20
Eosinophilic Dermatoses
As with the group of disorders known as neutrophilic dermatoses, there is significant overlap in the cutaneous findings of entities where eosinophils play a role – from papular urticaria triggered by arthropod bites to Wells’ syndrome and hypereosinophilic syndrome (Fig. 20.1; Table 20.1). The exception is granuloma faciale, which has a more specific presentation.
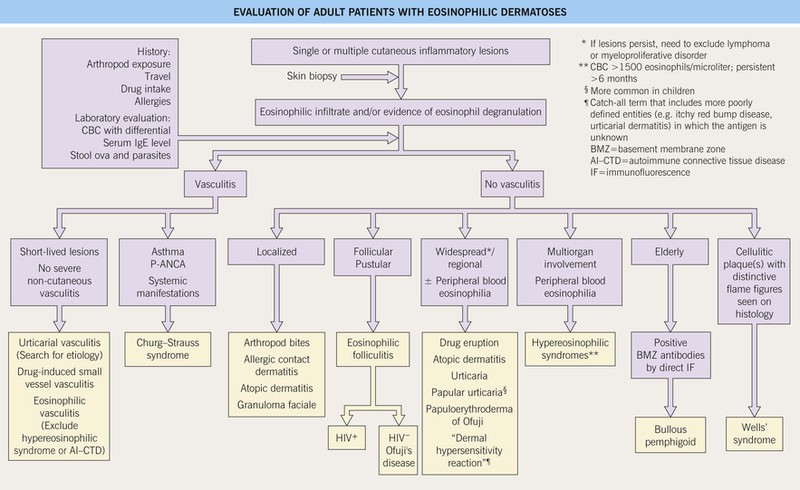
Fig. 20.1 Evaluation of adult patients with eosinophilic dermatoses. Histologically, these dermatoses are characterized by a prominent eosinophilic infiltrate and/or eosinophil granule protein deposition. Of note, systemic corticosteroids can significantly reduce the peripheral blood eosinophil count.
Table 20.1
Other disorders where eosinophils play a role (in addition to those listed in Fig. 20.1).
• Scabies – see Chapter 71
• Parasitic infections (e.g. larva migrans, onchocerciasis, schistosomiasis, strongyloidiasis)
• Seabather’s eruption – after ocean swimming, pruritic papules in distribution of swimsuit; due to larvae of either jellyfish (Linuche unguiculata) or sea anemones (Edwardsiella lineata)
• Pruritic papular eruption of HIV disease – nonfollicular pruritic papules
• Polymorphic eruption of pregnancy (also referred to as PUPPP) – urticarial plaques with involvement of striae and periumbilicial sparing; pregnant women
• Pemphigoid gestationis – urticarial plaques and vesicles similar to bullous pemphigoid; pregnant women
• Angiolymphoid hyperplasia with eosinophilia – nodules of the head and neck; adults
Limited to Neonates or Infants
• Erythema toxicum neonatorum – papules and pustules with erythematous flare; neonates
• Incontinentia pigmenti (stages I and II) – linear streaks of vesicles and keratotic papules along Blaschko’s lines
• Infantile eosinophilic folliculitis – recurrent crops of pruritic follicular papules and pustules, primarily of the head and neck
PUPPP, pruritic urticarial papules and plaques of pregnancy.
Granuloma Faciale
• Idiopathic disorder characterized by a persistent red-brown to violet-brown plaque on the face (Fig. 20.2); prominent follicular openings are often noted and a third of patients have multiple plaques.


Fig. 20.2 Granuloma faciale. Red-brown plaques on the lateral cheek (A) and nose (B). Note the prominent follicular openings. B, Courtesy, Cloyce L. Stetson, MD.
• DDx: sarcoidosis, foreign body granuloma, granulomatous rosacea, and other entities that lead to persistent red to red-brown plaques of the face (see Fig. 99.2).
• Rx: often difficult; intralesional CS, topical calcineurin inhibitors, cryosurgery, vascular lasers.
Exaggerated Insect Bite and Insect Bite-Like Reactions (Eosinophilic Dermatosis Associated with Hematologic Disorders/Malignancies)
• The most common associated systemic disorder is chronic lymphocytic leukemia, but these reactions can also be seen in patients with myeloproliferative disorders (see Table 99.2) and at sites of mosquito bites in those with Epstein–Barr virus-associated NK/T-cell lymphomas.
Papuloerythroderma of Ofuji
Wells’ Syndrome (Eosinophilic Cellulitis)
• Recurrent burning, pruritic or painful pink to red plaques that are often edematous, thus resembling infectious cellulitis; over time the lesions may become more infiltrative (Fig. 20.3).
• Associated symptoms include malaise and occasionally fever; peripheral eosinophilia is common.
• Within the dermis, there is a discharge of the granular contents of eosinophils, which then coat collagen fibers and lead to the formation of ‘flame figures’; the latter can also be seen in other disorders in which there are numerous eosinophils.
• DDx: infectious cellulitis (edematous lesions), exaggerated arthropod reactions (see above), parasitic infections, and other causes of pseudocellulitis (see Table 61.2).
• Rx: systemic CS; occasionally steroid-sparing agents are needed.
Hypereosinophilic Syndrome
• Classically defined as peripheral eosinophilia (>1500 eosinophils/microliter) for at least 6 months (or less than 6 months if associated end-organ damage), with multi-organ involvement, but in the absence of an identifiable cause (Table 20.2).
Table 20.2
Diagnostic criteria and classification of hypereosinophilic syndromes (HES).
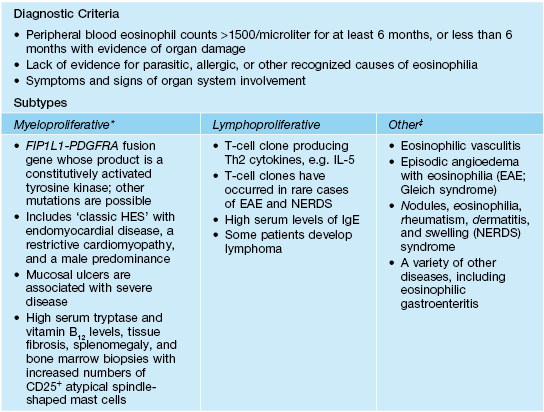
* Includes patients with eosinophilic leukemia, who may have other cytogenetic abnormalities; can also screen for other rare fusion genes or rearrangements involving PDGFRB or FGR1, which encode platelet-derived growth factor receptor (beta polypeptide) and fibroblast growth factor receptor-1, respectively.
‡ List is not exhaustive.
• Mucocutaneous lesions are seen in at least 50% of patients and include nonspecific pruritic erythematous papules and nodules, urticaria, angioedema, dermatitis, erythroderma, and in the myeloproliferative form, mouth or anogenital ulcers; thromboses can lead to retiform purpura.
• DDx: with the exception of granuloma faciale and eosinophilic folliculitis, the entities outlined in Fig. 20.1; several of the entities in Table 20.1, in particular parasitic infections; hereditary and acquired angioedema; for lymphoproliferative form, cutaneous T-cell lymphoma; if oral ulcers, oral aphthae.
For further information see Ch. 25. From Dermatology, Third Edition.