Chapter 22 Epineurial Suture, Split, and Graft Repair
Epineurial Suture
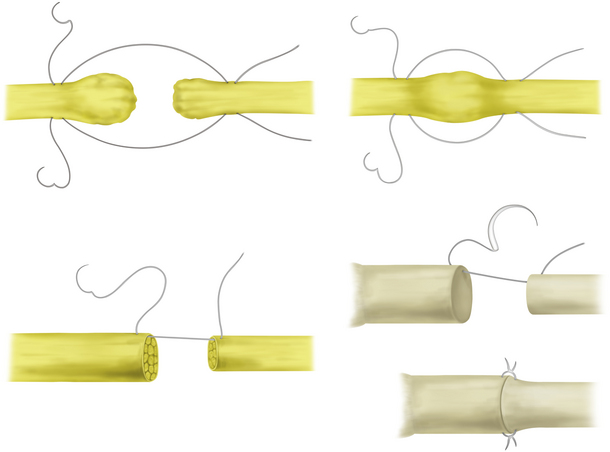
End-to-End Repair
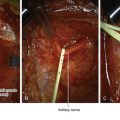
• When a nerve has been transected or has a focal lesion in continuity and trimming of the proximal and distal neuroma does not result in a sizable gap, end-to-end repair without a lot of tension can sometimes be accomplished (Figure 22-1).
• After resection to healthy tissue, the gap is small enough to be closed by drawing the resultant trimmed stumps together. An epineurial end-to-end repair is the standard nerve repair.
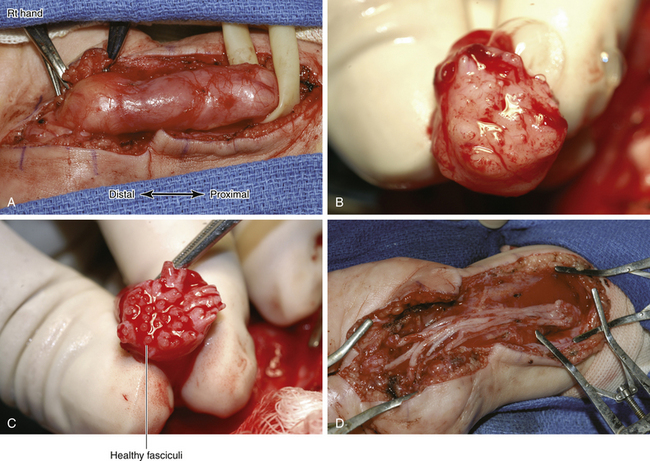
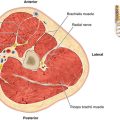
• The important step, once repair is deemed necessary, is to trim both nerve ends to healthy fascicular structure (Figure 22-2, left). Some form of magnification aids in determining a healthy fascicular pattern (see Figure 22-2, right).
• If there is significant hemorrhage from either stump, the stump is gently grasped between the surgeon’s thumb and index finger, and saline is dripped on the stump. If patience is not rewarded, the offending vessel should be accurately cauterized with a fine bipolar forceps.
• Once this is done, it is time to suture the stumps together. On occasion, the longitudinal epineurial vessels on either stump can be used as a guide to help align the stumps. We prefer to pass the needle through the lateral epineurium. This is done at a similar site on the opposite stump and repeated on the opposite side of the nerve at 180 degrees.
• These sutures are then tied, usually simultaneously, by the surgeon and surgeon’s assistant (Figure 22-3).
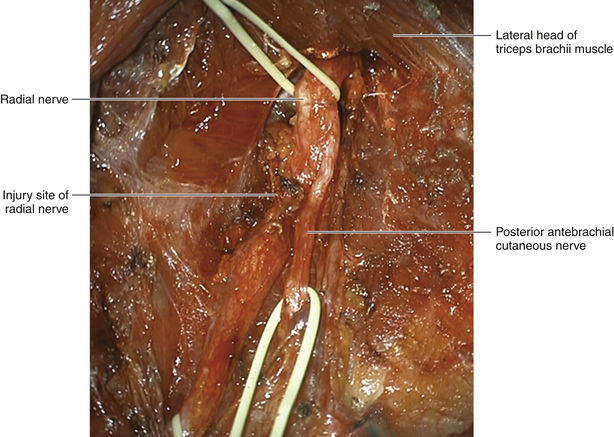
• Suture line tension is minimized by mobilizing the proximal and distal stumps. In some circumstances (e.g., splitting off the origin of musculocutaneous nerve from the lateral cord), considerable relaxation is achieved. In other circumstances (e.g., ulnar and radial nerves), transposition will shorten the gap. In other sites (e.g., midarm median nerve), little can be gained.
• We use only slight joint flexion to shorten the interval between stumps. If significant joint flexion is required, we utilize grafts instead.
• After the lateral sutures are tied, sutures are placed halfway between each lateral suture and then between that suture and the lateral one and so forth until an anterior row of sutures is placed (Figure 22-4).
• The lateral sutures are reversed to invert the nerve so that the backside is exposed. This is then sutured in the same way as the anterior side of the nerve.
• We then like to roll the repair site between a moistened forefinger and thumb to straighten out the fascicular structure and align the two stumps as well as possible.
• When proximal and distal nerve stumps are of different sizes, it is especially important to use the preceding technique so that the stumps are well apposed.
• Visualization of fascicular architecture may be of value so that previously connected fascicles can be realigned fairly accurately. This can sometimes be done even though the repair is at an epineurial rather than a fascicular level.
Perineurial Suture
• A discussion of end-to-end repair raises the question of individual versus group fascicular repair. We occasionally do fascicular end-to-end repair in a split repair, when grafts are not necessary (seldom the case), but not when the whole cross section of the nerve needs repair. Much depends on the fascicular structure of the damaged nerve. If there are only a few fascicles, they should be matched as closely as is possible. If a group of fascicles are solely motor or sensory, and those groups can be reasonably defined in both proximal and distal stumps, those particular proximal and distal elements should be apposed.
• Our experimental studies showed few advantages and some disadvantages to such an internal fascicular repair, perhaps because of the increased manipulation of fascicles necessary, so we only employ these techniques in those selected cases suggested above.
• In wrist-level median nerve transection, the proximal and distal stump sensory fascicle (usually fairly large at this level) is identified and sutured separately from the motor fascicles.
• Most end-to-end epineurial sutures are done with a nonabsorbable 6-0 suture, whereas smaller nerves such as the digital or sensory nerves of the arm, or individual fascicles, are repaired with 8-0 or 10-0 suture.
• Heparinized saline, dripped on the suture line by the assistant with a syringe and blunt plastic needle, helps keep the field clear while surgery is under way.
• Microsurgical instruments must be handled with care between cases so they are in pristine condition at the time of surgery. All microsurgical techniques should be mastered in the laboratory, before entry into the operating room. The rat sciatic nerve is an excellent model for beginners.
• Loupes are used for most repairs of larger nerves, but the microscope is used for smaller nerves and in infants. The microscope is particularly helpful in providing excellent illumination and view for both the surgeon and the assistant.
Split Nerve Repair
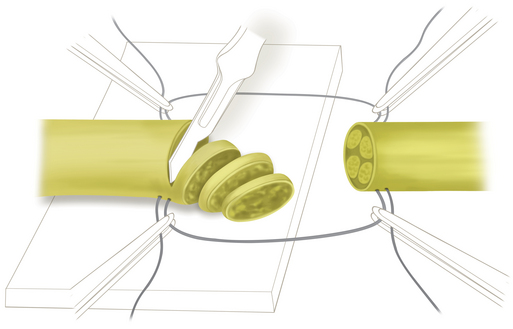
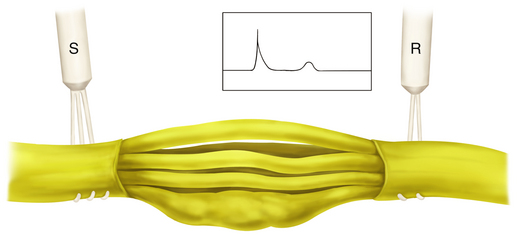
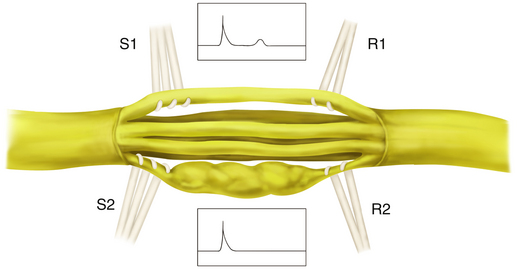
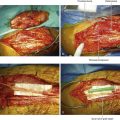
• This type of repair is done when a lesion in continuity is encountered that transmits a nerve action potential (NAP), yet gross examination reveals a portion of the cross section of the nerve to be more involved or damaged than the rest (Figure 22-5).
• The concept forms the basis for splitting peroneal and tibial nerves apart and testing each independently in a sciatic nerve injury. In smaller nerves, microsurgical technique is employed to sort damaged from undamaged fascicles or groups of fascicles.
• This technique is crucial if surgery is not to add damage to a preoperative clinical picture. For example, if a median nerve is repaired to regain sensation in the presence of reasonable thenar muscle function, it is essential that the recurrent branch be split back through the injury site and preserved while the sensory fascicles are grafted.
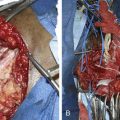
• The damaged fascicles are surgically split off and tested by NAP recordings, and the traces are compared with those from the healthier-looking portion of the nerve (Figure 22-6).
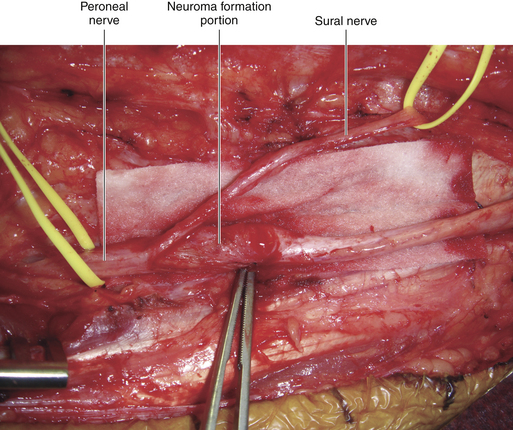
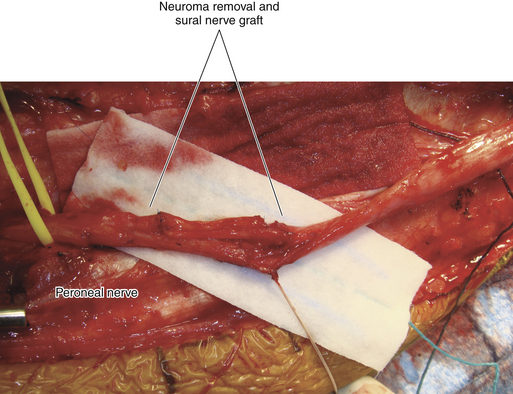
• If there is no NAP conduction in the more damaged portion of the cross section of the nerve, that part is resected and repaired, usually with grafts (Figure 22-7).
• This procedure is usually easier than a graft repair of the whole nerve, because the stumps are stabilized by the portion of nerve left behind, which only requires a neurolysis and is not resected or repaired (Figures 22-8 and 22-9).
• Outcomes in this category of split repair are, not surprisingly, relatively favorable when compared with total repair of the cross section, whether done by end-to-end suture or by graft.
Graft Repair
Autografts
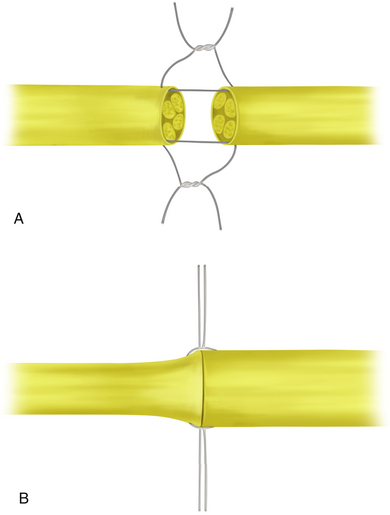
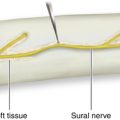
• When the gap is too great for end-to-end repair, autografts are harvested and a fascicular or grouped interfascicular graft repair is done, depending on the oligofascicular or polyfascicular nature of the two stumps. Repair gaps are carefully measured, and incisions for donor grafts of the needed length are placed (Figure 22-10).
• The graft source is influenced by a number of factors, including convenient anatomical proximity, injury to potential graft sites, and other specific issues. In general, sources for grafts in order of preference are:
• Of these, the use of sensory nerves of the caliber of the sural, antebrachial cutaneous, or SSR nerves rather than mixed motor-sensory nerves is favored.
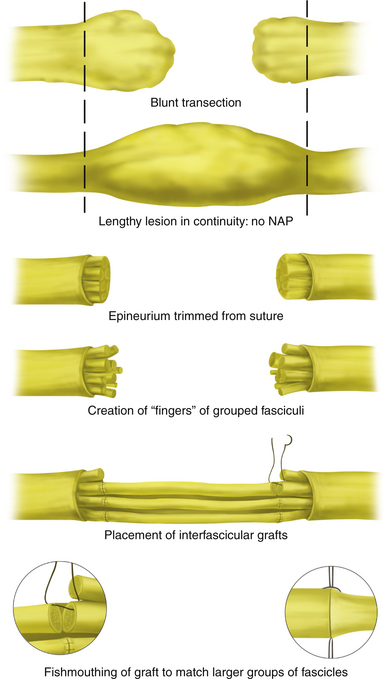
• Multiple strands are placed from a large proximal fascicle to a large distal fascicle. Alternatively, grafts from small groups of fascicles proximally are placed to small groups distally, depending on the fascicular architecture of the two stumps (Figure 22-11).
• Grafts are placed to reconnect appropriate fascicular groups whenever possible. This works best for short lesions, where the gap is relatively short and thus the faces of the two stumps resemble each other in fascicular pattern.
• When a lengthy lesion has been resected, matching fascicles by interposed grafts is of course difficult. In general we connect groups of those proximal fascicles in the vicinity of 3, 6, 9, and 12 o’clock to those groups of fascicles at 3, 6, 9, and 12 o’clock in the distal stump (Figures 22-12 to 22-14).
• We use fine 7-0, 8-0 or10-0 suture to do this. The ends of the grafts are spread or “fishmouthed” with suture as they are apposed to groups of fascicles.
Harvesting the Graft
• Grafts must be harvested, which means that limbs must be prepared.
• Either open or closed methods of harvesting grafts may be employed, but it is essential not to damage the donor nerve in the harvesting process.
• Once removed, the graft is taken to the back operating table, trimmed of excess fat or attached vessels, and measured into segments 10% longer than the measured gap between the stumps.
• Graft segments are kept in a bowl of sterile saline until ready to be used for the repair.
Inserting the Graft
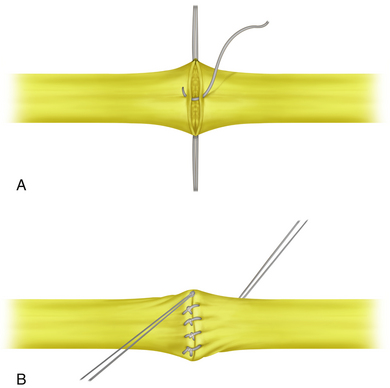
• Either the proximal or the distal end can be sewn in steps or done individually—first the proximal and then the distal end.
• It is best to estimate the number of grafts needed to fill as much of the volume of the nerve as possible.
• Proper preparation of each stump to be grafted is very important.
• Scarred epineurium is resected, and groups or “fingers” of fascicles are created by dissecting down the face of each stump with a scalpel or microscissors.
Graft Apposition
• Bleeding is irrigated away or sometimes tamponaded with a fragment of muscle or Gelfoam. The use of bipolar cautery is necessary for larger interfascicular bleeding points.
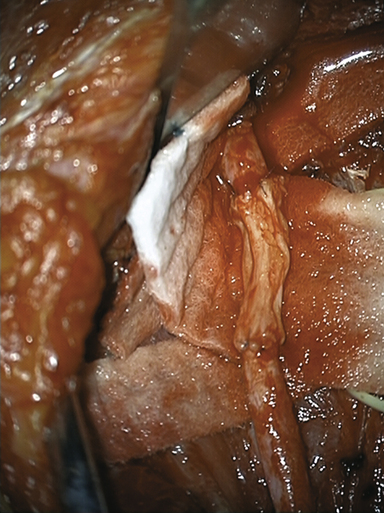
• Interfascicular epineurium is resected from around those groups of fascicles so that they are exposed for a few millimeters. This permits fairly accurate apposition of the grafts to groups of fascicles.
• The grafts should be gently apposed and held by only two or three fine sutures on each graft end.
• The repair area should be kept moist with mildly warm, heparinized saline.
Graft Site Environment
• The environment around the graft site is important. It should be cleared of scar tissue as much as possible to provide a good blood supply to the graft site from healthy tissues.
• Graft repair is difficult at certain sites, such as brachial plexus spinal nerves at an intraforaminal level, the pelvic plexus, or the sciatic nerve near the sciatic notch. Graft repair at these sites requires special patience, perseverance, and experience.