Epidemiology as a Basis for Informing Contemporary Physical Therapy Practice
To address the gap between lifestyle practices and the body of knowledge on the relationship between lifestyle choices and health,1 a societal commitment to reducing the number of patients rather than increasing the focus on biomedical care (drugs and surgery) has never been more urgent. Physical therapists are uniquely qualified and strategically positioned as health care professionals to lead in the translation of this well-established body of knowledge into daily practice.2 A consideration of the risks of lifestyle-related conditions in every individual is consistent with a comprehensive model of best practice in the context of epidemiological trends—that is, evidence-based practice in the context of practice priorities that are themselves informed by evidence. This chapter expands these concepts and outlines principles for applying them proactively and as a priority in the health care of every patient. Physical therapists can have a major impact on the leading priorities of health care, one individual at a time.
What Is Health?
The World Health Organization (WHO) defines health as “a complete state of physical, emotional and social well-being”—not merely the absence of disease and impairment.3 Although physical well-being contributes to health in the other dimensions, it does not ensure health. Thus emotional and social well-being should be assessed as systematically as is physical well-being in a model of care based on health. Collectively, these domains of health translate into an individual’s capacity to perform activities that enable him or her to participate fully in life.4 The WHO’s definition of health has not been amended since 1948. Although having withstood time, this definition has failed to be incorporated as the primary goal of contemporary health care.
Because of widespread immigration, the cultural and ethnic demographic profiles of high-income countries such as those in North America and Europe are changing rapidly. Beliefs, attitudes, values, cultures, ethnicity, and traditions affect health, ill health, and their interactions, including how often individuals seek health care. For example, Asian immigrants to the United States report fewer stress-related and psychological problems than do non-Hispanic Caucasians.5 With increasing time in the United States, however, reports of stress increase for Asian Americans. This may reflect a number of factors: cultural differences in the acceptability of reporting psychological distress (leading to underreporting by members of some cultural groups), sensitization to the definition and the awareness of stress with increasing duration of residence, or the compounding effect of increasing stress in the new culture. How best to reduce racial and ethnic disparities through culturally competent health care is a matter of debate and requires such outcomes as client satisfaction, improved health status, and culturally appropriate management and delivery across racial and ethnic groups.6,7
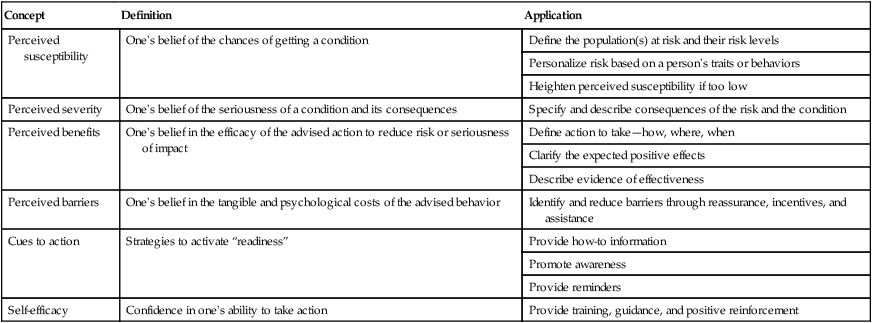
Since the psychobiological adaptation model was posited over 25 years ago,8 the few models of physical therapy practice that have been reported have included psychosocial and other nonphysiological components.9–11 Psychosocial components include health belief, self-efficacy, and perceived control. The Health Belief Model is useful in appreciating the ways in which belief may affect health, illness, and the responses and reactions to them (Table 1-1).12 Assessment of self-efficacy provides an index of an individual’s sense of mastery over his or her health and well-being. These concepts can be used in a clinician’s practice setting. A few questions can help assess a patient’s perception of susceptibility to risk or a condition. These concepts can provide a basis for health education that includes increasing the patient’s awareness of the effects of lifestyle factors on health and of their consequences. The action necessary to avoid the condition or minimize its risk can be selectively targeted for each individual when the individual’s context is known.
Table 1-1
Concepts of the Health Belief Model
| Concept | Definition | Application |
| Perceived susceptibility | One’s belief of the chances of getting a condition | Define the population(s) at risk and their risk levels |
| Personalize risk based on a person’s traits or behaviors | ||
| Heighten perceived susceptibility if too low | ||
| Perceived severity | One’s belief of the seriousness of a condition and its consequences | Specify and describe consequences of the risk and the condition |
| Perceived benefits | One’s belief in the efficacy of the advised action to reduce risk or seriousness of impact | Define action to take—how, where, when |
| Clarify the expected positive effects | ||
| Describe evidence of effectiveness | ||
| Perceived barriers | One’s belief in the tangible and psychological costs of the advised behavior | Identify and reduce barriers through reassurance, incentives, and assistance |
| Cues to action | Strategies to activate “readiness” | Provide how-to information |
| Promote awareness | ||
| Provide reminders | ||
| Self-efficacy | Confidence in one’s ability to take action | Provide training, guidance, and positive reinforcement |
From Stretcher VJR, Rosenstock IM: The health belief model. In Glanz K, Lewis FM, Rimer BK, editors: Health behavior and health education: theory, research and practice, San Francisco, 1977, Jossey-Bass.
The International Classification of Functioning, Disability and Health advocated by the WHO interrelates body functions and structures, activity, and participation in life.4 The biomedical model focuses on impairment (i.e., body functions and structures), with less attention to health and wellness, sickness impact, life satisfaction, and quality of life, which reflects an individual’s participation in life and associated activities. One problem that occurs when the primary focus is on the remediation of limitations of function and structure in managing the leading health care priorities of our day (i.e., chronic lifestyle-related conditions) is that such limitations do not necessarily affect activity and participation—the essence of a meaningful life. These relationships need to be evaluated in each case rather than assumed.
The integration of health belief and motivational models has been a means of incorporating psychosocial dimensions of care, interventions, and outcomes so as to directly focus on an individual’s limitations of activity and participation. As a result of this paradigm shift, an increasing number of measurement tools are available to assess the dimensions of health. These tools can be categorized as generic, as having general application across individuals and conditions, or as having specific application to a cohort of individuals, based on age, condition, or some other variable (see examples in Chapter 17). Many of these scales have been validated on a subset of these cohort groups. Physical therapists need to be able to use these tools knowledgeably and specifically to assess outcomes in their practices, just as they use conventional tools to assess and evaluate anatomic structure and physiological function. One such measure is the Short Form-36, which evaluates health-related quality of life and has become an established tool for general use and has been adapted cross-culturally.13,14 Such tools can be used to evaluate the individual’s perception of health improvement, which supplements conventional objective clinical measures.
The Paradox
People living in high-income countries (e.g., countries in North America and Europe, and some Asian countries) and, increasingly, in countries whose economies are growing are experiencing a paradox: an increase in the negative impact of a more Western lifestyle combined with an increase in advances in biomedicine. Technological and economic advances have been proposed as factors contributing to an obesity-conducive environment.15 The effects of low activity (hypokinesis) and poor nutritional choices on health in Western countries have been reported to be synergistic and partially additive,16 although a potent interaction may exist. The power of nonpharmacological interventions and solutions to affect global health priorities related to chronic lifestyle-related conditions can no longer be considered secondary to pharmacological solutions.17,18 Rather, they may need to be considered foremost.
A nationwide, population-based strategy to improve lifestyle is the primary means of improving a country’s overall health and minimizing morbidity and premature mortality from chronic lifestyle-related conditions with the least risk and cost.19–21 Even a modest reduction in cardiac risk factors, for example, could save approximately three times as many life-years as invasive interventions.22 Preserving and maximizing health in the most cost-effective, low-risk, and ethical manner warrant being universal health care priorities in the 21st century to stem the tide of chronic lifestyle-related conditions.
Lifestyle-Related Conditions
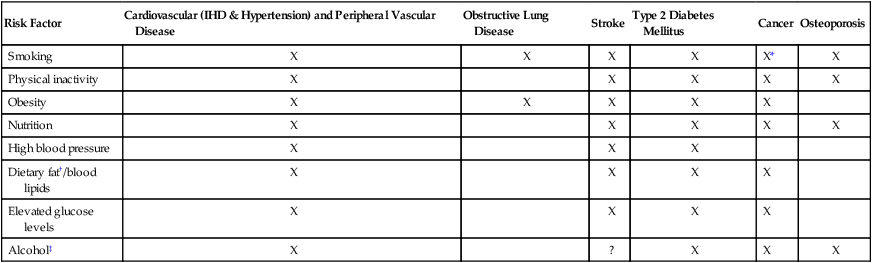
Poor nutritional choices and sedentary lifestyles combined with tobacco use, excessive alcohol consumption, and stress underpin chronic lifestyle-related conditions in high-income countries, and they pose the greatest threats to public health.23–25 Eight major risk factors related to lifestyle and their documented impacts on health appear in Table 1-2. This trend has given rise to dramatic increases in a relatively newly defined condition, metabolic syndrome, which includes insulin resistance, high blood pressure, elevated triglycerides and cholesterol, and obesity. With industrialization and technological advances, lifestyle-related conditions are on the rise in low- and middle-income countries as well.26,27 Despite their prevalence, however, the WHO has long proclaimed that lifestyle-related conditions are largely preventable.28
Table 1-2
Major Modifiable Risk Factors for Lifestyle-related Conditions
| Risk Factor | Cardiovascular (IHD & Hypertension) and Peripheral Vascular Disease | Obstructive Lung Disease | Stroke | Type 2 Diabetes Mellitus | Cancer | Osteoporosis |
| Smoking | X | X | X | X | X* | X |
| Physical inactivity | X | X | X | X | X | |
| Obesity | X | X | X | X | X | |
| Nutrition | X | X | X | X | X | |
| High blood pressure | X | X | X | |||
| Dietary fat†/blood lipids | X | X | X | X | ||
| Elevated glucose levels | X | X | X | X | ||
| Alcohol‡ | X | ? | X | X | X |
*An increased risk of all-cause cancer. Smoking is not only related to cancer of the nose, mouth, airways, and lungs; smoking increases the risk of all-cause cancer.
†Partially saturated, saturated, and trans fats are the most injurious to health.
‡Alcohol can be protective in moderate quantities, red wine in particular.
Modified from the Heart and Stroke Foundation of Canada, 2003; Bradberry JC: Peripheral arterial disease: pathophysiology, risk factors, and role of antithrombotic therapy, Journal of the American Pharmacy Association 44(2 Suppl 1):S37–S44, 2004; Charkoudian N, Joyner MJ: Physiologic considerations for exercise performance in women, Clinics in Chest Medicine 25:247–255, 2004.
Atherosclerosis is the major common denominator and contributor to lifestyle-related conditions, including ischemic heart disease (IHD), hypertension, and stroke. Factor analysis supports a two-factor solution for heart disease and possibly for other lifestyle-related conditions: family history (factor 1) and lifestyle factors such as smoking, serum cholesterol, blood pressure, nutrition, exercise, and weight control (factor 2).29 At the population level, choosing health—which includes smoking abstinence along with optimal nutrition and exercise throughout life—can enhance the quality of life, decrease the prevalence of chronic lifestyle-related conditions, and reduce the burden of these conditions on individuals, families, communities, and countries, including suffering and health care costs.30–32
Life Cycle and Lifestyle-Related Conditions
IHD secondary to atherosclerosis continues to be the leading cause of premature mortality and disability in industrialized countries. The prevention and management of risk factors of systemic atherosclerosis should be a primary target of contemporary care for children as well as for adults.33–35 Ischemic cerebrovascular, coronary, and peripheral vascular conditions are manifestations of the same underlying pathological process, blood vessel narrowing caused by atherosclerosis and thrombosis. Smoking, a high-fat diet, and inactivity can precipitate damage to the endothelium and fat deposition within arterial walls. This common pathway has been associated with increased fibrinogen and C-reactive protein, markers of inflammation.36 The focus of biomedical research has shifted to the role of inflammatory mediators and the contribution of low-density lipoproteins to atherosclerosis and away from the concept of degenerative vessel disease. Fibrinogen is an inflammation mediator and a clotting factor. People with cardiovascular disease have high fibrinogen levels, which further increase the risk for thrombosis and manifestations of circulatory disease. Inflammation has been implicated in a growing number of chronic conditions, such as IHD, stroke, asthma, gastrointestinal ulcers, cirrhosis of the liver, Alzheimer disease, cancer, and autoimmune conditions.37,38 Unhealthy lifestyle choices have been thought to contribute to a proinflammatory state, giving rise to low-grade infection in various organ systems and leading to the signs and symptoms associated with various chronic degenerative processes.39 Although this is an important finding, a proinflammatory milieu and inflammation are not the causes of the chronic conditions with which they have been associated but, rather, are precipitating effects of traumas resulting from lifestyle.
Lifestyle-related conditions can no longer be considered adult conditions or age-related conditions. Children are exhibiting signs of cardiovascular disease, including arterial atherosclerotic streaking, hypertension, type 2 diabetes mellitus, and obesity.40 Forty years ago, these conditions manifested in adults. With sedentary lifestyles, low activity, and poor nutrition, children are showing the results of accumulated injury to blood vessels and larger body frames and weights. As a consequence, children today are manifesting lifestyle-related conditions earlier than previous generations and are thus expected to die prematurely from these conditions and to have shorter life expectancies than their parents. Throughout their lives, these individuals can expect to have prolonged morbidity associated with these conditions, the secondary complications of these conditions, associated adverse responses to other health complaints, and increased iatrogenic problems (secondary to drugs and surgery).41,42 Health promotion strategies directed toward parents and young children will help to offset the population’s health threat of lifestyle-related conditions.
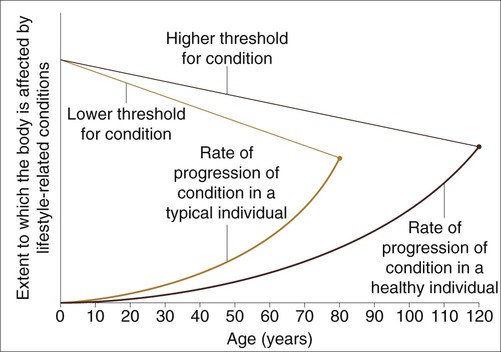
Life expectancy has almost doubled since 1900. The post–World War II baby-boom generation characterizes the demographics of many industrialized countries. This cohort has lived in prosperous times and up to that time was the longest living generation in history. Despite the prosperity seen by the baby boomers, this era was associated with more sedentary lifestyles and access to food products low in nutritional value. Although the manifestations of lifestyle-related conditions are associated with aging, they are not necessary consequences of aging. This is based on cross-cultural comparison studies. Optimal nutrition, exercise, stress control, smoking abstinence, and moderate alcohol consumption, if any, are central to reducing the probability of chronic lifestyle-related conditions and associated disability and maximizing quality of life as people age.43 In particular, increased quality of life with a higher threshold for chronic lifestyle-related conditions and less morbidity toward the end of life is the objective. Figure 1-1 shows the theoretical increase in the threshold of these conditions with healthy lifestyle choices (i.e., not smoking, optimal nutrition and weight control, regular physical activity and exercise, optimal sleep, and reduced stress) and reduced rate of progression of chronic conditions. Ostensibly, the net result is more “life to years” as well as more “years to life.”
“First Do No Harm”
As primarily a noninvasive health care profession, physical therapy is uniquely positioned to have a primary role in promoting health and wellness, while also preventing, managing, and in some cases, reversing these pandemic lifestyle-related conditions, objectives that commonly coexist because they share a common pathway.44 Integrating health promotion into practice would directly address the ultimate knowledge translation gap in health care (with respect to the benefits of healthy living).45 Indeed, focusing on health promotion, in addition to directly addressing the risk factors and/or manifestations of secondary lifestyle-related conditions, may result in more favorable outcomes for a patient’s presenting problem. Triage of individuals by both noninvasive practitioners and invasive practitioners would constitute a bold initiative in health care. Such triage could establish whether a patient’s complaint is best managed in the short and long term wholly noninvasively, wholly invasively, or by some combination, with a view to weaning the patient off medications or minimizing the medication. Similarly, every effort should be made to avoid surgical intervention and its risks whenever possible (i.e., surgical intervention as a last resort rather than a first resort) by exploiting noninvasive interventions and strategies to restore health and promote lifelong health. When an individual enters the health care delivery system, her or his receptivity to health information is likely to be high. This is a prime opportunity to evaluate risk factors and prescribe a lifelong health plan.
The effectiveness of nonpharmacological treatments in the management of chronic lifestyle-related conditions has been well documented, but implementation has been poor.46–48 As noninvasive practitioners, physical therapists have a primary role on the health team, which may include physicians and surgeons (i.e., invasive practitioners), nurses, nutritionists, pharmacists, social workers, psychologists, respiratory therapists, spiritual leaders, and others, depending on the requirements of each case. On a broader level, physical therapists can serve in a multisector capacity as consultants and work alongside health care policy makers, corporate business people, urban planners, and architects in developing healthy and safe homes, workplaces, recreational facilities, and communities. The role of the physical therapist clinician is shifting from hospital-based acute care and private practice to the community, schools, industry, home, workplace, and playing field.
Biomedical research that evaluates drugs and surgery often lacks control groups that are otherwise healthy or a comparative group in the research design that includes a potentially superior, noninvasively managed group where feasible. For example, a 12-month exercise program involving selected individuals with stable coronary artery disease has shown superior event-free survival and exercise capacity when compared with individuals who received percutaneous coronary intervention.49 In another study, the mortality rate of individuals with heart disease has been estimated to be reduced by 20% to 25% with cardiac rehabilitation, which is comparable to the results of established therapies such as beta blockers.50 Cardiac rehabilitation is noninvasive; thus it is cheaper and has few side effects. Management is focused on changing negative health behaviors and maximizing lifelong health rather than on simply altering a sign or a symptom.
Evidence-Informed Practice
Addressing the Health Care Priorities of the Day
Physical therapists treat individuals with chronic lifestyle-related conditions as either primary or secondary diagnoses. Smoking is currently the leading cause and contributor to chronic conditions and premature death in the United States, with poor diet and sedentary lifestyle anticipated soon to overtake tobacco use.51 Television viewing, an indicator of sedentary living, is associated with obesity and is a marker of cardiovascular disease independent of total reported physical activity.51 As noninvasive practitioners, physical therapists have a responsibility to manage these conditions and their risk factors in all patients so as to prevent or control their physical, psychosocial, economic, and societal impact and to promote health in their practices. By prioritizing health and addressing suboptimal health behaviors, regardless of a patient’s primary complaint, the complaint may be mitigated, the rate and quality of recovery potentially improved, and the potential for recurrence reduced.
Our Village
Fundamental to the principle of evidence-informed practice is the fact that health care providers respond to epidemiological indicators and an understanding of the changing demographics and face of our “village.” Lifestyle-related conditions are the leading killers in our village. Men can expect to live 75 years; women, 82 years.52 Functional capacity, however, is estimated to decrease 10% per decade, and half of this decrement is due to sedentary living. Raising children to be healthy and physically active will promote a generation of healthy adults and will thereby delay their physical dependence by 10 to 20 years.
Health care workers with international health organizations are trained to manage the unique needs of their villages. This entails knowing the health priorities of the village and making decisions that positively affect the problems and reduce their impact on the community as a whole. In some parts of the world, a health care worker who focuses on malaria when intestinal parasites are the priority is a hindrance, rather than a help, to that village. Similarly, in our health care climate, physical therapists need to make it a priority to meet the leading needs of their “villages.” Smoking abstinence, good nutrition, weight control, exercise, and stress management are evidence-based noninvasive interventions consistent with the needs of contemporary physical therapy practice; the therapeutic potential and impact of those elements on the health of our village are enormous. For example, each kilogram of weight loss has a dose-dependent effect on health outcomes. Further, as little as 30 minutes of moderately intense activity on most days of the week offsets the deleterious effects of sedentary living.53 With the aging of the people of our village and the signs of lifestyle-related conditions now evident in children and young people, the burden of chronic conditions will be prolonged, particularly as individuals approach the end of life. It has been suggested that life expectancy will plateau or even decrease as a result.42
Indigenous peoples in North America and Australasia have unique health challenges and needs. They tend to be less well educated than the dominant culture, have fewer employment opportunities, experience more violent injuries and deaths, and have poorer health and shorter lives. They have significant health risks because of sociocultural factors and genetic predisposition, such as higher rates of IHD, stroke, type 2 diabetes mellitus, obesity, hypertension, tobacco use, and alcoholism. Large-scale intervention programs are needed for the Native American population based on studies of the health of its children.54 The past few generations have witnessed a shift from indigenous foods to refined grains and foods high in fat and sugar and from active to inactive lifestyles. These trends have exacted an enormous toll in terms of personal and social health indicators.
As individuals age in industrialized countries, their activity levels tend to decline. With relatively long life expectancy in these countries, sedentary lifestyles may prolong end-of-life morbidity. A study of individuals who adhered to exercise programs and those who did not revealed the importance of variables such as self-efficacy, perceived fitness, social support, and enjoyment.55 The results of this study have important implications for urban planning; they can inform the design of healthy communities, as well as individual activity and exercise programs.
A study of black Seventh-day Adventists has provided a unique opportunity to isolate the effects of lifestyle on African Americans. Seventh-day Adventists promote spiritual well-being and a healthy diet and lifestyle. As a result, the health of black Seventh-day Adventists is better and the incidence of chronic lifestyle-related conditions is lower than that of African Americans who are not Seventh-day Adventists.56 In addition, based on the results of a study of a large cohort, Mormons tend to be fitter and have fewer risk factors for IHD than do other Americans.57
The physical activity profiles of African American women have been compared with recommendations for moderate levels of activity.58 In this study, findings showed that few subjects met the recommended levels of daily physical activity. Exercise was performed on fewer than the recommended number of days per week and for less than the recommended 8 to 10 minutes per session. Attention to frequency and duration may be particularly important when counseling African American women about regular physical activity.
African American women have a higher risk for cardiovascular disease and stroke than do Caucasian American women.59 Based on a cross-sectional study of 399 urban African American women, correlates of physical activity within this cohort were identified. Programs to promote physical activity should address the safety of the physical environment and psychosocial factors. Inactive women with less than a high school education and those who perceive themselves to be in poor health should be considered special target groups.
Latina women have a higher risk for cardiovascular disease and stroke than do Caucasian American women; this has been attributed to the higher incidence of obesity and type 2 diabetes mellitus among Latinas.60 The facilitators and barriers to exercising in this cultural cohort have been examined in a cross-sectional study of 300 Latinas. Physical activity has been reported to be higher in younger women, in married women, and in women who had confidence that they could become more active, who saw people exercising in the neighborhood, and who attended religious services.60 The church was recommended as a suitable community setting for initiating programs that provide women with the knowledge, skills, and motivation to become more active and to transmit this information to others in the community through their families.
The impact of gender is being increasingly appreciated in terms of health affliction, access to health care, and physiological responses and psychological reactions to illness.61,62 In a Swedish cohort of older adult individuals, obesity-related health indicators and risk factors were reported to differ in men and women and also to differ on the basis of socioeconomic status.63 In response to cardiac rehabilitation, gender-specific effects on high-density lipoprotein cholesterol have been documented.64 Women demonstrate greater improvement in high-density lipoprotein than do men.
Urbanization, modernization, and immigration are affecting global health. Within industrialized countries, indigenous people are moving from rural to urban areas; this is occurring in the United States, Canada, Australia, New Zealand, and many African countries. Rather than seeing improvements in their health overall, relocated rural people are succumbing to lifestyle-related conditions. Middle-aged black men who move to urban areas from rural South Africa, for example, increase their risk for IHD and stroke.65 One explanation for this observation is increased autonomic reactivity to the stress of relocation; however, other lifestyle factors may be implicated. These patterns have been reported for other groups as well; for example, Mexicans and Asians who move to affluent industrialized countries.66 The typical health advantage for people who move to the West from certain Asian countries, such as Japan, is lost with increasing numbers of years in the new culture.67
Principles of Evidence-Informed Practice
The efficacy of the quick fix (drugs and surgery) in the management of chronic conditions, particularly lifestyle-related conditions, is being seriously questioned. With respect to long-term outcomes, noninvasive interventions may often be more successful.68 Premature mortality can be significantly reduced with regular physical activity, optimal nutrition and weight control, and avoidance of smoking.69 Relative to invasive care, noninvasive interventions associated with physical therapy (health education and exercise) are low in cost; yet access to these noninvasive measures is commonly more limited than access to invasive care.
The Priorities of Our Village
Although most people are aware of the positive benefits of healthy choices, what is less apparent to them is that small changes in health behaviors can result in major effect sizes. These effect sizes most often surpass those of medications targeted at a single sign or symptom. In a study of over 23,000 people between 35 and 65 years old, for example, Ford and his colleagues70 showed that over an 8-year period, people who did not smoke, had a body mass index under 30, were physically active for at least 3.5 hours a week, and followed healthy nutritional principles had a 78% lower risk for developing a chronic lifestyle-related condition. Specifically, the risk for type 2 diabetes mellitus was reduced by 93%, myocardial infarction by 81%, stroke by 50%, and cancer by 36%. Even if not all four of these health factors were present, the risk for developing one or more chronic lifestyle-related conditions decreased commensurate with an increase in the number of positive lifestyle factors. Should a medication be found to have such potent benefits, it would be hailed as nothing short as miraculous.
The goal in health care is to exploit the benefits of lifestyle modification and supplement those benefits with medication only if necessary,71 rather than the other way around (supplementing medication with lifestyle modification). A healthy lifestyle is the treatment of choice for lifestyle-related conditions; it is also the primary intervention for their prevention.72 The translation of these research findings into health care practice is a priority.
Ischemic Heart Disease
The risk factors for IHD are well established.73 They contribute to atherosclerotic deposits not only throughout coronary vessels but throughout the systemic arterial vasculature.74 Nonmodifiable risk factors include age, sex, family history, and past history. Modifiable risk factors include increased cholesterol, increased homocysteine, smoking, inactivity, high blood pressure, diabetes, weight, and stress.75–77 Less commonly acknowledged risk factors include elevated C-reactive proteins (markers of inflammation37), sharing a lifestyle with someone who has IHD,78 and having overweight parents.79 Further, a shared lifestyle confers increased evidence of IHD in and health risk for children.80 Other emerging risk factors include passive smoking, level of education, depression, anger coupled with hostility, and social isolation.81,82
Based on epidemiological evidence, a 1% decrease in cholesterol reduces the risk for IHD by 3%, and a long-term reduction in diastolic blood pressure of 5 to 6 mm Hg reduces the risk by 20% to 25%.83 Thus even modest changes can have a sizable impact on health. Most risk factors are associated with behavior choices and can be substantially modified.84
Risk factors for IHD are prevalent in the general population. When a cross section of people in their later middle-age years was screened, atherosclerosis involving the femoral artery affected two-thirds of them.85 Further, a direct relationship existed between the degree of atherosclerosis and cardiovascular and general circulatory health. Individuals with peripheral artery disease have a several-fold increased risk for IHD; thus peripheral artery disease can be considered a marker of systemic atherosclerosis. It is estimated that optimal lifestyle could reduce cardiac events related to atherosclerosis by 70% to 80%. Regular walking has a significant effect on reducing the risk for IHD, as has vigorous activity.86 In men with left ventricular hypertrophy, moderate physical activity reduces the risk for stroke by 49% compared with sedentary men who do not have left ventricular hypertrophy.87 Type 2 diabetes mellitus has been reported to be a strong risk factor (and hypertension a less strong risk factor) for IHD in women when compared with men.88
Self-reported fitness has been reported to be independently related to fewer risk factors for IHD and angiographic evidence of IHD in women undergoing coronary angiography for suspected ischemia.89 Measures of obesity are not independently associated with these outcomes. Thus fitness appears to be more important than body weight for cardiovascular risk in women. Physical activity and fitness warrant detailed assessment. They should be an integral part of the cardiovascular risk-factor stratification, and interventions should aim at long-term increases in physical activity and fitness. Assessment of physical activity and exercise programs should be included in the management of all people, particularly in women and those at risk for IHD.
Mediterranean-type diets have been increasingly shown to have multiple health benefits and are superior to the North American diet in terms of food diversity and healthfulness. These diets are high in fish, fresh fruit and vegetables, and multigrains. Mediterranean-type diets are also low in added sugar and salt, and they favor unsaturated vegetable oil over saturated animal fats. When diet-related studies are evaluated, people who consume fish twice a week have a 47% reduced risk for cardiac mortality compared with those who eat fish less than once a month.90 Cereal fiber (two whole-grain slices of bread daily) is associated with a 14% reduced risk for myocardial infarction or stroke. Cereal fiber consumption even later in life is associated with a reduced incidence of cardiovascular disease.91 One alcoholic drink a day is associated with the least number of cerebrovascular abnormalities. Moderately and highly physically intense leisure-time activities predict 28% and 44% lower mortality rates, respectively, compared with little activity. Low, moderate, and high levels of exercise are associated with 30%, 37%, and 53% more years of healthy life, respectively. Aerobic training can reduce serum lipids even in older individuals; high-density lipoproteins increase and low-density lipoproteins decrease.92 With lifestyle change, atherosclerosis can regress and associated cardiac events can be minimized.93–96
Psychosocial factors have been identified as risk factors for IHD. Difficulty in managing anger and hostility is one such risk factor, regardless of whether a person has a type A or a type B personality.97 Stress is a risk factor that can be classified as minor daily hassles or as major negative events. Lipoprotein levels increase with both levels; however, coping style and subjective appraisal of stressors are powerful mitigating factors.98 Cumulative daily hassles may be underestimated in terms of their impact on health compared with major life stressors. After an individual’s first coronary event, avoidance strategies are inversely associated with healthy lifestyles, whereas positive reappraisal and problem solving are directly associated.99 Positive reappraisal and problem solving, program participation, rather than adopting distancing and escape strategies predict a person’s capacity to change lifestyle after a coronary episode. Stress management should consider the type of stressor and help to modify the individual’s coping strategies and interpretation of stressors.
The risk for a cardiac event after the first one is high.100,101 Thus there is a high prevalence of repeated revascularization procedures and the prescription of more drugs with increased potency to help offset worsening pathophysiological changes. Ornish102 reported that 194 individuals with previous revascularization procedures avoided repeat procedures for at least 3 years (the duration of follow-up in the study) when they participated in a comprehensive lifestyle-change program. Compared with individuals who also had had a previous revascularization procedure but did not participate in the lifestyle-change program, those who did participate reported a level of angina comparable to that experienced with revascularization. The effects of noninvasive intervention can be considered long term, given their multisystem benefits. Revascularization focuses on the repair of an impairment and does not provide the additional multisystem benefits of the lifestyle-change program.
To date, efforts to champion aggressive modification of risk factors have been modestly successful. Optimal control of modifiable risk factors for coronary atherosclerosis, including cigarette smoking, dyslipidemia, hypertension, and sedentary lifestyle are well known to reduce the incidence of IHD and, in turn, revascularization procedures and health care utilization.103 Our major health crisis can be addressed only by means of a system of care committed to health, wellness, aggressive risk-factor prevention, and lifestyle modification.
Smoking-Related Conditions
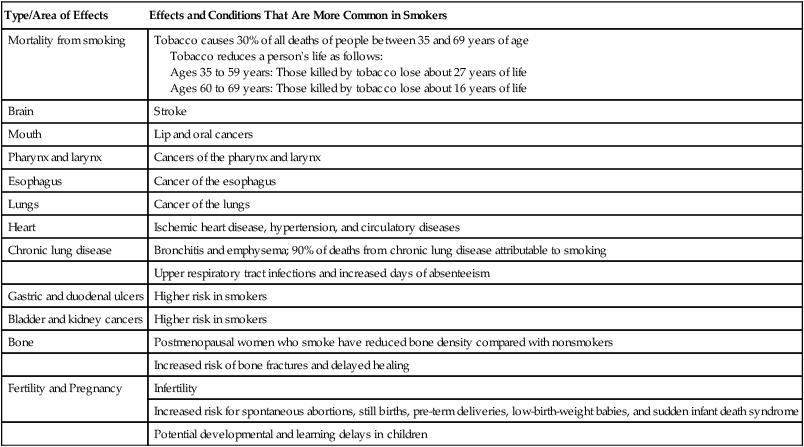
Smoking is the leading cause of preventable death in the United States, as well as the rest of the world.51 Despite the well-documented health hazards, smoking remains prevalent in industrialized and nonindustrialized countries and is estimated to shorten life by 11 minutes for each cigarette smoked.104 Thus smoking cessation is a primary health care goal, as well as a professional goal. (In 1996, the APTA adopted guidelines from the Agency for Health Care Policy and Research [AHCPR], which have subsequently been revised.105) The danger of smoking extends beyond COPD and cancer. Overall morbidity and all-cause mortality, including cancer of organs other than the respiratory tract, are higher in smokers.
Of the leading causes of mortality worldwide, COPD is typically among the top killers and is associated with the loss of a million years of life each year.106 In the United States, COPD ranks fourth behind IHD, cancer, and stroke. Long-term smokers have higher incidences of all-cause morbidity and mortality (Table 1-3); thus smoking leads to life-threatening conditions that are systemic and are related not just to the respiratory tract.90 Former and current smokers have 25% and 44% fewer healthy years of life, respectively, compared with lifelong nonsmokers. Smoking cessation is a priority for all individuals, not only those with lung disease, regardless of disease severity.107 Smoking by children is highly associated with parental smoking; thus smoking by adults with young families has become a primary focus of public health initiatives.79 Smoking is the single most important preventable cause of illness and death.
Table 1-3
Tobacco Facts and Multisystem Consequences of Smoking
| Type/Area of Effects | Effects and Conditions That Are More Common in Smokers |
| Mortality from smoking | Tobacco causes 30% of all deaths of people between 35 and 69 years of age Tobacco reduces a person’s life as follows: |
Data from National Cancer Institute: Cancer Facts, 2010; U.S. Department of Health and Human Services: The health consequences of smoking: a report of the Surgeon General, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2004; Peto R, Lopez AD, Boreham J, et al: Mortality from tobacco in developed countries: indirect estimation based on national vital statistics, Lancet 339:1268–1278, 1992; Twardella D, Kupper-Nybelen J, Rothenbacher D, et al: Short-term benefit of smoking cessation in patients with coronary artery disease: estimates based on self-reported smoking data and serum cotinine measurements, European Heart Journal 25:2101–2108, 2004.
Pulmonary rehabilitation has demonstrated sustainability of smoking cessation and other health benefits in individuals with COPD;108 thus its use is warranted as a preventive measure, as well as for the remediation and management of disease.109 Rehabilitation programs have proven efficacy, independent of pharmacotherapy, so they should be considered primary interventions rather than priorities after conventional expensive medical care has failed.110 Only with health coaching and follow-up can these individuals effect lifelong health behavior change to minimize exacerbations, reduce doctor and hospital visits, continue working, and reduce overall morbidity. Innovative smoking cessation programs warrant development so that they have maximal impact in the most significant window of opportunity and stage of readiness of a smoker to quit. One such program consisted of 5 weeks of counseling.111 The mean time to deliver the intervention was 44 minutes. At 1 month, 70% of participants had continued to abstain. The mean cost of the intervention was approximately $50 for each person.
Smoking cessation is the most cost-effective intervention for smokers with heart disease in terms of health protection and risk reduction. Further, treatment of hyperlipidemia and referral to cardiac rehabilitation are highly cost-effective per quality-adjusted life-year and are relatively cost-effective per year of life saved. Smoking is an established risk factor for ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage,112 as well as for IHD. The risk is directly proportional to the amount smoked. Risk factor detection and management are the cornerstones of high-impact and high-quality care of cardiovascular disease.
Hypertension and Stroke
Stroke is a preventable tragedy for nearly 750,000 people in the United States annually; hypertension is the most common risk factor.113 Although lowering blood pressure below 130/85 mm Hg is well accepted across ages, the success of blood pressure control has been reported to be less than 25% in the hypertensive population.114 Stroke risk is far from being well controlled despite considerable understanding of its causes, and it remains a major health threat. Risk factors for stroke include previous stroke, hypertension, IHD, atrial fibrillation, hyperlipidemia, diabetes, abnormal ankle-to-brachial pressure index, reduced exercise endurance, retinopathy, albuminuria, autonomic neuropathy, smoking, alcohol consumption, and lack of exercise.113,115–119
Risk factors for hypertension and stroke can be accentuated by smoking, elevated cholesterol, glucose intolerance, inactivity, and obesity.120 In addition to stroke, serious consequences of hypertension include hypertension heart disease and renal disease. Implicated as a cause of stroke is increased sympathetic reactivity.121
In the adult population between 60 and 74 years of age, almost 75% of African Americans and 50% of Caucasians have high blood pressure.122 As with IHD, risk factors for high blood pressure consist of nonmodifiable and modifiable risk factors. Nonmodifiable risk factors include age, sex, race, and other genetic factors. Modifiable risk factors include diets high in sodium and low in potassium, alcohol consumption, reduced physical activity, and being overweight.123 Obesity is a strong predictor of hypertension.124 Although significant reduction of hypertension has been attributed to low-dose thiazide diuretics and beta blockers, the first line of defense to prevent high blood pressure and normalize blood pressure should be nutritional approaches, weight reduction, and regular physical activity and exercise.125 In individuals whose hypertension is controlled, the combination of a Mediterranean diet and physical activity can reduce health risk substantially.126 Like other lifestyle-related conditions, hypertension is increasingly common in American children; thus screening should be included in routine pediatric assessments.127
With respect to nutrition, high sodium and low potassium have been implicated in hypertension and stroke, as have lipids. The National Academy of Science has recently announced that reducing added salt by as little as one-third would reduce hypertension in the United States by 25% (11 million fewer cases). Low plasma vitamin C is associated with a several-fold increased risk for stroke, particularly in men who are overweight and hypertensive.128 A minimal reduction in diastolic blood pressure (5 to 6 mm Hg) reduces the risk for stroke by 35% to 40%.83 Thus weight control; regular exercise; a diet rich in fruits, vegetables, and whole-grain cereals; smoking cessation; and blood pressure control are central to stroke prevention, as well as to the comprehensive management of stroke.
Although weight reduction is an essential component of hypertension prevention and management, the protective effect of physical activity may be unrelated to the degree of obesity.129 A 4% to 8% reduction in body weight can reduce blood pressure by 3 mm Hg, and physical activity can reduce blood pressure by 5/3 mm Hg.130
In normotensive African American men, aerobic exercise can attenuate an exaggerated blood pressure response.131 Similarly, normotensive fit African American women have blunted blood pressure responses to experimental stressors.132 One study reported no relationship between physical activity and hypertension, flow-mediated dilation of the brachial artery, or an index of angiogenesis assessed with plasma vascular endothelial growth factor (the latter two being indicators of endothelial dysfunction).133 In this study, however, physical activity was based on self-report in a questionnaire rather than on fitness outcomes, so the results of the study are difficult to interpret.
Physical activity and optimal nutrition can reduce the risk for early atherosclerosis, a precursor to stroke, in lifelong nonsmokers.134 Smokers benefit less from this protective effect. Physical activity seems not only to reduce the risk for stroke but also to provide a potent prophylactic strategy for increasing blood flow and reducing brain injury during cerebral ischemia.135 A possible mechanism is augmented endothelium-dependent vasodilation via up-regulation of endothelial nitric oxide synthase throughout the vasculature. Aerobic exercise three times a week reduces cerebral infarct size and functional deficits in a mouse model and improves endothelium-dependent vasorelaxation.135
Assessment of risk for hypertension is an important component of each patient’s assessment. The management strategy should be based on an analysis of the overall risk assessment rather than on blood pressure alone. The prevention of hypertension requires more than normalizing blood pressure if the deadly manifestations of high blood pressure including IHD are to be avoided. Because of the dire consequences of hypertension, the American Heart Association advocates stringent blood pressure limits—specifically, below 130/85 mm Hg, regardless of age.136 Recommendations by the American Heart Association concerning physical activity and exercise guidelines for survivors of stroke concur that physical conditioning is a primary goal in these individuals, who must contend with both the pathological effects of stroke and the effects of deconditioning.137 Walking as little as 2 hours a week can reduce the risk for stroke by 50%.130 Improved conditioning may help to reduce limitations of activity and participation and hence improve quality of life. The burden of disease and disability and their risk factors may be correspondingly reduced.
To affect the health of the population, stroke prevention depends on the dissemination of these well-established and widely available interventions to a large number of people through public health policy. Advice given by a health provider to individuals with stroke for the purpose of prevention of a second stroke can have significant impact. In one study, individuals were simply advised to eat fewer high-fat and high-cholesterol foods and to exercise more.138 Compared with a control group that received no advice, those receiving advice reported fewer days with limited activity, fewer days that “were not good physically,” and more “healthy” days. The results of this study are compelling in that even simple advice by a health care provider can have a major impact on important health behaviors and on potential health outcomes.
Type 2 Diabetes Mellitus and Metabolic Syndrome
Type 2 diabetes mellitus is a serious multisystem condition that has rapidly become pandemic in Western countries and some other countries where its incidence was previously minimal. In addition to the serious physical and functional consequences of this condition, perceived health status and quality of life are also compromised.139 By 2010, an estimated 250 million people will be affected worldwide.140 Formerly known as adult-onset diabetes, type 2 diabetes mellitus is now being diagnosed in children, predisposing them to blindness, IHD, stroke, renal disease, peripheral neuropathies, vascular insufficiency, and amputations.141,142 Inositol acts as a poison on the membranes of cells in the presence of high blood sugar, and it has been implicated in the deadly systemic consequences of diabetes. The primary consequences include pathological changes to the macro- and microvasculature and to the nerve endings. Impaired glucose tolerance is a marker of vascular complications in the large and small blood vessels, independent of an individual’s progression to diabetes. Early detection of glucose intolerance allows intensive dietary and exercise modifications, which have been shown to be more effective than drug therapy in normalizing postprandial glucose and inhibiting progression to diabetes.143 Diabetic autonomic neuropathy as an independent risk factor for stroke may reflect increased vascular damage and effect on the regulation of cerebral blood flow in individuals with diabetes.115
Individuals with type 2 diabetes mellitus have increased risk for cardiovascular disease compared with individuals without diabetes, so strict control is essential. Moderate physical activity (such as brisk walking144) along with weight loss is a powerful combination to reduce the risk for type 2 diabetes mellitus, as well as to reverse it. These interventions combined with a balanced diet can reduce the risk for developing diabetes among those who are at high risk by 50% to 60%.86 Cigarette smoking is an independent risk factor for type 2 diabetes mellitus145 and is particularly dangerous for individuals who already have diabetes.141
Metabolic syndrome refers to a virulent and lethal group of atherosclerotic risk factors, including dyslipidemia, obesity, hypertension, and insulin resistance, and it affects some 47 million people in the United States.146 The incidence of the syndrome is increasing and warrants aggressive noninvasive management. Insulin sensitivity is predicted primarily by body mass index, smoking, age, and daily physical activity. Weight reduction counters the effects of metabolic syndrome and may counter the associated hypertension and dyslipidemia as well. Diet and exercise are primary components of the multifactorial approach to preventing and managing this lethal condition.
Obesity
Obesity has been increasing exponentially over recent decades; currently, 61% of the American population is overweight.147 Obesity is becoming a global pandemic that rivals malnutrition as a health priority in some low-income countries,148 and it contributes to health risks for all lifestyle-related conditions. The complications and risks for which each patient should be assessed include IHD, cardiac myopathy, and chronic heart and lung dysfunction; hypertension and stroke; some cancers; insulin insensitivity and type 2 diabetes mellitus; gallbladder disease; dyslipidemia; osteoarthritis and gout; and pulmonary conditions, including alveolar hypoventilation and sleep apnea.149–153 With each kilogram of weight above normal, the risk for hypertension, IHD, and type 2 diabetes mellitus increases proportionately. Obesity is commonly linked with insulin resistance and high blood pressure, which may reflect reduced activity and exercise. Reduced physical activity is a predictor of obesity.154 Insulin resistance associated with lack of exercise in people who are overweight may be further compounded by insulin resistance associated with chronic inflammation observed in fat cells.155 Abdominal obesity, lipid metabolism, and insulin resistance are interrelated markers for coronary artery disease.156 In addition to cardiovascular and general health risk, being overweight affects quality of life.157,158
Comprehensive management of an individual who is overweight and has abnormal blood glucose levels includes normalizing blood glucose (with recommendations for low-glycemic foods and small, frequent snacks rather than infrequent large meals), weight reduction, restricted intake of trans fats and saturated fats, strict blood pressure and lipid control, regular physical activity and exercise, and avoidance of tobacco.159
Nutritional habits during childhood are associated with lifestyle-related conditions in adulthood.160 Obesity in children is associated with parental obesity.79 Maintaining weight within a healthy body mass index range throughout life is recommended for optimal health. Although body mass index may be limited with respect to assessing adiposity because it fails to discriminate between muscle and fat and identify regional adipose depositions, it remains a useful supplementary clinical index.161 Physical therapy has a primary role in preventing and managing overweight and obesity in every client or patient, regardless of age, given obesity’s serious multisystem consequences, psychosocial sequelae, and threat to life participation and satisfaction.162
Cancer
Cancers associated with the highest mortality rates include lung, colorectal, and pancreatic cancer.163 Smoking has been implicated as a risk factor for many cancers, not only those involving the respiratory tract. The role of lifestyle factors in cancer remission has not been studied in detail.
Cancer prevention and rehabilitation have become a specialty area, requiring an integrated knowledge of pathophysiology, psychosocial implications, and management interventions.164,165 Routine assessment of health behaviors and risk factors and healthy living recommendations may help avert the diagnosis of many cancers or mitigate their effects. To date, evidence that walking is an effective strategy to prevent cancer has been best established for colon cancer,86 although breast cancer and prostate cancer have also been reported to be positively affected by regular aerobic exercise including walking.166,167
Musculoskeletal Health
Osteoporosis and arthritis contribute to considerable morbidity and secondarily to mortality. Because both of these conditions have lifestyle components, a lifestyle risk factor review should be included in every initial assessment to establish a baseline of musculoskeletal health. Moderate levels of physical activity, including walking, are associated with a substantially lower risk for hip fractures in postmenopausal women.168 Thus assessment of both nonmodifiable and modifiable risks is a major component of the health assessment as a means of minimizing morbidity and potential mortality.9 Osteoporosis and associated morbidity, particularly in older age groups, is a serious health issue that warrants monitoring. Establishing baseline information on bone health in every patient is prudent, given the relationship between bone health and lifestyle behaviors (e.g., activity and nutrition—smoking and heavy consumption of meat, alcohol, and coffee). Although older, postmenopausal women have been the focus of bone health studies, other groups are also at risk for osteoporosis and should not be overlooked: older men; inactive children, particularly girls; and individuals with chronic conditions who may be less able to undertake weight-bearing activities and physical activity. In a study of the development of bone mass and strength in girls and young women, only exercise (not daily calcium intake) was associated with bone density and strength.169 This finding stresses the singular importance of bone building in young people to help offset osteoporosis later in life and associated decrement in quality of life.
Psychological Health
Mental health problems and depression are prevalent in Western society despite its affluence. Based on one descriptive study, individuals with mental health conditions such as schizophrenia tend to have poor physical health and die prematurely from cardiovascular disease.170 Compared with women who have schizophrenia, men with the condition consumed less fruit, vegetables, whole grains, and rice than recommended. Further, the incidence of smoking and obesity in both sexes was higher than in the general population. Cholesterol levels were high and activity levels low. This study suggested cause for concern about both the physical and psychological well-being of individuals with mental health conditions and indicated the need for further investigation of the physical health and well-being of people with mental challenges.
Dementia and Alzheimer disease appear to be increasing. Aging has been countered as a primary argument for this trend in favor of lifestyle-related influences including nutrition, specifically, processed meat consumption. Recently, Alzheimer disease has been associated with the consumption of meat from animals that have been fed nonnatural foods. This has been thought to lead to misfolding of DNA, thus affecting cognitive function in people who have consumed such products over many years.171 Other factors that have been associated with the condition include decreased cerebral blood flow.172 Understanding the vascular component of this condition along with food-related explanations will be an important advance in its prevention and management. In a cohort of older African Caribbean individuals, vascular risk has been associated with cognitive impairment and physical activity is inversely related to impaired cognition.173 Exercise training has been reported to improve physical health and depression in individuals with Alzheimer disease.174 Whether this reflects a vascular component of the pathogenesis of the disease that is offset by exercise warrants elucidation.
Dental Health
Periodontitis, characterized by low-grade infection of the gums, is widespread and may be associated with serious systemic health problems. In a study of 39,461 men, periodontitis risk decreased with increased physical activity, independent of such risk factors as age, smoking, diabetes, body mass index, alcohol consumption, and total calories.175 Inactivity and the typical Western diet have been described as proinflammatory. Whether the benefits of a physically active lifestyle and an optimal diet can extend to dental health warrants investigation.
Promoting Healthy Living: The Contemporary Physical Therapist’s Role
Assessment of health behaviors and recommendations for healthy living can be put into practice in every patient interaction176 and, in turn, help reduce the population’s health risk and mitigate the economic cost of lifestyle-related conditions.177 Increased consumption of meat, fat, and sugar has contributed to the increased prevalence of lifestyle-related conditions in low- and middle-income countries, as well as in high-income countries.178 An associated increase in the prevalence of insulin-resistance syndromes is further increasing the incidence of cardiovascular disease.179 Anthropologists have argued that food abundance and inactivity may be altering evolutionary processes and that these factors contribute to the current pandemic of chronic conditions.180 Attitudes toward factors contributing to lifestyle-related conditions reflect the values and behaviors of society. Optimal control will be achieved only with widespread public health policy, social action involving health care providers, and an increase in individual responsibility.
Why Physical Therapists Need to Understand and Advocate Optimal Nutrition
Given that an association has been established between diet and chronic lifestyle-related conditions, the question of what is the optimal nutritional regimen for humans has been widely debated. Of note is that the anatomic structure and physiological (endocrine) function of humans are consistent with an organism designed for a largely plant-based diet—that is, having hands rather than claws, a particular tooth type and skin type, salivary glands, acidity in the saliva, ptyalin in the saliva, a specific level of hydrochloric acid in the stomach, and an intestinal tract of a certain length.181
Cultures that consume a diet based primarily on plants tend to have superior health outcomes. The diets of octogenarians in Asia and of centenarians in general tend to be high in fiber and low in saturated and trans fats, refined sugar, and salt compared with the typical diet of Western people.182 The Mediterranean diet, which includes plentiful fruits, vegetables, fish, and vegetable oil, has shown health benefits and is associated with lower incidence of chronic disability and premature death compared with the typical Western diet.87,126 Cultures in the Mediterranean region also tend to have higher activity levels, which influences metabolism and physiological responses to food.
Weight-loss diets are a multibillion-dollar industry in Western cultures. Many of these diets are unsubstantiated or may theoretically work but are not well balanced in terms of the macro- and micronutrients needed daily for optimal health. Low-carbohydrate diets have been popular, but weight loss associated with these diets results from calorie restriction and the duration of the diet rather than from a reduction in carbohydrate consumption.183 Weight control is achieved by the balance between optimal caloric and nutrient content consumed and optimal energy expenditure. Given the pandemic of obesity in industrialized countries, physical therapists need to understand the normal physiological adaptations to poor food choices and sedentary lifestyles—weight distribution, endocrine changes, cardiovascular and pulmonary changes, and musculoskeletal changes—in order to prescribe the best lifelong management programs.
Overweight and obesity constitute a life-threatening pandemic that warrants management before the manifestation of one or more of its life-threatening consequences, in addition to its associated psychosocial and economic consequences. Along with obesity, glucose intolerance may complicate the picture, or the patient may have subclinical intolerance. Central adiposity, in particular, has been associated with a high incidence of insulin resistance, which may explain the high rates of dyslipidemia, hypertension, and type 2 diabetes mellitus in these individuals.184 Thus the physical therapist has a primary role in basic nutrition counseling, commensurate with the promotion of optimal health, and in providing information about nutrition (related to exercise energetics and glucose control) to support a prescribed dosage of regular exercise and physical activity. A nutritionist may need to be consulted to provide nutrition counseling beyond fundamental needs, especially in complicated cases.
Nutrition guidelines have been revised by the U.S. Department of Health and Human Services185 and Health Canada.186 Compared with previous versions, the revisions appear to be better aligned with the literature than with the interests of lobby groups from the food industry and producers of so-called nutritional supplements. Some authorities have argued that the current pandemic of lifestyle-related conditions reflects adherence to guidelines over which food-industry lobbyists had influence, rather than lack of adherence by consumers. Current consumption of fats, refined foods, and vegetables in North America, for example, has failed to meet the recommended revised guidelines. Diets high in salt, saturated fat, and refined foods, and low in servings of vegetables and fruit have been implicated in lifestyle-related conditions.
The revised guidelines are more evidence based and have been designed to optimize health and reduce the risk for chronic conditions. Earlier guidelines fell short with respect to this objective. Adherence to established dietary guidelines for Americans as assessed by the healthy eating index was only weakly associated with risk for major chronic conditions in men187 and was not associated at all with risk for major chronic conditions in women.188 Thus dietary guidelines and the healthy eating index require refining to achieve more favorable outcomes and to allow them to be assessed.
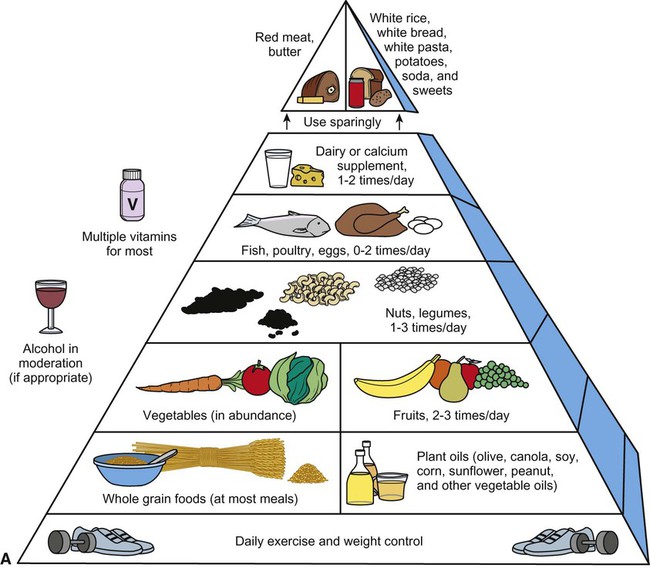
An optimal food pyramid, on which the revised nutrition guidelines are based, is shown in Figure 1-2, A. The pyramid illustrates general guidelines for maximizing health in the general public, and these guidelines have been shown to offset lifestyle-related conditions.189 Each individual’s diet should conform with these guidelines for optimal lifelong health. The nutrition food pyramid emphasizes abundant servings of vegetables at the base; followed by vegetable or lean-meat protein sources and dairy; beans, lentils, and whole grains; and low-glycemic foods. Red meat and eggs, positioned at the top of the pyramid, are to be consumed most sparingly. The typical Western diet is short on vegetables, fruits, and fiber (particularly insoluble fiber)190–192 and includes excess salt, sugar, highly refined foods, and saturated and trans fats.193 Diets high in grain-based foods are associated with reduced cardiovascular risk, independent of other behaviors.193,194 The food pyramid has recently been revised as a plate icon where 2-3 servings of vegetables cover half the plate, a quarter carbohydrates (multigrains) and the remaining quarter vegetable protein or animal protein Figure1-2, B. Unless a person has an objectively identified deficit, there is no evidence that nutrient supplementation adds benefit to a daily nutritious diet.
Attention to nutrition is important not only in relation to body weight. Cholesterol and triglycerides are risk factors for IHD.195 To address this major health threat, lipid-lowering drugs have glutted the pharmaceutical market and one-stop coronary cholesterol clinics have been advertised. However, a cardioprotective diet, which has been well described in the literature, should be the goal, in conjunction with lipid-lowering agents in selected cases. Even when medications are used, weaning individuals off them as lipids and cholesterol are lowered by noninvasive means is an important goal of physical therapy, in conjunction with a lifelong program of exercise, good nutrition, no smoking, moderate alcohol consumption, and stress management.
With respect to body mass, risk factors increase as body mass increases beyond a healthy range. Studies recommend that a healthy waist girth (low risk) is <84 cm (33 in) for women and <89 cm (35 in) for men.196 Further, waist-to-hip ratio has been shown to be a better predictor of myocardial risk than body weight alone.197 Thus measures of height and weight to calculate body mass index, as well as waist and hip girth, are simple standardized assessment tools and outcomes that can be used diagnostically and as tools to evaluate response to interventions such as dietary education and exercise to achieve optimal weight.
Finally, Western diets have excessive salt content—hence the pandemic of hypertension. Measures need to be taken to legislate the salt added in food production and processing. An overriding simple solution at the individual level is restricting added salt to foods. A one-third reduction of salt intake by the average American (from 3400 mg to 2300 mg daily) would reduce cases of hypertension (the second-leading cause of death in the United States), by 11 million and would lower health care costs by $17.8 billion.198
Why Physical Therapists Need to Understand Exercise in the Context of Population Health
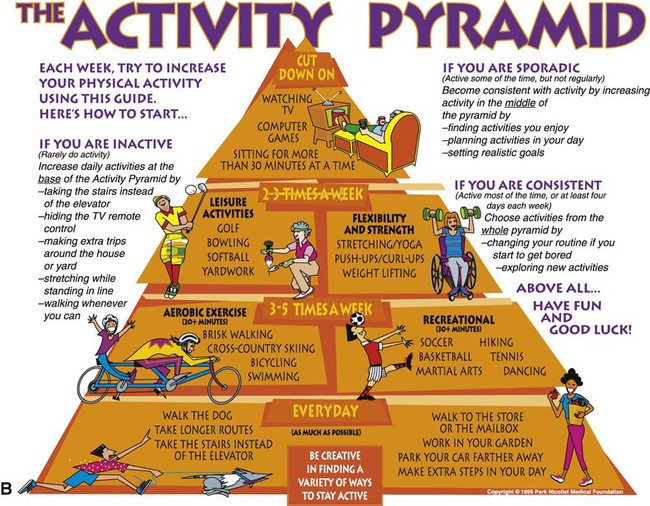
The physical activity and exercise pyramid is illustrated in Figure 1-2, B. This pyramid shows a physically active lifestyle at the base, followed by aerobic exercise three to five times a week, followed by strengthening exercise and flexibility, with rest and inactivity at the top.
Sedentary behavior has been a recent focus of study with the recognition that reducing sedentary behavior is not necessarily synonymous with increasing physical activity. The literature supports that prolonged periods of being sedentary are associated with greater health risk than multiple short periods of sedentary behavior (i.e., breaks in sedentary time).199,200 Sedentary activity is common today; people often sit for long periods in front of a television or computer, and children and adolescents are increasingly consumed with screen-based activities. Recommendations for breaks in sedentary behavior are complementary to those for increasing physical activity. Sedentary behavior in early childhood is associated with such behavior in adolescence and adulthood.201 Encouraging physical activity in adults and children regularly throughout the day requires not only individualized education about exercise, but structuring neighborhoods, transportation systems, recreational facilities, homes, and workplaces that are health promoting.
The physical activity pyramid, like the food pyramid, is a reminder of the importance of lifestyle choices for optimal health.202 Generally, walking 10,000 steps a day is consistent with an active lifestyle and good health in an adult,203 whereas fewer than 5000 steps a day would be considered a sedentary lifestyle. Walking 7500 to 9999 steps a day is consistent with a somewhat active lifestyle, and more than 12,500 steps a day would be consistent with a highly active lifestyle.
With increased physical activity, the risks for IHD, stroke, and colon cancer are reduced. The precise dosage-response relationships between physical activity and health and between physical fitness and health have yet to be clarified and may differ among people.204 Moderate physical activity, which does not have to be strenuous or prolonged, includes leisure activities such as walking and gardening and is associated with marked health benefits.145 Even light to moderate physical activity in middle and old age confers marked benefit to cardiovascular health and is protective against all-cause mortality.205 The U.S. Surgeon General recommends 30 minutes of moderately intense exercise on most days, with an accumulated duration of 180 minutes a week.206
Exercise has a profound effect on the endothelial function of blood, which has been implicated in atherosclerosis, IHD, cerebrovascular disease, and gastrointestinal conditions, and could explain exercise’s multisystem benefits. Moderate levels of physical activity reduce the risk for stroke, independent of other factors.207 In addition to dietary habits, reduced physical activity has been implicated in most lifestyle-related conditions including osteoporosis, and exercise is recognized as an essential component in the primary prevention of these conditions. Even mild physical activity has an important role in the primary prevention of type 2 diabetes mellitus through its direct effect on increased tissue sensitivity to insulin.208 Nonpharmacological interventions for preventing and managing hypertension have been strongly advocated to maximize their therapeutic benefit and minimize the risks associated with medications.209 Furthermore, in older people, regular physical activity has an important role in preventing chronic conditions and prolonged end-of-life suffering.210
Why Physical Therapists Should Promote Smoking Cessation
Smoking is the leading cause of premature death. It results in premature death and higher rates of all-cause death.50 Although Caucasian Americans have a higher rate of smoking than do African Americans, African Americans and women who smoke have respiratory problems at a younger age, despite having started smoking later and having a lower overall pack-year smoking history.211 Men with a strong intention to quit have been reported to have a more favorable attitude toward quitting and a stronger sense of perceived control than those with a less strong intention to quit. In addition, men who have a strong intention to quit smoking have greater success.212 With a view to promoting lifelong health, advocating smoking reduction and cessation is an important responsibility of the physical therapist regardless of the patient’s problems.
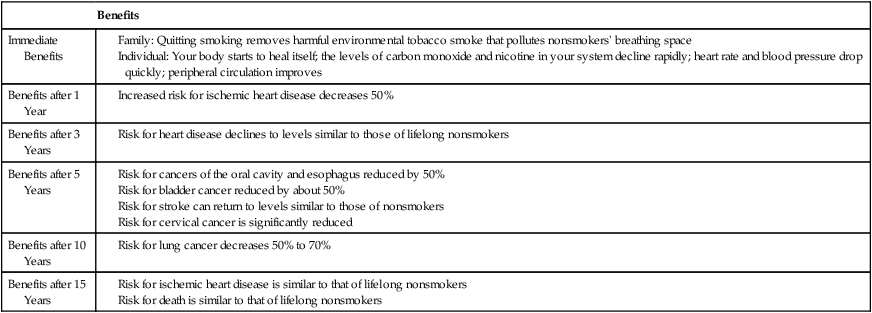
Over time, smoking cessation can reverse many of the lethal effects of smoking (Table 1-4; also see Table 1-3). For smokers unable to quit, advocating “competing” health strategies has been proposed.213 Improved diets and increased physical activity and exercise, however, do not counter the negative effects of smoking.134
Table 1-4
Health Benefits of Quitting Smoking
Data from the American Cancer Society, 2004; U.S. Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2004; American Lung Association. www.lungusa.org/site/pp.asp?c=dvLUK9O0E&b=22938; Manson JE, Tosteson H, Ridker PM, et al: The primary prevention of myocardial infarction, New England Journal of Medicine 326:1406–1416, 1992.
Why Physical Therapists Need to Understand Ethnic and Cultural Differences
Industrialized countries are becoming increasingly ethnically and culturally diverse as people migrate around the globe, particularly to high-income countries where lifestyle-related conditions are prevalent. With birth rates on the decline in these countries, immigration is being encouraged. Thus it is important to understand the role and impact of ethnicity and culture as important factors influencing health, ill health, use of health care services, the types of health education that are needed, and the ways in which they should be disseminated.214
The prevalence of COPD and its associated mortality increase with age, rates being higher in Caucasians than in other ethnic groups in North America.211 Among people with advanced COPD, however, African Americans and women are more prone than other groups to the adverse effects of tobacco. Cardiovascular disease in Mexican Americans and Native Americans is a particular concern and has implications for optimal care and service delivery.54,215,216 Obesity, hypertension, and metabolic syndrome are also more prevalent in these groups, so their special needs should be recognized by physical therapists. Currently, Eastern Europe, the Middle East, and Asia have the highest smoking prevalence in the world.
The health advantages that people of other cultures enjoy in their homelands (Asians, for example) are compromised when they immigrate to Western countries and adopt Western dietary and exercise habits.67,217,218 Although they may benefit from improved health services and access, lifestyle-related conditions exact more of a toll on new immigrants with each passing year. The physical therapist has a unique role as health educator in promoting optimal lifestyle practices in new immigrants, as well as in long-term residents.
People from Utah, 72% of whom are Mormon by faith and follow a strict lifestyle code, have among the best health indexes in the country and some of the lowest rates of chronic disease,57 but ethnic minorities in Utah are at increased risk for heart disease and stroke, among other conditions. Designing preventive and management strategies requires responding to the needs of different groups. A training program designed specifically for African Americans with stroke and complex comorbidities can be highly effective in improving fitness and reducing risk for further disease and disability.219 Racial differences have been documented with respect to the interactions of obesity, hypertension, and diabetes between African American and European American women.220 Greater emphasis needs to be placed on targeting risk factors in various ethnic and cultural groups. For example, alcohol consumption in Caucasian Americans and weight control in African Americans and Caribbean groups are among the targeted priorities.221 For each individual, the severity of the problem, the risks, and the willingness to change needs to be assessed to effectively target management strategies. Sensitivity to cultural, as well as to individual, differences when designing health-education strategies is essential to the long-term success of the intervention.
Cultural differences in self-reports of body functioning have been reported.222 These differences, along with low education status, are thought to explain the overrating of functional status in self-reports as compared with objective measures of performance. These observations support the need for greater cultural sensitivity and awareness in the clinic, particularly when the patient belongs to a minority group and the physical therapist is part of the dominant Caucasian American group. These findings support the need for objective functional assessment in addition to self-reported functional status.
Another important cultural factor in health care is the reporting of exertion, discomfort, and pain, which affect activity and participation. Studies have examined the expression of pain and the responses of health care providers to the pain expressed by people from cultures different from those of the health care provider. In addition to cultural differences in pain expression, patients from cultures that are highly expressive in expressing discomfort and pain have been reported to receive less medication and fewer pain control interventions than individuals who are less expressive, a characteristic consistent with the dominant culture.223,224
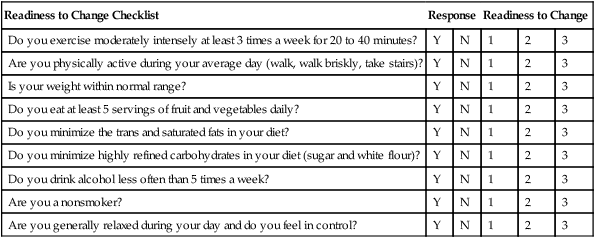
Physical Therapists as Drivers of Change in Health Behaviors
Based on the discordance between the extant knowledge of lifestyle-related conditions and health-promoting lifestyles, health care has failed to significantly reduce the prevalence of these diseases and their risk factors. The issue of why people do not always make appropriate lifestyle choices is of central importance to their health and to the practice of the health care provider. Patients may be more inclined to make follow-up visits to their health care providers than to change their lifestyles.225 One explanation for the failure of conventional models of health education226–232 is that traditionally they have been based on a unidirectional model of information delivery—that is, from the health care provider (a dominant person) to the individual or patient (a subordinate person) in the form of brochures, books, videos, magazine articles, and television and radio announcements. These formats typically are not well targeted to a specific demographic or to the needs of the learner. Smoking cessation programs, for example, have been reported to be more effective when targeted to the specific needs of middle-aged men, including resources that promote a perceived sense of control over health behavior.233 Changes in behavior are effected most successfully in a personal, bidirectional model, including rapport building, trust, commitment, and follow-up. Other important factors include receptivity, susceptibility, beliefs, timing, message delivery, barriers, reinforcers, and external stimulus-control factors.234 Such a strategy is the so-called AIM approach: Assess the learner, Identify barriers to learning, and Motivate the individual to make change.235
Cardiovascular disease is the leading cause of death in women, particularly those over 60 years of age. This cohort of women believes they are at low risk for heart attack, yet 82% of coronary events in women are explained by the absence of a low-risk lifestyle.236 Although women may respond favorably to risk-reduction initiatives, their awareness of risk factors and prevention strategies may be poor.237 When health information (with respect to a low-fat plant-based diet, exercise, smoking cessation, and stress management) is delivered in a supportive group environment, in innovative multiple formats (e.g., a retreat and group meetings), people make sustainable lifestyle changes that reduce health-risk factors, decrease the need for medication, and improve their quality of life.238,239 Furthermore, health education is more effective when cultural differences that affect health beliefs, attitudes, and behaviors are considered.240–242
Understanding poor adherence to health behavior change is as important as understanding the factors contributing to good adherence. In healthy middle-aged men at risk for IHD, for example, poor adherence to the recommendation to increase dietary fiber is related to smoking, hostility, perception of barriers to diet change, and poor knowledge of risk factors.243 Poor adherence to following a low-fat diet is related to smoking, young age, and having no family members or friends with IHD. Poor adherence to an exercise program is associated with young age and having young children at home. Such information for various target groups is important in planning effective health-education interventions. The results of studies, however, are based on group outcomes. Individual assessments are needed to determine the barriers to and facilitators of learning for each person. The physical therapist needs to anticipate that these may change for an individual over time.
Education is a common component of the management of every patient with the exception of those who are unconscious, severely mentally challenged, or cognitively incapable of responding to the information. Even in these cases, education of the attending health care providers and caregivers can be the priority. The success of health education reflects the individual’s expectations.244 Most physical therapists and other health care providers have little background in assessing expectations. Physical therapists would benefit from formal education in assessing the learners’ needs and wants, expectations, and readiness to learn and implement positive changes in their behaviors. Varying expectations may be particularly important when the patient is from a culture different from that of the physical therapist.
Various theories have been proposed to explain people’s health choices and to promote improved choices. One such theory is that of reasoned action or planned behavior.245 Based on this theory, an individual’s decision to engage in a healthy behavior such as exercise is based on his or her intention. Intention is a function of the person’s attitudes, perceived control and self-efficacy, and social factors. The elements of the McEwen model of health motivation are comparable and have been used, for example, to effect positive lifestyle changes in individuals participating in cardiac rehabilitation.246 The assessment includes the individual’s current knowledge, perceived severity, perceived susceptibility, perceived value of action, background variables, internal and external aids and hindrances, and the catalyst factors. Understanding the factors that affect an individual’s lifestyle choices is vital for targeting health education so as to produce sustained outcomes.
The transtheoretical model of “readiness to change behavior”247 outlines several behavioral-change stages, including precontemplative, contemplative, preparation, action, and maintenance. In designing health promotion education programs, this model helps to identify the stage of readiness to change, so that interventions can be tailored to and timed with an individual’s readiness to interact with the information, thereby enhancing outcomes. The five stages of change are shown in Box 1-1. Key questions can be asked to establish an individual’s stage of readiness to change (Box 1-2).
A study of change in exercise behavior employing the transtheoretical model in sedentary women compared psychological variables and the capacity for a moderate or vigorous exercise program, either at home or at a center, to effect change in their exercise habits over 18 months.248 Self-efficacy for exercise competence increased as women moved from the contemplative to the action stage and was particularly marked in the groups involved in vigorous exercise. Almost half of the women shifted from the action stage to the maintenance stage. The intervention was effective regardless of the setting and the intensity of the exercise program.
When patients are in the preparation and action stages, the physical therapist can teach a range of self-monitoring skills and recording strategies along with information about circulatory and heart conditions, risk factors, and prevention. Blood pressure self-monitoring can be taught, provided the equipment is calibrated and checked by the physical therapist, standardized procedures are used, and the patient’s measurement proficiency is evaluated.249
Psychological principles, including cognitive and behavior-modification strategies, are central to behavior change; they include the stimulus environment and events before the behavior, the reinforcement of the behavior, and consequent events.250 Shaping, feedback, and reinforcement schedules are powerful strategies. Complex behaviors such as lifestyle behaviors may be shaped by the introduction of small, progressive, easily achievable steps toward a larger goal, a process comparable to the integrated stepwise approach used to improve dietary habits.96 These principles can be incorporated into a model of lifestyle modification that incorporates factors such as culture.234,250
Education and effecting change in health behaviors are perhaps the most important components of the physical therapist’s expertise because such change dramatically affects the lifelong health of each individual patient. Preventive health messages stated by a health care provider can be powerful, and they are a strong predictor of change in health behaviors.230,251–253 However, preventive health messages are delivered to a relatively small number of patients by their health care providers. Thus lifestyle recommendations should be delivered as a holistic management priority to every patient, in a structured, conscious manner comparable to the rigor and precision of a prescribed treatment program. The cumulative time the physical therapist spends with each patient over days, weeks, and years translates into numerous teachable moments. Multiplying this time spent annually in teachable moments by the number of physical therapists in the world indicates that the potential for having a societal impact and making a global assault on lifestyle-related conditions is enormous.
Sending a patient home with a brochure on exercise or telling a patient not to smoke has a low probability of producing lasting results—or any results at all. The educational needs of the patient, in terms of receptivity to new information and to the styles of teaching and learning that are being used, need to be established; otherwise, both the clinician and the patient are wasting their time. Educational needs are multifactorial; they include health beliefs, self-efficacy, readiness to change, and motivation. The transtheoretical model247 of readiness to change (see Boxes 1-1 and 1-2) is valuable in demonstrating how to determine the patient’s stage through appropriate questions and how to devise strategies for moving a patient from one stage to the next in a progression toward preparation, action, and maintenance. Self-efficacy is an important determinant of readiness to change and of one’s capacity to effect and maintain a behavioral change.254 If the stage of readiness to change is considered when promoting healthy lifestyles, health coaching can be successful even if brief.255 The level of importance a person ascribes to a behavior and that person’s sense of confidence that she or he can effect the change are the main determinants in whether the person will achieve the threshold level and make the change. Factors that contribute to this decision should be integral components of the assessment; they can be examined systematically, as outlined in Table 1-5. The individual is asked to weigh the benefits and costs of changing a given lifestyle behavior as opposed to not changing that behavior at that point in time. Decision balance analysis involves having the patient identify the benefits and costs of making a lifestyle change and of not making the change. This information is useful to the practitioner in directing and planning interventions that will effect changes in health behavior in an individual.
Table 1-5
Health Behavior Change: Decision Balance Analysis
| Change | No Change |
| Benefits | Benefits |
| 1. | 1. |
| 2. | 2. |
| 3. | 3. |
| 4. | 4. |
| Costs | Costs |
| 1. | 1. |
| 2. | 2. |
| 3. | 3. |
| 4. | 4. |
Modified from Rollnick S, Mason P, Butler C: Health behavior change: a guide for practitioners, Philadelphia, 2002, Churchill Livingstone.
People in need of care such as hospitalized patients are a receptive and captive audience. They present prime opportunities for identifying teachable moments. Even if older, these individuals are motivated to better understand their risk factors and to change their lifestyles.256
The impact of the physical therapist as a driver of change may reflect her or his capacity to serve as a role model. Physicians who exercise, for example, are more likely to advise that their patients exercise, as well as to advocate other positive health behaviors.257,258 Thus as a health care professional, practicing what one preaches may have a powerful effect on patient adherence to lifestyle change and health recommendations.
Evidence-Based Practice
Knowledge into Action
With the advent of Sackett’s rules of evidence259 and schemes for grading the quality of scientific studies and critical-appraisal topics,260 physical therapists have had to learn to be discriminating consumers of research. In addition, systematic reviews and metaanalyses have emerged to examine areas of practice where there are discrepancies in the literature regarding a treatment’s effect and to answer specific clinical questions. The levels of evidence and the grading recommendations for the quality of studies are shown in Table 1-6.
Table 1-6
Basis for Clinical Recommendations Based on Levels of Evidence and Grading of Recommendations
| Level of Evidence | Type of Evidence |
| I | Evidence is obtained from meta-analysis of multiple, well-designed, controlled studies. Randomized trials with low false-positive and low false-negative errors (high power). |
| Evidence is obtained from at least one well-designed experimental study. | |
| II | Randomized trials with high false-positive and/or negative errors (low power). |
| III | Evidence is obtained from well-designed, quasi-experimental studies, such as nonrandomized, controlled single group, pre-post, cohort, time, or matched case-control series. |
| IV | Evidence is from well-designed, nonexperimental studies such as comparative and correlational descriptive and case studies. |
| V | Evidence from case reports and clinical examples. |
| Grade | Grading of Recommendations |
| A | There is evidence of type I or consistent findings from multiple studies of types II, III, or IV. |
| B | There is evidence of types II, III, or IV and findings are generally consistent. |
| C | There is evidence of types II, III, or IV but findings are inconsistent. |
| D | There is little or no systematic empirical evidence. |
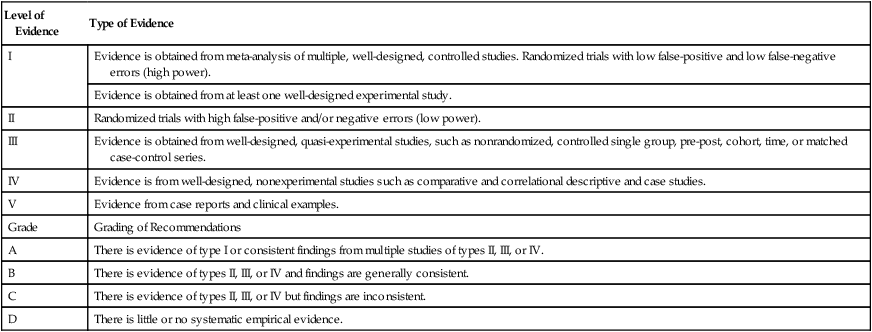
From Cook DJ, Guyatt GH, Laupacis A, et al: Rules of evidence and clinical recommendations on the use of antithrombotic agents, Chest 102(4 Suppl):305S–311S, 1992.
Physical Therapists as Drivers of Change
Strategies of behavioral change such as the transtheoretical model261 are being adopted with increasing frequency for the purpose of promoting healthy lifestyle change. Implementation of such a program in the workplace has been shown to increase physical activity in previously sedentary adults, to reduce the number of reported barriers to such activity, and to increase muscle endurance, predicted  , and flexibility.262
, and flexibility.262
Refocusing and Expanding the Clinical Repertoire of Physical Therapists
Today’s health care system is complex, and multiple forces drive the direction of types of services and their delivery. The reductionist perspective of the human body in the biomedical model largely predominates as the model underlying illness care. (Reductionism is the belief that the whole can be understood by the examination of small parts, that is, that treatment focuses on the disease rather than the mind and body as a whole.) Such illness care has been increasingly influenced by economic forces and directed care based on economic factors, such as drug prescription, rapid discharge from the hospital, and focus on process and functional outcomes.263 The absence of health promotion and wellness initiatives on a patient-by-patient basis before hospital discharge results from economic priorities, yet is a lost window of opportunity at a time when an individual may be receptive to information relating to changes in health behaviors—the teachable moment.263 Preventive information about nutrition, exercise, smoking cessation, and excessive alcohol consumption is not receiving the attention it deserves from health care providers or from patients.
As noninvasive practitioners, physical therapists are positioned professionally to be leaders in effecting health behavior change. Knowledge of physiology, pathophysiology, and clinical medicine and surgery is not sufficient for the physical therapist to be able to address complex, contemporary, population-wide health problems. To implement effective prevention and interventions with sustainable outcomes, the physical therapist has to consider the interface of treatments and recommendations for each individual. Establishing rapport, exploring the patient’s perception of the importance of change in health behavior, building confidence, exchanging information, and reducing resistance are key interpersonal skills needed to promote sustainable health-behavior change.264–266
The medical literature abounds with consensus statements of policies and procedures for treating specific conditions. Physical therapy has the expertise to develop parallel guidelines for noninvasive interventions, which in many instances, should be considered before invasive interventions or at least concurrently with them. The medical literature supports invasive care, so often it is not balanced with noninvasive interventions. For example, the report of the Sixth American College of Chest Physicians Consensus Conference on Antithrombotic Therapy has been cited in recommendations for patients following total hip arthroplasty.267 Physical therapy has a primary perioperative role in the prophylaxis and management of the potentially lethal effects of thrombosis after surgery. This perspective is relatively obscure in the position statement compared with the emphasis on drugs and other options; yet it is highly effective, has an excellent cost-benefit ratio, and results in minimal side effects compared with the systemic risks of antithrombotic therapy.
The time has come for a call to action within the physical therapy profession concerning the ill health that plagues our village. It is time to take a leadership role in the prevention of lifestyle-related conditions and their reversal, as well as remediation. In the pursuit of health and participation for all, physical therapists have a primary role in health care policy making, including the health of communities and countries, and should become involved in urban and environmental health initiatives, in community health planning,268–270 and in health and wellness programs, as well as continuing to provide vital one-on-one care to people. Physical therapists can be leaders in promoting community-based programs such as community-based tai chi programs270 and programs for individuals with physical challenges, including stroke.271,272 Community-based programs have been shown to be effective if they are well planned and supervised.
Translating sustainable health behavior from the hospital or clinic to the home cannot be assumed; rather, it is a unique skill that should be based on psychosocial teaching and learning factors. Although center- and clinic-based care is convenient for the health care provider, transitioning to home and community is fundamental to the process. The closer-to-home philosophy allows skills to be generalized from one setting to another. Closer-to-home health care delivery has attracted interest largely for economic reasons. However, the fact that better care and longer-lasting sustainable health behaviors may result is also a major reason to promote such care. Cardiac rehabilitation, for example, when initiated in the home environment in low-risk individuals, shows more sustainable physical and psychosocial benefits over time than when initiated in a facility.273 Community-based programs have to be adapted to the cultural and socioeconomic conditions of that community to promote optimal buy-in from the participants and to maximize their success.221,274
Continuing Professional Education
Another component of staying up to date through continuing education is reading the professional literature. Knowing what to read and understanding how to read the literature are as important to the clinician as clinical skills, and both skills have to be refined throughout the practitioner’s career. Table 1-7 rates the levels of quality of common publications and reading materials accessed by clinicians. Box 1-3 identifies important factors that should be considered when reading in order to enhance professional expertise. Journal clubs in the profession have become a popular means of sharing and discussing published information.
Table 1-7
Sources of Health Information and Quality Rating
| Information Source | Quality Rating |
| Scientific/Professional | Usually externally peer-reviewed journals (blind or nonblinded); although not infallible, information in journals has the highest probability of containing credible information, compared with other sources |
| Monographs | May or may not be peer reviewed |
| Books | Usually not peer reviewed |
| Professional newsletters | Typically not reviewed |
| Magazines | Highly variable |
| Newspapers | Highly variable |
| Television and radio | Highly variable |
| Internet | Highly variable |
Every Patient Is a Case Study
The randomized controlled clinical trial (RCCT) has become the gold standard for evaluating clinical interventions. Despite the scientific rigor involved, the limitations of the RCCT need to be appreciated by clinicians. Because of these limitations, Simon275 has argued that the clinical relevance of the RCCT may be overestimated and would be better described as a “silver standard.” The designs of RCCTs and their statistical analyses are based on probability theory. Because of this, results can be generalized only to comparable groups, not to an individual—the focus of the clinical situation. The results of RCCTs homogenize the outcomes for individuals who responded to treatment, failed to respond, or had negative outcomes. As clinical practitioners, we are interested in knowing how a particular individual with a given presentation will respond to a given treatment. The clinician needs to exercise a high level of clinical reasoning and judgment in determining the probability of a favorable response to a given treatment regimen in a given individual, based on studies of groups. Thus the physical therapist needs to understand the differences between the responders (favorable and unfavorable) in an RCCT and the nonresponders. This information is seldom detailed in published articles.
The clinical decision-making process is iterative and time limited.9 Physical therapy diagnoses are derived from detailed histories and assessments. Clinical hypotheses are formulated, and the physical therapist systematically evaluates them to establish the cause of the complaints and factors that contribute to them. The physical therapist selects valid and reliable measures and outcomes and conducts them in a standardized manner. The patient’s treatment response and prognosis are predicted so as to establish a timeline for treatment. Based on the assessment, each treatment intervention is prescribed (e.g., with respect to exercise, the type, intensity, duration, frequency, and course). Periodic reevaluation with established standardized outcomes measures are conducted to determine whether the patient has achieved the treatment objective and may be discharged or whether the prescriptions need to be modified and, if so, in what way. The relevant outcomes and outcome measures are identified at the start of treatment, and the treatment responses are evaluated over time until the predetermined outcomes are achieved within the predetermined time frame.
Aligning practice with research requires that the physical therapist apply research tools in practice, or at least have an understanding of them and their impact on drawing conclusions about the effect of treatment. For example, patients often improve spontaneously with time. This phenomenon is called “regression toward the mean.” Physical therapy often involves an eclectic treatment approach involving multiple interventions. Because of this, individual treatment effects cannot be isolated. Rather, the physical therapist has to conclude that treatments A, B, and C may have resulted in some improvement; however, the effect of spontaneous improvement with time can be determined only in a controlled clinical trial or on the basis of a prolonged unchanging baseline in the patient’s symptoms. Confounding variables such as medications and improvement with time need to be isolated so that it is possible to say that they may have contributed to the outcome, even if they cannot be ruled out. Confounding variables, which result from inadequate experimental control, cloud the interpretation of cardiovascular and pulmonary physical therapy studies.276 The effect of placebo also plays a major role in treatment outcome. This effect reflects such factors as patient expectancy. Once maligned and considered a characteristic of the hypochondriac, the placebo effect is now known to be a potent and clinically important self-healing effect that warrants being promoted. To date, there is little scientific evidence about how to exploit the power of the placebo effect systematically to promote self-healing.
Health promotion practice needs to be modified to the needs of a patient based on his or her cultural background and affiliation. Cultural competence in practice is geared toward augmenting clinical outcomes by adapting communication style, assessments, and treatments. Differences in people with respect to culture, traditions, and religion or faith can affect health, illness, health reporting, beliefs, and expectations about treatment intervention, as well as adherence to the treatment program. For example, the holy month of Ramadan requires creativity in managing the needs of Muslims. During Ramadan, Muslims fast from dawn to dusk, and the fast may include abstinence from water as well as from food. Sedentary people show greater adverse physiological effects during this period, both when at rest and during exercise, than do active people.277 Body weight drops in a predictable manner. The respiratory exchange ratio decreases during exercise, reflecting increased fat metabolism. Serum iron and platelets decrease, particularly in sedentary people, and fluid balance is better maintained in active people. Exercise, particularly whole-body exercise, may have to be curtailed or modified during fasting. This is especially true when Ramadan falls during the hot summer months.
Adapting lifestyle and treatment recommendations to the needs of the people physical therapists serve is fundamental to a successful outcome. The parameters of exercise prescription for optimal health benefits have been well documented (see Chapter 18). Prolonged adherence to physical activity and exercise programs, however, is poor. Understanding the factors that sustain health behaviors is as critical as the physiological basis for them. One study compared the effects of conventional aerobic training with the effects of a program designed to increase strength, endurance, and mind-body coordination but designed also for “comfort,” so that the program would be more appealing to people unused to exercise. After training, participants in the latter group had superior endurance compared with those in the conventional group, and they reported more comfort and less exertion. This preliminary study supported the idea that an exercise program modified for comfort and enjoyment still resulted in a greater capacity to adapt to increased physiological demands. Such programs should be extended so that adherence over time can be evaluated. In addition, readiness to change as described in the transtheoretical model needs to be considered in studies of long-term lifestyle change.278
Physical Therapy’s Role: Participation in Health Promotion Practice
Healthy lifestyle choices (specifically, not smoking, optimal nutrition, maintaining an optimal weight, not being sedentary, being physically active and exercising regularly, sleeping well and avoiding undue stress) can prevent lifestyle-related conditions. Should the risk factors or manifestations of lifestyle-related conditions emerge, adopting healthy living practices can reverse the risk factors or manifestations in some cases, as well as prevent future signs and symptoms. Given the established prevalence of lifestyle-related conditions, a primary clinical competency of physical therapy in the 21st century is multiple health behavior change.261,278 In addition to promoting health and wellness one on one, physical therapists need to present a high profile in health promotion and illness prevention by developing and writing physical therapy publications throughout the various levels of their professional associations. They can participate in consensus groups within these associations to issue physical therapy position statements, broadcast television and radio public service announcements, and set up information booths in shopping malls, community centers, and other strategic places within the community. Innovative wellness and prevention programs such as heart camps and retreats should be established.279 Such active leadership and participation by physical therapists enables them to exploit a range of avenues for effective communication and education strategies directed to the general public in addition to traditional one-on-one contact with patients.
Capitalizing on public health and condition-specific initiatives (e.g., Heart Month and Cancer Month) can reinforce existing community, state or province, national, and global health initiatives. The physical therapist needs to be proactive and function as a role model for health as a community leader by acknowledging these important initiatives and arranging activities to support them. Formal acknowledgment of the initiatives strengthens the profession’s identity and its responsibility regarding the conditions being addressed. It also educates the public and reinforces physical therapy’s role in the prevention, primary management, and in some cases, reversal of these conditions in the minds of the public, insurers, health care policy makers, health care colleagues, legislators, and others. For example, to address the serious pandemic of type 2 diabetes, the state of Tennessee has initiated statewide action. Schools and communities have been selected as primary prevention targets for the promotion of healthy food choices and activity programs.280 The initiative is multidisciplinary and multisectorial, and health profession organizations, government, churches, schools, and employers across the state are participating. The World Health Organization has several important annual health markers, including May 31 of each year, which has been designated as World No Tobacco Day. These occasions should be publicized and supported collectively by the physical therapy community globally.
Physical Therapy’s Role: Participation in Population-Wide Health Initiatives
As primary health care professionals, physical therapists are uniquely positioned to develop, support, and promote innovative health programs, thereby strengthening the health of communities en masse as well as doing so one person at a time in the clinic. Several excellent resources are available on the subject of building healthy neighborhoods and communities; they are highly recommended to physical therapists as bases for practicing at the levels of the village and community as well as the individual.281,282
Multicomponent, multiprofessional wellness and preventive health programs have been proposed to be components of each hospital department, including the emergency department. Hospital-based programs can be successfully implemented in diverse geographic areas and can be focused on each region’s needs.267 Despite the compelling benefits of home- and community-based care, their effectiveness cannot be assumed. Programs need to be judiciously targeted with due consideration given to the purpose of care, the target population, the congruence of the care and individuals’ needs and wants, and outcomes at the individual and societal levels.283
The Groningen Active Living Model is an example of a behavior change model that has been developed to encourage sedentary adults to be physically activity.55 The variables that were examined to determine program success included perceived fitness, social support, self-efficacy, and enjoyment. The outcomes were program adherence and physical activity. With respect to adherence, task self-efficacy was an important mediating variable in this cohort, followed by self-efficacy in overcoming barriers, in social support, and in enjoyment. Perceived physical ability and fitness were relatively less important mediators.
The Hearts for Life community-based program has shown positive outcomes with respect to risk reduction and improvement of knowledge.284 The Choose to Move physical activity program for women provides an important model for public health and participatory research organizations of targeted, low-cost self-help programs that support the Healthy People 2020285 objectives for physical activity, nutrition, and cardiovascular health.286 Women who completed the program increased their physical activity, reduced their consumption of high-fat foods, and increased their knowledge and awareness of cardiovascular risk and its symptoms. Schools and workplaces are also sites for innovative health programs in the community. Preventive cardiology programs for children, such as HeartPower!, show some success in nutritional domains.287 Such programs, however, could benefit from the expertise of a physical therapist with respect to developing, coordinating, integrating, and evaluating a physical activity and an exercise component. Low-income families in particular have an increased risk for inactivity and obesity. A school program for children of low-income families used the Internet, videos, provision of health snacks, and participation in a gym lab to promote exercise and healthy food choices.288 This program resulted in reduced fat intake and increased physical activity by the children.
One medium through which a physical therapist can assume the role of health coach has been through telerehabilitation. Telerehabilitation has come of age and is a major vehicle that can be exploited by physical therapists for targeted education of patients in the community289 and for general preventive health. Home-based education about nutrition and exercise has been reported as a means of targeting individuals with obstructive sleep apnea and promoting lifestyle change.290
Marketing research methods have been investigated as a means of improving population health outcomes and making their success rates comparable to those that have been well established in business marketing. Mass media promotion has been used to communicate an innovative physical activity and exercise resource called Small Steps.291 Callers responded to a mass publication campaign to promote Small Steps. People phoned toll free to a call-in center where trained screeners recruited members of the public into a controlled trial, identified their stage of readiness to change based on a few structured questions, and sent out the Small Steps kit, which provided information about being physically active and exercising, along with a workbook. More than 80% of the callers were women. The prospect of making small steps toward improving their health was as compelling for men as for women. At the 3-month follow-up, self-reported current levels of physical activity (main outcome) had changed substantially. Thus the results supported the idea that with the use of mass media, people who are in the preparation stage of being more physically active can shift to the action stage. Long-term studies are needed to establish the long-term benefits of this program and its translation into health outcomes. The reasons given for calling the resource center included the appeal of taking small steps when undertaking health behavior changes, improving nutrition, becoming more active, learning new things, and assisting others to improve their diets and activity levels.
The Magic Bullet and the Fountain of Youth
A “magic bullet” and a “fountain of youth” are not just myths. They exist, but they are not to be found in a pill or in surgery. For almost a century of documented physical therapy practice, education and exercise have been the hallmarks of the profession292–294 and the elixirs that add years to life and life to years. These “drugs” have been at the core of the practice of the physical therapist, who is distinguished from invasive-medicine practitioners primarily by the use of noninvasive “drugs” as opposed to the invasive interventions of pharmacotherapy and surgery. In addition to providing preventive health benefits, lifestyle changes such as smoking cessation, optimal nutrition, and exercise can enhance the quality of life295 and increase the probability of long-term health.