Envenomation by Marine Life
Interactions with various forms of marine life can result in anaphylactic reactions or envenomation.
Reaction to Sponges
Sponges (see Plate 36) are stationary animals that attach to the sea floor or coral beds. Embedded in their connective tissue matrices are spicules of silicon dioxide or calcium carbonate. Other chemical toxins and secondary coelenterate (stinging) inhabitants contribute to the skin irritation and systemic manifestations that result from dermal contact.
Signs and Symptoms
Treatment
2. To remove embedded microscopic spicules, apply sticky adhesive tape, a commercial facial peel, or a thin layer of rubber cement; then peel away the adherent spicules.
3. Apply a 5% acetic acid (vinegar) soak for 10 to 30 minutes three or four times a day. If vinegar is not available, use isopropyl alcohol 40%. Do not use a topical steroid preparation as the primary (initial) decontaminant because this may worsen the reaction.
4. After decontamination and at least two vinegar applications, use a mild emollient cream (e.g., hydrocortisone or triamcinolone) to soothe the skin.
5. If the allergic component is mild, apply a topical steroid preparation. If the allergic component is severe, as manifested by weeping, crusting, and vesiculation, administer a systemic corticosteroid (e.g., prednisone, 60 to 100 mg, tapered over 14 days).
6. Perform frequent follow-up wound checks because significant infections sometimes develop. Culture infected wounds and administer antibiotics (see Chapter 52).
Jellyfish Stings (Also Fire Coral, Hydroids, and Anemones)
Signs and Symptoms
1. Skin irritation: stinging, pruritus, paresthesias, burning, throbbing, redness, tentacle prints, impression patterns (see Plate 37), blistering, local edema, petechial hemorrhages, skin ulceration, necrosis, and secondary infection
2. Neurologic: malaise, headache, aphonia, diminished touch and temperature sensation, vertigo, ataxia, spastic or flaccid paralysis, mononeuritis multiplex, parasympathetic dysautonomia, plexopathy, peripheral nerve palsy, delirium, loss of consciousness, and coma
3. Cardiovascular: anaphylaxis, hemolysis, hypotension, small artery spasm, bradycardia, tachycardia, congestive heart failure, and ventricular fibrillation
4. Respiratory: rhinitis, bronchospasm, laryngeal edema, dyspnea, cyanosis, pulmonary edema, and respiratory failure
5. Musculoskeletal: abdominal rigidity, myalgias, muscle cramps/spasm, arthralgia, and arthritis
6. Gastrointestinal: nausea, vomiting, diarrhea, dysphagia, hypersalivation, and thirst
7. Ocular: conjunctivitis, chemosis, corneal ulcer, iridocyclitis, elevated intraocular pressure, and lacrimation
8. Other: chills, fever, acute renal failure, and nightmares
Treatment
a. Maintain the airway and administer oxygen.
b. Obtain intravenous access. Administer lactated Ringer’s solution or normal saline solution to support the blood pressure to at least 90 mm Hg systolic.
c. Treat anaphylaxis if present (see Chapter 26).
d. If the sting is from the box jellyfish (Chironex fleckeri) (see Plates 38 and 39) or severe and from the sea wasp (Chiropsalmus quadrigatus), consider immediate administration of C. fleckeri antivenom. Administer this in a dose of one ampule (20,000 units per ampule) IV diluted 1 : 5 to 1 : 10 in isotonic crystalloid. A large sting in an adult may require the initial administration of two ampules. Alternatively, administer this in a dose of three ampules intramuscularly into the thigh. Antivenom administration may be repeated once or twice every 2 to 4 hours until there is no further worsening of the reaction (skin discoloration, pain, or systemic effects).
e. If the sting is from the Irukandji (Carukia barnesi), hypertension from catecholamine stimulation may be severe. If necessary, administer an α-adrenergic blocking agent (phentolamine, 5 mg IV initially, followed by an infusion of up to 10 mg/hr).
f. Authorities no longer recommend the pressure immobilization technique to treat a box jellyfish sting or any other jellyfish sting.
a. If possible, apply a topical decontaminant immediately (described in step d, later). If more than 1 or 2 minutes will elapse before the application of the decontaminant, rinse the wound with seawater. Do not rinse gently with freshwater; if freshwater is to be used, the stream must be forceful (e.g., jet stream from a shower or hose).
b. Hot packs or showers to tolerance (45° C [113° F]) may be more effective than dry, (nonmoist), cold (insulated ice) packs.
c. Do not rub or abrade the wound.
d. If these have been done, apply a topical decontaminant. The efficacy may vary depending on the stinging species.
• Acetic acid 5% (vinegar) is the decontaminant of choice with a box jellyfish (C. fleckeri) sting.
• For other stings, diminish the pain using vinegar, isopropyl (rubbing) alcohol 40%, sodium bicarbonate (baking soda), papain (papaya latex or nonseasoned meat tenderizer, the latter in a brief [<15 minutes] application), or dilute household ammonia. Other substances that may be effective include sugar or olive oil, or lemon or lime juice. Urinating on the sting is generally not helpful. A sting from the Australian Physalia physalis, a recently differentiated species, should not be doused with vinegar.
• Do not apply a solvent (e.g., formalin, ether, gasoline).
• Perfume, aftershave, or high-proof liquor may worsen the skin reaction.
e. After decontamination, remove the adherent nematocysts. Apply shaving cream or a paste of soap or baking soda, flour, or talc, and shave the area with a razor or other sharp edge.
f. Apply a local anesthetic ointment or mild steroid preparation to soothe the skin.
g. If the reaction is severe, administer a systemic corticosteroid (e.g., prednisone, 60 to 100 mg, tapered over 14 days).
h. Inspect the wound regularly for ulceration and the onset of infection.
3. If the eye is involved, it should be anesthetized with proparacaine 0.5% and irrigated to 100 to 250 mL of normal saline to remove foreign matter. Slit lamp examination and fluorescein staining to identify corneal defects are recommended.
Prevention
1. Give all jellyfish a wide berth when swimming or diving.
2. Wear a “stinger suit” when immersed in jellyfish-infested water.
3. When diving, scan for surface concentrations of stinging animals.
4. If “stinger enclosures” are present, do not venture beyond their confines.
5. Consider the use of a topical skin protective preparation such as Safe Sea (jellyfish-safe sunblock).
Sea Bather’s Eruption
Signs and Symptoms
1. Stinging of the skin while still in the water or immediately on exiting; may be intensified by the application of fresh water
2. Skin redness, papules (see Plate 40), urticaria, and blisters minutes to 12 hours after exposure
a. Most common areas: buttocks, genitals, and under breasts (women)
b. Individual lesions resembling insect bites
c. Also seen under bathing caps and swim fins and along the edge of the cuffs of wet suits
3. Fever, chills, headache, fatigue, malaise, vomiting, conjunctivitis, and urethritis
Treatment
1. Apply a topical decontaminant. Acetic acid 5% (vinegar) seems to be less effective than papain. Otherwise, scrub thoroughly with soap and water.
2. After decontamination, apply calamine lotion with 1% menthol to control itching. A high-potency topical corticosteroid preparation may be of benefit.
3. If the reaction is severe, administer a systemic corticosteroid (e.g., prednisone, 60 to 100 mg, tapered over 14 days).
Starfish Puncture
The most common venomous starfish (Fig. 53-1) have glandular tissue interspersed underneath the epidermis that covers the rigid spines, which may attain a length of 4 to 6 cm (1.6 to 2.4 inches). The envenomation occurs when a spine punctures the skin.

FIGURE 53-1 Spines of the crown-of-thorns starfish (Acanthaster planci). (Courtesy Paul Auerbach, MD.)
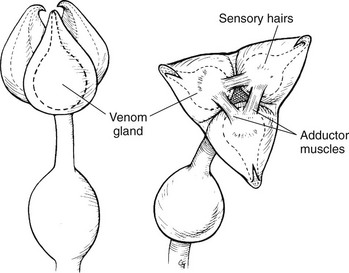
Sea Urchin Spine Puncture or Envenomation by Pedicellariae
Sea urchins envenom their victims in one of two ways: (1) puncture wound by sharp, venom-bearing spine(s) or (2) inoculation of venom via the venom gland in the base of flower-like, stalked pincer organs (globiferous pedicellariae) (Fig. 53-2).
Treatment
1. Immerse the wound in nonscalding, hot water to tolerance (45° C [113° F]) for 30 to 90 minutes or until significant pain relief.
2. Remove any obvious spine fragments. Do not attempt to crush remaining fragments. If spines are felt to remain within the patient near a joint, splint the affected limb.
3. If pedicellariae are attached, apply shaving foam and scrape them away with a razor.
Sea Cucumber Irritation
Sea cucumbers are worm- or sausage-shaped bottom feeders (Fig. 53-3). They produce in their body walls a visceral cantharidin-like toxin that is concentrated in tentacular organs that can be projected and extended anally when the animal mounts a defense.

FIGURE 53-3 Extruded tentacular organs of Cuvier from within a sea cucumber. (Courtesy Paul Auerbach, MD.)
Treatment
1. Wash the skin with soap and water.
2. Because sea cucumbers may feed on stinging cells of jellyfish, initial skin detoxication should include topical application of 5% acetic acid (vinegar), papain, or 40% isopropyl alcohol.
3. If the eye is involved, it should be anesthetized with proparacaine 0.5% and irrigated with 100 to 250 mL of normal saline to remove foreign matter. Slit lamp examination and fluorescein staining to identify corneal defects are recommended.
Bristleworm Irritation
Certain segmented marine worms have chitinous bristles arranged in soft rows around the body (see Plate 42). These are dislodged into the human victim when a worm is handled.
Signs and Symptoms
Burning sensation, raised red urticarial rash, papular dermatitis, soft tissue edema, and pruritus
Treatment
1. Remove all large visible bristles using forceps.
3. To remove embedded spines, apply sticky adhesive tape, a commercial facial peel, or a thin layer of rubber cement; then peel away the adherent spines.
4. Apply acetic acid 5% (vinegar), isopropyl alcohol 40%, dilute ammonia, or a paste of unseasoned meat tenderizer for 10 to 15 minutes to achieve pain relief.
5. Apply a thin layer of a topical corticosteroid preparation.
6. If the reaction is severe, administer a systemic corticosteroid (e.g., prednisone, 60 to 100 mg, tapered over 14 days).
Cone Shell (Snail) Sting
These cone-shaped shelled mollusks intoxicate their victims by injecting rapid-acting venom by means of a detachable, dart-like radular tooth (Fig. 53-4).
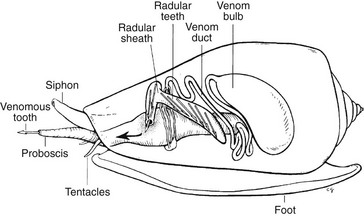
FIGURE 53-4 Venom apparatus of cone shell.
Signs and Symptoms
1. Mild sting (puncture) that resembles bee or wasp sting
2. Alternative initial symptoms: localized ischemia, cyanosis, numbness in area around wound
3. More serious envenomations: paresthesias at wound site, which become perioral and then generalized
4. Dysphagia, nausea, syncope, weakness, areflexia, aphonia, diplopia, blurred vision, pruritus, disseminated intravascular coagulation, generalized muscular paralysis leading to respiratory failure, cardiac failure, and coma
Treatment
1. Apply the pressure immobilization technique for venom sequestration (see Chapter 37): If practical by virtue of the sting’s location, place a cloth or gauze pad 6 to 8 cm (2.4 to 3.1 inches) by 2 cm (0.8 inch) thick directly over the sting, and hold it firmly in place using a circumferential bandage 15 to 18 cm (5.9 to 7 inches) wide, applied at lymphatic-venous occlusive pressure. If the cloth or gauze pad is not available, a rolled bandage may be used alone.
a. Do not occlude the arterial circulation, as determined by the detection of arterial pulsations and proper capillary refill.
b. Splint the limb, and do not release the bandage until after the patient has been brought to proper medical attention and you are prepared to provide systemic support, or after 24 hours.
c. Check frequently that swelling beneath the bandage has not compromised the arterial circulation.
Blue-Ringed Octopus Bite
Signs and Symptoms
1. Local reaction: one or two puncture wounds characterized by minimal discomfort, described as minor ache, slight stinging, or pulsating sensation
a. Occasionally, initial numbness at the site, followed in 5 to 10 minutes by discomfort that may spread to involve the entire limb, persisting for up to 6 hours
b. Within 30 minutes: redness, swelling, tenderness, heat, and pruritus
c. Most common local tissue reaction: absence of symptoms, small spot of blood, or tiny blanched area
2. Within 10 to 15 minutes: oral and facial numbness, followed rapidly by diplopia, blurred vision, aphonia, dysphagia, ataxia, myoclonus, weakness, sense of detachment, nausea, vomiting, flaccid muscular paralysis, and respiratory failure
Stingray Spine Puncture
Signs and Symptoms
1. Immediate local intense pain with central radiation, soft tissue edema, and dusky (ischemic) discoloration with surrounding erythema
2. Rapid (hours to days) fat and muscle hemorrhage and necrosis
3. Weakness, nausea, vomiting, diarrhea, diaphoresis, vertigo, tachycardia, headache, syncope, seizures, inguinal or axillary pain, muscle cramps, fasciculations, generalized edema (with truncal wounds), paralysis, hypotension, and arrhythmias
Treatment
1. Immerse the wound in nonscalding hot water to tolerance (45° C [113° F]) for 30 to 90 minutes or until there is significant pain relief. No reason exists to add ammonia, magnesium sulfate, potassium permanganate, or a solvent to the soaking solution. Do not immerse the wound in ice water.
2. Remove any obvious spine fragments. This may be done during the hot water soak. However, if the spine is seen to be lodged in the patient and has penetrated deeply into the chest, abdomen, or neck and may have violated a critical blood vessel of the heart, it should be managed as a weapon of impalement (e.g., knife) would be. In this case the spine should be left in place (if possible) and secured from motion until the patient is brought to a controlled operating room environment where emergency surgery can be performed to guide extraction of the spine and control bleeding that may occur on its removal.
3. Administer appropriate pain medications. Consider local or regional anesthetic administration.
4. Administer prophylactic antibiotics if the wound is more than minor or if the patient is immunocompromised (see Chapter 52).
5. Do not suture the wound closed unless bleeding cannot be controlled with pressure or this wound closure method is necessary for evacuation.
Scorpion Fish Spine Puncture
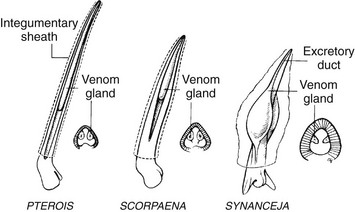
Scorpion fish (Fig. 53-5), lionfish (Fig. 53-6), and stonefish (Fig. 53-7) envenom their victims using dorsal, anal, and pelvic spines, which are erected as a defense mechanism (Fig. 53-8). Other venomous fish that sting in a manner similar to scorpion fish include the Atlantic toadfish, European ratfish, rabbitfishes, stargazers, and leatherbacks. Other marine fishes carry spines that envenom to a lesser degree.

FIGURE 53-5 Scorpion fish assuming the coloration of its surroundings. (Courtesy Paul Auerbach, MD.)
FIGURE 53-6 Adult lionfish. (Courtesy Paul Auerbach, MD.)
Signs and Symptoms
1. Immediate, intense pain with central radiation
a. If untreated, pain peaking at 60 to 90 minutes and persisting for 6 to 12 hours (stonefish)
b. Stonefish pain possibly severe enough to cause delirium and persisting at high levels for days
2. Wound and surrounding area initially ischemic and then cyanotic, with more broadly surrounding areas of erythema, edema, and warmth
3. Anxiety, headache, tremors, maculopapular rash, nausea, vomiting, diarrhea, abdominal pain, diaphoresis, pallor, restlessness, delirium, seizures, limb paralysis, peripheral neuropathy, lymphangitis, arthritis, fever, hypertension, respiratory distress, pulmonary edema, bradycardia, tachycardia, atrioventricular block, ventricular fibrillation, congestive heart failure, syncope, and hypotension
Treatment
1. Immerse the wound in nonscalding hot water to tolerance (45° C [113° F]) for 30 to 90 minutes or until significant pain relief occurs. No reason exists to add ammonia, magnesium sulfate, potassium permanganate, or a solvent to the soaking solution. Do not immerse the wound in ice water.
2. Remove any obvious spine fragments. This may be done during the hot water soak.
3. Administer appropriate pain medications. Consider local or regional anesthetic administration.
4. Administer prophylactic antibiotics if the wound is more than minor or the patient is immunocompromised (see Chapter 52).
5. Give stonefish antivenom in cases of severe systemic reaction from stings of Synanceja species. The antivenom is supplied in ampules containing 2 mL (2000 units) of hyperimmune horse serum, with one vial neutralizing one or two significant punctures. Anticipate anaphylaxis associated with the administration of an antivenom product.
Catfish Spine Sting
Signs and Symptoms
1. Instantaneous stinging, throbbing, or scalding pain with central radiation; normally, pain subsiding within 30 to 60 minutes, but possibly lasting up to 48 hours
2. Area around the wound ischemic, with central pallor that grows cyanotic before onset of erythema and edema
3. Local muscle spasm, diaphoresis, fasciculations, weakness, syncope, hypotension, and respiratory distress
Treatment
1. Immerse the wound in nonscalding hot water to tolerance (45° C [113° F]) for 30 to 90 minutes or until significant pain relief occurs. No reason exists to add ammonia, magnesium sulfate, potassium permanganate, or a solvent to the soaking solution. Do not immerse the wound in ice water.
2. Remove any obvious spine fragments. This may be done during the hot water soak.
3. Administer appropriate pain medications. Consider local or regional anesthetic administration.
4. Administer prophylactic antibiotics if the wound is more than minor or the patient is immunocompromised (see Chapter 52).
5. Be aware that tiny Amazonian catfishes swim up the human urethra and are not easily dislodged. Ingestion of a large quantity of ascorbic acid (vitamin C), which is then excreted in the urine, may soften the spines and allow the fish to be “passed.”
Weever Fish Spine Sting
Signs and Symptoms
1. Instantaneous burning, scalding, or crushing pain with central radiation
a. Peak of pain at 30 minutes with subsidence within 24 hours, but can last for days
b. Possibly of an intensity sufficient to induce irrational behavior and syncope
2. Little bleeding at puncture wound site; often appears pale and edematous initially
a. Over 6 to 12 hours, wound becoming red, ecchymotic, and warm
b. Increasing edema for 7 to 10 days, causing the entire limb to become swollen
3. Headache, delirium, aphonia, fever, chills, dyspnea, diaphoresis, cyanosis, nausea, vomiting, seizures, syncope, hypotension, and cardiac arrhythmias
Treatment
1. Immerse the wound in nonscalding hot water to tolerance (45° C [113° F]) for 30 to 90 minutes or until significant pain relief occurs. No reason exists to add ammonia, magnesium sulfate, potassium permanganate, or a solvent to the soaking solution. Do not immerse the wound in ice water.
2. Remove any obvious spine fragments. This may be done during the hot water soak.
3. Administer appropriate pain medications. Consider local or regional anesthetic administration.
4. Administer prophylactic antibiotics if the wound is more than minor or the patient is immunocompromised (see Chapter 52).
Sea Snake Bite
Signs and Symptoms
1. Onset potentially delayed by up to 8 hours
2. No appreciable local reaction to a sea snake bite other than the initial pricking sensation
3. Initially, euphoria, malaise, or anxiety
4. Over 30 to 60 minutes, classic muscle aching and stiffness (particularly of the bitten extremity and neck muscles), along with dysarthria and sialorrhea
5. Within 3 to 6 hours, moderate to severe pain with passive movements of the neck, trunk, and limbs
6. Ascending flaccid or spastic paralysis, beginning in lower extremities
7. Nausea, vomiting, myoclonus, muscle spasm, ophthalmoplegia, ptosis, dilated and poorly reactive pupils, facial paralysis, and trismus
8. In severe cases, skin cool and cyanotic, loss of vision, and possible coma
Treatment
1. Apply the pressure immobilization technique for venom sequestration (see Chapter 37).
2. Be prepared to assist ventilations. Administer oxygen.
3. With any evidence of envenomation, give polyvalent sea snake antivenom. The minimum effective adult dosage is 1 ampule (1000 units). The patient may require 3 to 10 ampules depending on the severity of the envenomation. Anticipate anaphylaxis associated with the administration of an antivenom product. Tiger snake antivenom is no longer recommended for use if sea snake antivenom is unavailable.