93 Epilepsy
Salient features
Examination
• Ask the patient about aura, whether she bit her tongue, whether she was incontinent during the attack, any hallucinations (déjà vu phenomenon). Ask the patient about triggering factors (including television, disco strobes, hypoglycaemia and alcohol ingestion) and whether they are recurrent. Take a family history (about 30% of patients with epilepsy have a history of seizures in relatives), and past history of head injury.
• Confirm this by asking the eye-witness about the description of seizures (note whether they were tonic–clonic), frothing at the mouth, whether the patient was unconscious or incontinent, how long the whole ‘episode’ lasted and how long she was unconscious after the attack, and whether there was any weakness after the attack (Todd’s paralysis).
• Tell the examiner that you would like to evaluate for depression (~55% of patients with uncontrolled seizures are depressed. Patients with well-controlled seizures have rates of depression that are greater than rates the general population, and suicide rates are three-fold, with the highest rates in the 6 months after diagnosis). Since antiepileptic drugs cause mood changes, it is appropriate to evaluate mood before starting therapy.
Questions
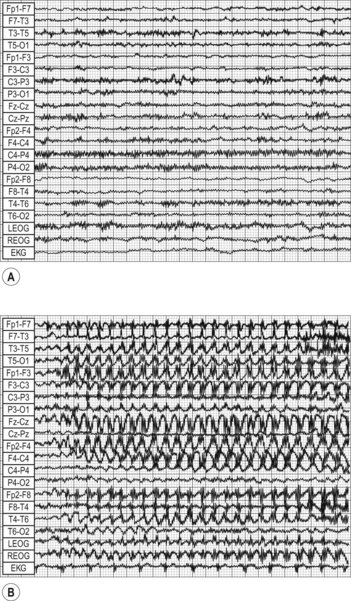
How would you investigate the patient?
How would you classify seizures?
• Generalized seizures: grand mal (tonic–clonic) seizures, petit mal and atypical absences, myoclonus, akinetic seizures. Petit mal describes only 3 Hz seizures rather than clinically similar absence attacks, which are partial seizures.
• Partial or focal seizures (a partial seizure is epileptic activity confined to one area of cortex with a recognizable clinical pattern): simple partial seizures (no impairment of consciousness), complex partial seizures, partial seizures evolving to tonic–clonic.
Advanced-level questions
What is Todd’s paralysis?
Paresis of a limb or hemiplegia occurring after an epileptic attack, which may last up to 3 days.
How would you manage epilepsy?
• General advice: avoid ladders, heights, unsupervised swimming and cycling for 2 years from the last episode
• Antiepileptic drugs: the first-line drugs for epilepsy monotherapy remain carbamazepine and sodium valproate; phenytoin is now used less often. Although lamotrigine has a monotherapy licence, its place has still to be defined. Several new ‘add on drugs’ have been licensed in recent years including vigabatrin, gabapentin, lamotrigine and topiramate. An overview of trials in patients with refractory partial seizures suggests no major differences between these agents in either efficacy or tolerability (BMJ 1996;313:1169–74). Prolonged use of vigabatrin can result in severe visual field defects, prompting the development of guidelines for monitoring vision (BMJ 1998;317:1322). The SANAD trial suggested that lamotrigine is the drug of first choice in patients with partial seizures, and valproate for patients with generalized or unclassified seizures in the absence of factors that would lead to an alternative choice. Valproic acid was more effective than lamotrigine and topiramate in generalized seizures. Lamotrigine had almost twice the failure rate because of inadequate seizure control, whereas topiramate was similarly effective in controlling seizures but had a higher failure rate caused by discontinuation because of side effects (Lancet 2007;369:1016–26). Ethosuximide and valproic acid were more effective than lamotrigine in the treatment of childhood absence epilepsy. Valproate, compared with other commonly used antiepileptic drugs, was associated with an increased risk of impaired cognitive function at 3 years of age and risk of birth defects. Therefore, it should be avoided as a first-choice drug in women of childbearing potential; risks of valproate should be balanced with the risks of uncontrolled seizures.
• Vagal stimulation remains an experimental approach in seizure control (J Clin Neurophysiol 1997;14:358–68).
• Advice about driving: those who have had more than one seizure are unable to hold a driving licence in the UK unless they have been free from any form of epileptic attack while awake for a period of 1 year before the issue of a licence or, in the case of attacks while asleep, these attacks must have occurred only while asleep over a period of 3 years and no awake attacks before the issue of a licence. Drivers of heavy goods vehicles and public service vehicles must have been free of epileptic attacks for at least the last 10 years and must not have taken anticonvulsant medications during this 10-year period.
• Patients should be discouraged from participating in other activities for which a history of seizures increases the risk of injury or death, such as operating high-risk power equipment, working at heights and swimming or bathing alone.
• Women who intend to use oral contraceptive pills and are taking phenytoin, carbamazepine, phenobarbital, topiramate or oxcarbazepine (these drugs induce hepatic enzymes to increases clearance of oral contraceptives) should be advised to use preparations containing at least 50 µg ethinylestradiol in order to reduce the chance of pregnancy. Valproate should also be avoided because of the risk of teratogenicity.
What do you understand by the term status epilepticus?
It is a medical emergency where seizures follow each other without recovery of consciousness.
What do you know about the pathogenesis of epilepsy?
• Neuronal networks between thalamus and cerebral cortex, as in absence seizures
• Intrinsic neuronal function as in channelopathies: mutations in SCN1B, which encodes a voltage-gated sodium channel subunit, are associated with generalized epilepsy with febrile seizures; mutations in KCNQ2 and KCNQ3, which both encode potassium channels, are associated with benign familial neonatal convulsions.