CHAPTER 5 Esophageal Atresia with Tracheoesophageal Fistula
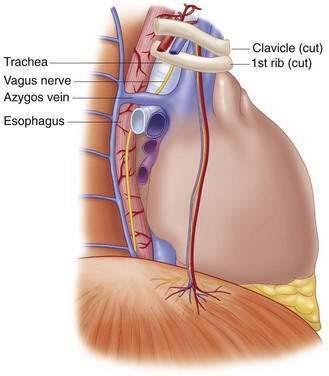
Step 1: Surgical Anatomy
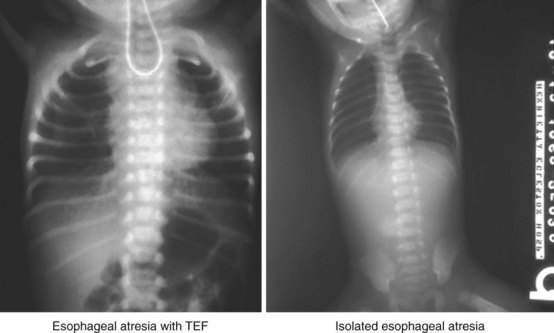
Step 2: Preoperative Considerations
 Cardiac: Echocardiogram to evaluate cardiac anatomy as well as identify position of the aortic arch. Surgical approach through the right or the left side of the chest is determined by the side of the aortic arch. In general, the arch is on the left and access for repair is through the right side of the chest.
Cardiac: Echocardiogram to evaluate cardiac anatomy as well as identify position of the aortic arch. Surgical approach through the right or the left side of the chest is determined by the side of the aortic arch. In general, the arch is on the left and access for repair is through the right side of the chest.Step 3: Operative Steps
Anesthetic Considerations
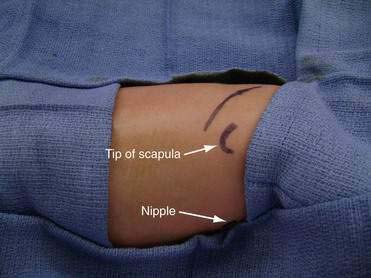
Positioning
Incision and Access
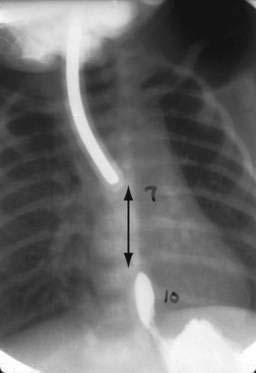
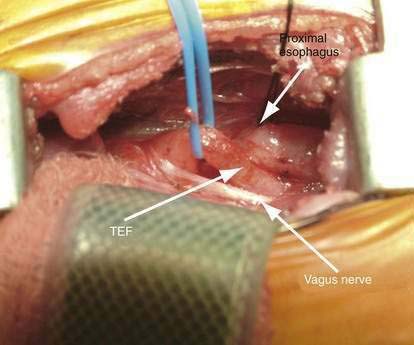
Division of the TEF and Mobilization of the Esophagus
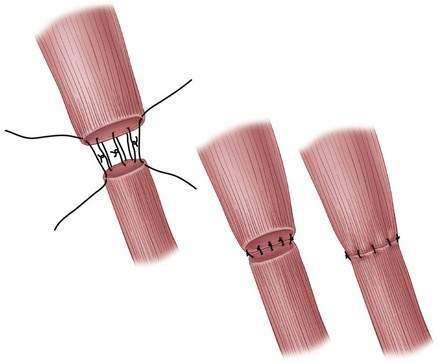
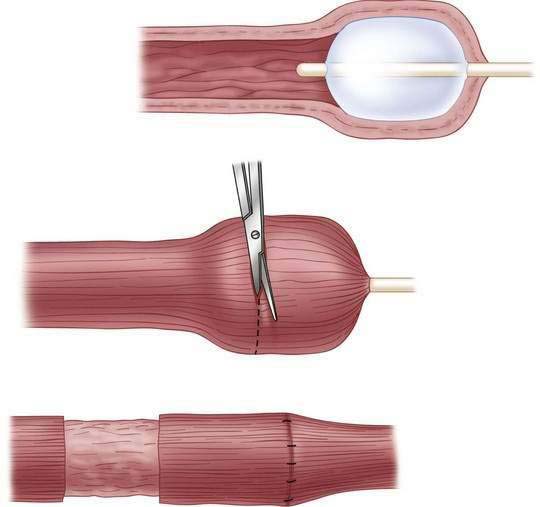
Anastomosis (Fig. 5-8)
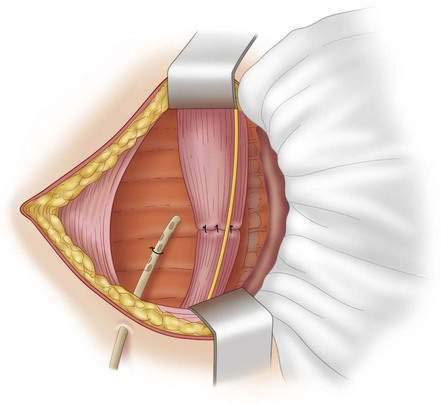
Closing
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Foker JE, Kendall TC, Carlton K, et al. A flexible approach to achieve a true primary repair for all infants with esophageal atresia. Semin Pediatr Surg. 2005;14:8-15.
Morrow SE, Ashcraft KW. Esophageal atresia. In: Ziegler MM, Azizkhan RG, Weber TR, editors. Operative pediatric surgery. New York: McGraw-Hill; 2003:349-354.
Raffensperger JG. Esophageal atresia and tracheoesophageal stenosis. In: Raffensperger JG, editor. Swenson’s pediatric surgery. 5th ed. Norwalk, CT: Appleton and Lange; 1990:697-717.
Ricketts RR, Luck SR, Raffensperger JG. Circular esophagomyotomy for primary repair of long-gap esophageal atresia. J Pediatr Surg. 1981;16:365-369.
Schwartz MZ. An improved technique for circular myotomy in long-gap esophageal atresia. J Pediatr Surg. 1983;18:833-834.