Chapter 14 Epiduroscopic Adhesiolysis
With epiduroscopy, it is now possible to directly observe pathologic conditions such as epidural fibrosis, perineural scars, postoperative tissue changes, herniated nucleus pulposus, and hypertrophied ligamentum flavum. Several new procedures have also been made possible by epiduroscopy. Through manipulation of the equipment, the adhesion or fibrosis of the perineural area can be lysed. With insertion of an epidural catheter, chemical adhesiolysis can be performed. Also, drugs can be more effectively administered to a target nerve [1].
There are, however, a few limitations of epiduroscopic adhesiolysis. During epiduroscopy, the epidural space can be visualized only if it is kept distended by repeated injections of saline. More importantly, epiduroscopic procedures can elevate the intracranial pressure and intraorbital pressure. The procedural time requires 45 to 60 minutes for lumbar epidural space examination [2–5].
Preoperative preparation
Imaging Diagnosis
Magnetic resonance imaging or computed tomography of the lumbar and sacral spine should be considered to assess the contents of spinal canal and seek spinal stenosis [7].
Indications
Complications
The following complications may occur after epiduroscopic adhesiolysis:
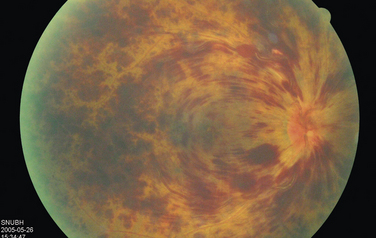
 Retinal hemorrhage and temporal blindness (Fig. 14-2) can occur when the sudden increase in epidural pressure is transmitted to the subarachnoid space [11]. The optic nerve and its vasculatures may be compressed by the resulting higher cerebrospinal fluid pressure. The vasculature compression may rupture retinal blood vessels.
Retinal hemorrhage and temporal blindness (Fig. 14-2) can occur when the sudden increase in epidural pressure is transmitted to the subarachnoid space [11]. The optic nerve and its vasculatures may be compressed by the resulting higher cerebrospinal fluid pressure. The vasculature compression may rupture retinal blood vessels.Instrumentation
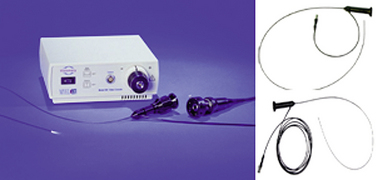
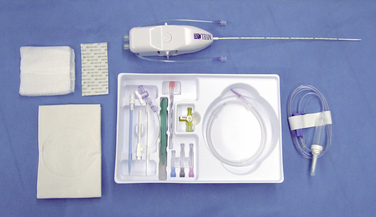
Instruments
The instruments and supplies needed for epiduroscopic adhesiolysis are as follows:
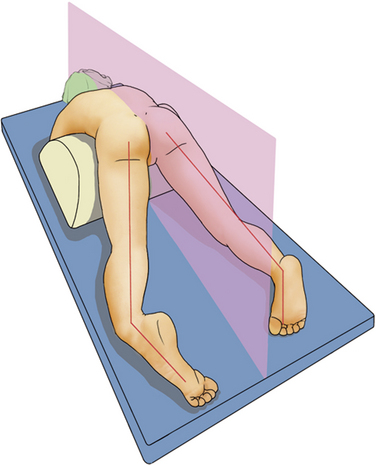
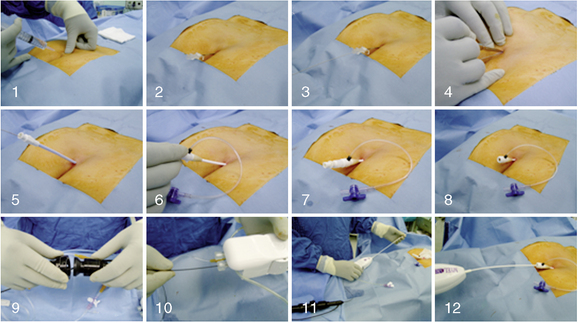
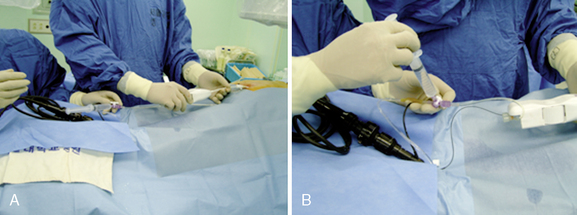
Procedure
Postprocedural management
 A postoperative neurologic examination should be performed. If any new neurologic deficits are detected, magnetic resonance imaging and neurologic consultation should be considered.
A postoperative neurologic examination should be performed. If any new neurologic deficits are detected, magnetic resonance imaging and neurologic consultation should be considered.BOX 14.1 Regimen for Chemical Epiduroscopic Adhesiolysis
The use of hypertonic saline has been controversial. We, therefore, do not use the hypertonic saline for epidural adhesiolysis procedure.
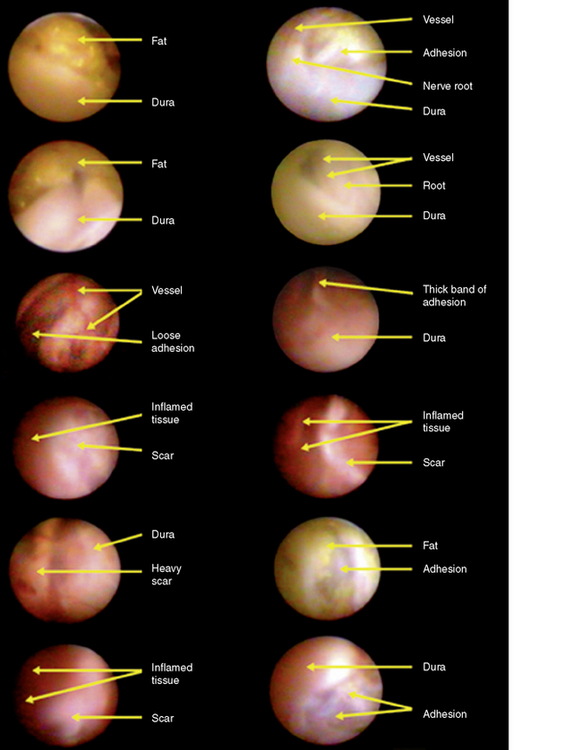
Epiduroscopic findings
Table 14.1 and Figure 14-12 illustrate common epiduroscopic findings during the adhesiolysis procedure.
Table 14.1 Characteristics of Structures Seen on Epiduroscopic Images
| Structure | Characteristics |
|---|---|
| Epidural fat | Yellowish, loose globular, and glistening |
| Dura mater | Convex, tubular, gray-white, with blood vessels on the surface, giving the appearance of a road map |
| Nerve root |
Data from http://www.myelotec.com/en/phys/anatpath.html
Case study 14.1
On the epidurogram taken during epiduroscopy, a complete filling defect of contrast agent was noted above the left L5-S1 disc level, whereas contrast agent flowed freely into the right epidural space (Fig. 14-13B). Many fibrous bands of tissue, white avascular scars, and inflamed erythematous tissue were noted around the left L5 foramen. After left L5 mechanical adhesiolysis, flushing with normal saline, and injection of hyaluronidase 1500 IU, the steerable catheter could freely pass the L5 neural foramen (Fig. 14-13C).
1 Schmerztherapeutisches Kolloquiurn, Iserlohn, G. Schütze, Hagenerstr. 121, 58642 Iserlohn. http://schmerz-ambulanz.com/index.php?option=com_content&view=article&id=71:epiduroskopie-konsensus &catid=18:publikationen&Itemid=51
2 Blomberg R., Olsson S. The lumbar epidural space in patients examined with epiduroscopy. Anesth Analg. 1989;68:157-160.
3 Saberski L.R., Kitahata L.M. Direct visualization of the lumbar epidural space through the sacral hiatus. Anesth Analg. 1995;80:839-840.
4 Manchikanti L., Rivera J.J., Pampati V., et al. One-day lumbar epidural adhesiolysis and hypertonic saline neurolysis in treatment of chronic low back pain: A randomized, double-blind trial. Pain Physician. 2004;7:177-186.
5 Manchikanti L., Boswell M.V., Rivera J.J., et al. [ISRCTN 16558617] A randomized, controlled trial of spinal endoscopic adhesiolysis in chronic refractory low back and lower extremity pain. BMC Anesth. 2005;5:10.
6 Saberski L.R. Current application of spinal canal endoscopy: Is it a diagnostic tool or a therapeutic modality? In: Syllabus: Current Concepts in Acute, Chronic and Cancer Pain Management ‘99. New York: The World Foundation for Pain Relief and Research; 1999:171-181.
7 Krasuski P., Poniecka A.W., Gal E., et al. Epiduroscopy: Review of techniques and results. Pain Clinic. 2001;13:71-76.
8 Igarashi T., Hirabayashi Y., Seo N., et al. Lysis of adhesions and epidural injection of steroid/local anesthetic during epiduroscopy potentially alleviate low back leg pain in elderly patients with lumbar spinal stenosis. Br J Anesth. 2004;93:181-187.
9 Racz G.B., Holubec J.T. Lysis of adhesions in the epidural space. In: Racz G.B., editor. Techniques of Neurolysis. Boston: Kluwer Academic; 1989:73-86.
10 Manchikanti L., Singh V. Epidural lysis of adhesions and myeloscopy. Curr Pain Headache Rep. 2002;6:427-435.
11 Amirikia A., Scott I.U., Murray T.G., Halperin L.S. Acute bilateral visual loss associated with retinal hemorrhage following epiduroscopy. Arch Ophthalmol. 2000;118:287-289.
12 Heavner J.E., Racz G.B., Raj P. Percutaneous epidural neuroplasty: Prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 1999;24:202-207.