizing what the patient would have wanted, and should be the ‘least restrictive of basic rights and freedoms’.
Proxy decisions should consider best interests, prioritizing what the patient would have wanted, and should be the ‘least restrictive of basic rights and freedoms’.
Consent
 given by a patient who has capacity to make a choice about his or her care
given by a patient who has capacity to make a choice about his or her care
 voluntary, i.e. free from undue pressure, coercion or persuasion
voluntary, i.e. free from undue pressure, coercion or persuasion
 continuing, i.e. patients should know that they can change their mind at any time.
continuing, i.e. patients should know that they can change their mind at any time.
The basis of informed consent
Advance decisions
 based on appropriate information
based on appropriate information
 specific and applicable to the situation in which it is being considered.
specific and applicable to the situation in which it is being considered.
Best interests of patients who lack capacity
Provision or cessation of life-sustaining treatment
 Based on good evidence, the team believes that further treatment will not save life
Based on good evidence, the team believes that further treatment will not save life
 The patient is already imminently and irreversibly close to death
The patient is already imminently and irreversibly close to death
 The patient is so permanently or irreversibly brain damaged that he or she will always be incapable of any future self-directed activity or intentional social interaction.
The patient is so permanently or irreversibly brain damaged that he or she will always be incapable of any future self-directed activity or intentional social interaction.
Assisted dying
Currently in many countries, there is no provision for lawful assisted dying. For example, physician-assisted suicide, active euthanasia and suicide pacts are all illegal in the UK. In contrast, some jurisdictions, including the Netherlands, Switzerland, Belgium and certain states in the USA, permit assisted dying. However, even where assisted dying is not lawful, withholding and withdrawing treatment is usually acceptable in strictly defined circumstances, where the intention of the clinician is to minimize suffering, not to cause death. Similarly, the doctrine of double effect may apply. It enables clinicians to prescribe medication that has as its principal aim, the reduction of suffering by providing analgesic relief but which is acknowledged to have side-effects such as the depression of respiratory effort (e.g. opiates). Such prescribing is justifiable on the basis that the intention is benign and the side-effects, whilst foreseen, are not intended to be the primary aim of treatment. End-of-life care pathways, which provide for such approaches where necessary, are discussed in Chapter 10.
FURTHER READING
British Medical Association. Assisted Suicide: Guidance for Doctors in England, Wales and Northern Ireland. London: BMA; 2010.
General Medical Council. Treatment and Care Towards the End of Life. London: GMC; 2010.
IMCA. Making Decisions: The Independent Mental Capacity Advocate (IMCA) Service. London: Department of Health; 2009.
UKHL. R (Purdy) v Director of Public Prosecutions [2009] UKHL 45.
Consent and children
 The patient, although under 16, can understand medical information sufficiently
The patient, although under 16, can understand medical information sufficiently
 The doctor cannot persuade the patient to inform, or give permission for the doctor to inform, his or her parents
The doctor cannot persuade the patient to inform, or give permission for the doctor to inform, his or her parents
 In cases where a minor is seeking contraception, the patient is very likely to have sexual intercourse with or without adequate contraception
In cases where a minor is seeking contraception, the patient is very likely to have sexual intercourse with or without adequate contraception
 The patient’s mental or physical health (or both) are likely to suffer if treatment is not provided
The patient’s mental or physical health (or both) are likely to suffer if treatment is not provided
 It is in the patient’s best interests for the doctor to treat without parental consent.
It is in the patient’s best interests for the doctor to treat without parental consent.
Confidentiality
When confidentiality must or may be breached
The duty of confidence is not absolute. Sometimes, the law requires that clinicians must reveal private information about patients to others, even if they wish it were otherwise (Box 1.5). There are also circumstances in which a doctor has the discretion to share confidential information within defined terms. Such circumstances highlight the ethical tension between the rights of individuals and the public interest.
1. The patient has given consent.
2. It is in the patient’s best interests to share the information but it is impracticable or unreasonable to seek consent.
Resource allocation
Fairness
Professional competence and mistakes
Clinical negligence
Clinical negligence remains relatively rare and undue fear of litigation can lead to defensive and poor practice. All doctors make errors and these do not necessarily constitute negligence or indicate incompetence. Inherent in the definition of incompetence is time, i.e. on-going review of a doctor’s practice to see whether there are patterns of error or repeated failure to learn from error. Regulatory bodies and medical defence organizations recommend that doctors should be honest and apologetic about their mistakes, remembering that to do so is not necessarily an admission of negligence (see p. 14). Such honesty and humility, aside from its inherent moral value, has been shown to reduce the prospect of patient complaints or litigation.
Policy
The issue of professional accountability in medicine is a hot topic. The law, professional guidance and policy documentation provide a starting point for clinicians. Complaints and possible litigation are often brought by patients who feel aggrieved for reasons that may be unconnected with the clinical care that they have received. When patients are asked about their decisions to complain or to sue doctors, it is common for poor communication, insensitivity, administrative errors and lack of responsiveness to be cited as motivation (see p. 7). There is less to fear than doctors sometimes believe. The courts and professional bodies are neither concerned with best practice, nor with unfeasibly high standards of care. What is expected is that doctors behave in a way that accords with the practice of a reasonable doctor – and the reasonable doctor is not perfect. As long as clinicians adhere to some basic principles, it is possible to practise defensible rather than defensive medicine. It should be reassuring that complaints and litigation are avoidable, simply by developing and maintaining good standards of communication, organization and administration – and good habits begin in medical school. In particular, effective communication is a potent weapon in preventing complaints and, ultimately, encounters with the legal and regulatory systems.
Communication
Communication in healthcare
What is patient-centred communication?
Patient-centred communication involves reaching a common ground about the illness, its treatment, and the roles that the clinician and the patient will assume (Fig. 1.1). It means discovering and connecting both the biomedical facts of the patient’s illness in detail and the patient’s ideas, concerns, expectations and feelings. This information is essential for diagnosis and appropriate management and also to gain the patient’s confidence, trust and involvement.
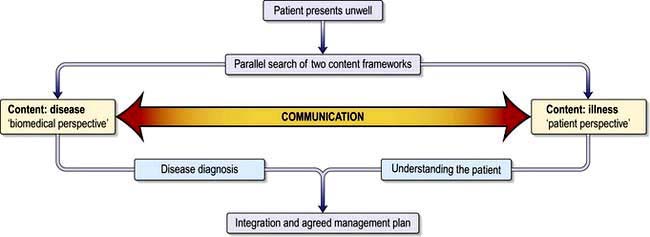
Figure 1.1 The patient-centred clinical interview.
(Adapted from: Levenstein JH. In: Stewart M, Roter D, eds. Communicating with Medical Patients. Thousand Oaks, CA: Sage; 1989, with permission.)
 Patients increasingly expect information about their condition and treatment options and want their views taken into account in deciding treatment. This does not mean clinicians totally abdicate power. Patients want their doctors’ opinions and expertise and may still prefer to leave matters to the clinician.
Patients increasingly expect information about their condition and treatment options and want their views taken into account in deciding treatment. This does not mean clinicians totally abdicate power. Patients want their doctors’ opinions and expertise and may still prefer to leave matters to the clinician.
 Many health problems are long-term conditions and patients may become experts actively involved in self-care. They have to manage their conditions and reduce risks from lifestyle habits in a partnership approach to care.
Many health problems are long-term conditions and patients may become experts actively involved in self-care. They have to manage their conditions and reduce risks from lifestyle habits in a partnership approach to care.
 A distinguishing feature of the healthcare professions is that patients expect humanity and empathy from their doctors as well as competence. Clinicians can usually offer practical help with patients’ concerns and expectations but, if not, they can always listen supportively.
A distinguishing feature of the healthcare professions is that patients expect humanity and empathy from their doctors as well as competence. Clinicians can usually offer practical help with patients’ concerns and expectations but, if not, they can always listen supportively.
Patient-centred communication requires a good balance between:
What are the effects of communication?
Enormous benefits accrue from good communication (Box 1.6). Patients’ problems are identified more accurately and efficiently, expectations for care are agreed and patients and clinicians experience greater satisfaction. Poor communication results in missed problems (Box 1.7) and concerns, strained relationships, complaints and litigation.
![]() Box 1.7
Box 1.7
Patient reports of failure to identify problems in interviews
 54% of complaints and 45% of concerns were not elicited
54% of complaints and 45% of concerns were not elicited
 50% of psychological problems not elicited
50% of psychological problems not elicited
 80% of breast cancer patients’ concerns remain undisclosed
80% of breast cancer patients’ concerns remain undisclosed
 In 50% of visits, patients and doctors disagreed on the main presenting problem
In 50% of visits, patients and doctors disagreed on the main presenting problem
 In 50% of cases, patient’s history was blocked by interruption within 24 seconds
In 50% of cases, patient’s history was blocked by interruption within 24 seconds
From: Simpson M, Buckman R, Stewart M et al. The Toronto Consensus Statement. British Medical Journal 1991; 303:1385–1387, with permission.
Adherence to treatment
Some 45% of patients are not following treatment advice properly. Errors in use of medications are costly and risk patient safety. Patients may not understand or remember what they were told, whilst others actively decide not to follow advice and commonly do not tell their doctors. Research shows that clinicians rarely check patients’ understanding or views, yet such communication contributes to adherence (Practical Box 1.1).
Patient satisfaction and dissatisfaction
Satisfaction with consultations is largely a result of patients knowing they are:
Satisfaction with a consultation affects psychological wellbeing and adherence to treatment, both of which have a knock-on effect on clinical outcomes. It also reduces patient complaints and litigation (Box 1.8). Some 70% of lawsuits are a result of poor communication rather than failures of biomedical practice. Complaints and lawsuits represent only the tip of the iceberg of discontent, as revealed by surveys of patients in hospital and primary care.
Barriers and difficulties in communication
Communication is not straightforward (Box 1.9). Time constraints can prevent both doctors and patients from feeling that they have each other’s attention and that they fully understand the problem from each other’s perspective. Underestimation of the influence of psychosocial issues on illness and their costs to healthcare means clinicians may resort to avoidance strategies when they fear the discussion will unleash emotions too difficult to handle, upset the patient or take too much time (Box 1.10).
![]() Box 1.9
Box 1.9
Common barriers and difficulties in communication
| Clinician factors | Shared factors | Patient factors |
|---|---|---|
![]() Box 1.10
Box 1.10
Strategies that doctors use to distance themselves from patients’ worries
| Patient says: ‘I have this headache and I’m worried …’ | |
|---|---|
|
Selective attention to cues |
‘What is the pain like?’ |
|
Normalizing |
‘It’s normal to worry. Where is the pain?’ |
|
Premature reassurance |
’Don’t worry. I’m sure you’ll be fine’ |
|
False reassurance |
‘Everything is OK’ |
|
Switching topic |
‘Forget that. Tell me about …’ |
|
Passing the buck |
‘Nurse will tell you about that’ |
|
Jollying along |
‘Come on now, look on the bright side’ |
|
Physical avoidance |
Passing the bedside without stopping |
From Maguire P. Communication Skills for Doctors. London: Arnold; 2000, with permission.
FURTHER READING
Ambady N, LaPlante D, Nguyen T et al. Surgeon’s tone of voice: a clue to malpractice history. Surgery 2002; 132(1):5–9.
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ 2007; 335:24–27.
Margalit A, El-Ad A. Costly patients with unexplained medical symptoms. A high-risk population. Patient Educ Couns 2008; 70:173–178.
The medical interview
Structure and skills for effective interviewing
There are seven essential steps in the medical interview:
3. Gathering information
The components of a complete history are shown in Table 1.1.
Questioning styles
The way a clinician asks questions determines whether the patient speaks freely or just gives one word or brief answers (Practical Box 1.2). Start with open questions (‘What problems have brought you in today?’) and move to screening (‘Is there anything else?’), focused (‘Can you tell me more about the pain?’) and closed questions (‘Where is the pain?’). Open methods allow clinicians to listen and to generate their problem-solving approach. Closed questions are necessary to check specific symptoms but if used too early, they may narrow down and lead to inaccuracies by missing patients’ problems.
![]() Practical Box 1.2
Practical Box 1.2
Questioning style
Closed questioning style
Open questioning style
Doctor: ‘Tell me about the pain you’ve been having.’ (open/focused Q)
Patient: ‘Well it’s been getting worse over the past few weeks and waking me up at night. It’s just here (points to sternum), it’s very sharp and I get a burning and bad acid taste in the back of my throat. I try to burp to clear it. I’ve taken antacids but they don’t seem to be helping now and I’m a bit worried about it. I’m losing sleep and I’ve got a busy workload so that’s a worry too.’
Doctor: ‘I see. So it’s bothering you quite a lot. Anything else you’ve noticed?’ (empathic statement, open screening Q)
Patient: ‘I’ve noticed I get it more after I’ve had a few drinks. I have been drinking and smoking a bit more recently. Actually I’ve been getting lots of headaches too which I’ve just taken Ibuprofen for.’
Doctor: ‘You say you are worried, is there anything in particular that concerns you?’ (picks up on patient’s cue and uses reflecting question)
Patient: ‘I wondered if I might be getting an ulcer.’
Doctor: ‘I see. So this sharp pain under your breastbone with some acid reflux for several weeks is worse at night and aggravated by drinking and smoking but not relieved by antacids. You are busy at work, getting headaches, drinking and smoking a bit more and not sleeping well. You’re concerned this could be an ulcer.’ (summarizing)
Patient: ‘Yes, a friend had problems like this.’
Doctor: ‘I can appreciate why you might be thinking that then.’ (validation)
Patient: ‘Yes and he had to have a “scope” so I wondered whether I would need one?’(expectation)
Doctor: ‘Well, let me explain first what I think this is and then what I would recommend next …’ (signposting)
4. Understanding the patient
Finding out the patient’s perspective is an essential step towards achieving common ground.
Ideas, concerns and expectations (ICE)
 ‘What were you worried this might be?’
‘What were you worried this might be?’
 ‘Are there any particular concerns you have about …?’
‘Are there any particular concerns you have about …?’
 ‘Was there anything you were hoping we might do about this?’
‘Was there anything you were hoping we might do about this?’
Hearing patients’ ideas, acknowledging their concerns and empathizing, are essential steps in engaging a patient’s trust, and beginning to ‘treat the whole patient’. The example in Practical Box 1.2 also shows how information that may be biomedically relevant emerges while listening to patients.
5. Sharing information
 Information must be related not only to the biomedical facts, but tailored to patients’ ideas and concerns.
Information must be related not only to the biomedical facts, but tailored to patients’ ideas and concerns.
 Most patients want to be fully informed, irrespective of socioeconomic group.
Most patients want to be fully informed, irrespective of socioeconomic group.
 Most patients of all ages will understand and recall 70–80% of even the most unfamiliar, complex or alarming information if given along the guidelines shown in Practical Box 1.3.
Most patients of all ages will understand and recall 70–80% of even the most unfamiliar, complex or alarming information if given along the guidelines shown in Practical Box 1.3.
![]() Practical Box 1.3 Giving information
Practical Box 1.3 Giving information
The 3E Model: Explore, Explain, Explore
Explain
Chunk and check. Give information in assimilable chunks, one thing at a time. Check after each chunk that the patient is understanding.
Signpost. ‘I’ll explain first of all …’; ‘Can I move on now to explain treatment options …?’
Link. Explain the cause and effect of the condition in the context of the patient’s symptoms, e.g. ‘The reason you are experiencing … is because …’
Plain language. Clear, concise language; translate any unavoidable medical terms and write them down.
Aid recall. Simple diagrams, leaflets, recommend websites and support organizations.
6. Reaching agreement on management
Clinical records
All medical interviews should be well documented. Good records are the responsibility of everyone in the healthcare team (Table 1.2), as is maintenance of confidentiality. They are vital in providing best care, reducing error and ensuring patient safety.
|
Records should include: |
aGMC Good Medical Practice 2012. bMPS Guide to Medical Records 2010; http://www.medicalprotection.org/uk/booklets/medical-records.
Team communication
Frameworks such as SBAR (Situation–Background–Assessment–Recommendation) use standardized prompt questions in four sections to ensure team members share concise and focused information at the correct level of detail (Box 1.11). This increases patient safety.
A – Assessment
R – Recommendation (examples)
FURTHER READING
BMA. Safe Handover: Safe Patients. Guidance on Clinical Handover for Clinicians and Managers. London: British Medical Association 2009; http://www.bma.org.uk/employmentandcontracts/working_arrangements/Handover.jsp.
SBAR (Situation–Background–Assessment–Recommendation) films at: http://www.institute.nhs.uk/safer_care/safer_care/sbar_escalation_films.html.
Communicating in difficult situations
Breaking bad news
 usually know more than anyone realizes and may imagine things worse than they are
usually know more than anyone realizes and may imagine things worse than they are
 appreciate clear information even about the worst news and want the opportunity to talk openly and ask questions, rather than join in a charade of deception
appreciate clear information even about the worst news and want the opportunity to talk openly and ask questions, rather than join in a charade of deception
A framework: the S–P–I–K–E–S strategy
S – Setting
 See the patient as soon as the current information has been gathered.
See the patient as soon as the current information has been gathered.
 Ask not to be disturbed and hand bleeps to colleagues.
Ask not to be disturbed and hand bleeps to colleagues.
 If possible, the patient should have someone with them.
If possible, the patient should have someone with them.
 Choose a quiet place with everyone seated and introduce everyone.
Choose a quiet place with everyone seated and introduce everyone.
 Indicate your status, extent of your responsibility toward the patient and the time available.
Indicate your status, extent of your responsibility toward the patient and the time available.
K – Knowledge
If the patient wishes to know:
 Give a warning to help the patient prepare: ‘I’m afraid it looks more serious than we hoped.’
Give a warning to help the patient prepare: ‘I’m afraid it looks more serious than we hoped.’
 At this point, WAIT: allow the patient to think, and only continue when the patient gives some lead to follow. This pause may be a long one, commonly a matter of minutes, but useful to help patients take in the situation. Patients may shut down and be unable to hear anything further until their thoughts settle down.
At this point, WAIT: allow the patient to think, and only continue when the patient gives some lead to follow. This pause may be a long one, commonly a matter of minutes, but useful to help patients take in the situation. Patients may shut down and be unable to hear anything further until their thoughts settle down.
 Give direct information, in small chunks. Avoid technical terms. Check understanding frequently: ‘Is this making sense so far?’ before moving on. Watch for signs the patient can take no more.
Give direct information, in small chunks. Avoid technical terms. Check understanding frequently: ‘Is this making sense so far?’ before moving on. Watch for signs the patient can take no more.
 Emphasize which things, for example pain and other symptoms, are fixable and which others are not.
Emphasize which things, for example pain and other symptoms, are fixable and which others are not.
 Be prepared for the question: ‘How long have I got?’ Avoid providing a figure to an individual, which is bound to be inaccurate. Common faults are to be overly optimistic. Some patients wish to know survival rates for their condition. Tell them as much as is appropriate. Stress the importance of ensuring that the quality of life is made as good as possible from day to day.
Be prepared for the question: ‘How long have I got?’ Avoid providing a figure to an individual, which is bound to be inaccurate. Common faults are to be overly optimistic. Some patients wish to know survival rates for their condition. Tell them as much as is appropriate. Stress the importance of ensuring that the quality of life is made as good as possible from day to day.
 Provide some positive information and hope, tempered with realism.
Provide some positive information and hope, tempered with realism.
E – Empathy
Responding to the patient’s emotions is about the human side of medical care and also helps patients to take in and adjust to difficult information. A range of emotions are experienced in seriously and terminally ill patients (Box 1.12).
 Be prepared for the patient to have disorderly emotional responses of some kind. Acknowledge them early on as being what you expect and understand and wait for them to settle before continuing.
Be prepared for the patient to have disorderly emotional responses of some kind. Acknowledge them early on as being what you expect and understand and wait for them to settle before continuing.
 Crying can be a release for some patients. Allow time if the patient needs it, rather than rushing in to stop the crying.
Crying can be a release for some patients. Allow time if the patient needs it, rather than rushing in to stop the crying.
 Learn to judge which patients wish to be touched and which do not. You can always reach out and touch their chair.
Learn to judge which patients wish to be touched and which do not. You can always reach out and touch their chair.
 Keep pausing to allow patients to think and frame their questions.
Keep pausing to allow patients to think and frame their questions.
 Watch for shutdown: stop the interview if necessary and arrange to resume later.
Watch for shutdown: stop the interview if necessary and arrange to resume later.
S – Strategy and summary
 The patient has understood what has been discussed because at times of emotion, misconceptions can take root
The patient has understood what has been discussed because at times of emotion, misconceptions can take root
 Crucial information is written down to take away
Crucial information is written down to take away
 The patient knows how to contact the appropriate team member and thus has a safety net in place; when the next appointment is (preferably soon), who it is with and its purpose
The patient knows how to contact the appropriate team member and thus has a safety net in place; when the next appointment is (preferably soon), who it is with and its purpose
 Family members are invited to meet the clinicians as the patient wishes and further sources of information are provided
Family members are invited to meet the clinicians as the patient wishes and further sources of information are provided
FURTHER READING
Lloyd M, Bor R. Communication Skills in Medicine, 3rd edn. Edinburgh: Churchill Livingstone; 2009.
Silverman J, Kurtz Z, Draper J. The Calgary-Cambridge guide: a guide to the medical interview. In: Skills for Communicating with Patients, 2nd edn. Abingdon: Radcliffe Medical Press; 2005, at: http://www.skillscascade.com/index.html.
FURTHER READING
Baile WF, Lenzi R, Kudelka AP et al. SPIKES – a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 2000; 5:302–311.
Chaturvedi SK. Truth telling and communication skills. Indian J Psychiatry 2009; 51:227.
Cheng SY, Hu WY, Liu WJ. Good death study of elderly patients with terminal cancer in Taiwan. Palliat Medic 2008; 22:626–632.
Clayton JM, Hancock K, Parker S et al. Sustaining hope when communicating with terminally ill patients and their families: a systematic review. Psychooncology 2008; 17:641–659.
When things go wrong
Complaints
The majority of complaints come from the exasperation of patients who:
 feel deserted and devalued by their clinician
feel deserted and devalued by their clinician
 have not been able to get clear information
have not been able to get clear information
 feel that they are owed an apology
feel that they are owed an apology
 are concerned that other patients will go through what they have.
are concerned that other patients will go through what they have.
Many complaints are resolved satisfactorily once these points are dealt with promptly and appropriately (Practical Box 1.4).
![]() Practical Box 1.4
Practical Box 1.4
Responding to complaints
 Remember the complainant is still a patient to whom there is a duty of care
Remember the complainant is still a patient to whom there is a duty of care
 Listen and express regret for distress
Listen and express regret for distress
 Acknowledge when things have gone wrong – be objective, not resentful or defensive
Acknowledge when things have gone wrong – be objective, not resentful or defensive
 Apologize for actual or perceived shortcomings
Apologize for actual or perceived shortcomings
 Provide easily understood information or explanations
Provide easily understood information or explanations
Lawsuits
FURTHER READING
National Patient Safety Agency. Being Open; Communicating Patient Safety Incidents with Patients, Their Families and Carers; 2009.
The Parliamentary and Health Service Ombudsman. Principles of Good Complaint Handling. London: HMSO; 2008.
World Health Organization. Patient Safety: Curriculum Guide for Medical Schools. Topic 8. Engaging with patients and carers. WHO; 2009:183–199.
Culture and communication
Non-verbal communication
Patients may be more or less traditional, so check out assumptions.
FURTHER READING
Cancer Research UK; http://info.cancerresearchuk.org/proceed/.
Kai J. Valuing Diversity: A resource for health professional training to respond to cultural diversity. London: Royal College of General Practitioners; 2006.
Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns 2006; 64(1–3):21–34.
Traylor AH, Schmittdiel JA, Uratsu CS et al. The predictors of patient-physician race and ethnic concordance: a medical facility fixed-effects approach. Health Serv Res 2010; 45:792–805.
Patients who have impaired faculties for communication
Impaired hearing
Some 55% of people over 60 are deaf or hard of hearing. Patients may be accompanied by a signer but less than 1% of hearing-impaired people sign. Many hard of hearing people lip-read and some commonsense tips are listed in Practical Box 1.5. Clinicians who mumble, speak fast or have strong accents have a responsibility to make particular efforts to be understood.
Impaired vision
Patients who have visual impairment can miss non-verbal cues in communication. It may sound obvious, but it helps to make more conscious efforts to use the patient’s name so they know they are being spoken to. Clinicians should avoid sudden touch, explain what they are about to do and say what they are doing as they go along. Large print information sheets should be available for those with limited vision; audiotapes, Braille and Moon versions for blind people (http://www.rnib.org.uk).
Recent influences on communication
The internet
Decision aids
Weighing up treatment benefits and risks where both may be substantial but not guaranteed is very hard for patients. Decision aids which are evidence-based, written in non-technical language and often including visual representations help people digest complex statistical information. They are reliable and from independent sources. Formats include web applications, DVDs, computer programs, leaflets and structured counseling. They are growing in number, with over 400 listed on the Cochrane register (see, e.g. http://www.ohri.ca/decisionaid).
Training in communication skills
FURTHER READING
Broom A. Virtually he@lthy: the impact of internet use on disease experience and the doctor-patient relationship. Qual Health Res 2005; 15:325–345.
Coulter A, Collins A. Making shared decision-making a reality. No decision about me without me. London: The King’s Fund; 2011.
McMullan M. Patients using the Internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns 2006; 63(1–2):24–28.
O’Connor AM, Stacey D, Entwhistle V et al. Decision aids for people facing health treatment or screening decisions (Cochrane Review). Chichester: The Cochrane Library 2005; (4).
Wilkinson S, Perry R, Blanchard K et al. Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med 2008; 22:365–375.
British Medical Association ethics
European Association for Communication in Healthcare


























































































































