CHAPTER 23 ENDPOINTS OF RESUSCITATION
The optimal endpoint of resuscitation has been debated since the early 20th century when Cannon espoused his controversial viewpoints concerning limited volume resuscitation, and it continues to be a topic of tremendous discussion and study. The ideal endpoint should be readily obtainable and easily interpretable. The goal is to provide adequate oxygen delivery (DO2) and therefore tissue perfusion without producing the complications of over-resuscitation. This is accomplished primarily by increasing cardiac output via increases in preload (volume loading) or vasoactive drugs. Multiple diagnostic measurements have been used to determine both optimal cardiac performance and adequate tissue perfusion. While no single value can be used exclusively, various measurements do allow uniformity in comparing adequacy of resuscitation. The values provide the ability over time to determine whether a patient is being properly resuscitated. These can be categorized into hemodynamic parameters, metabolic parameters, and regional perfusion endpoints.
HEMODYNAMIC PARAMETERS
Vital Signs and Clinical Endpoints
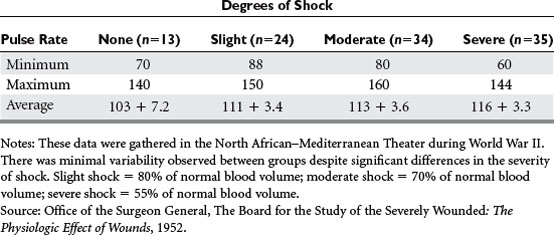
Shock has been defined in a multitude of ways, but can best be described as a lack of adequate tissue perfusion, and thereby an impairment of oxygen delivery and removal of waste products. The six basic advanced trauma life support (ATLS) physiologic parameters that have been used to identify shock are heart rate, respiratory rate, blood pressure, urine output, level of consciousness, and pulse pressure. Urine output and level of consciousness are direct measurements of tissue perfusion, and are defined by the classes of shock. Renal blood flow correlates with arterial pressure, but can be subject to significant autoregulation during periods of hypoperfusion. Level of consciousness is less reliable when influenced by intoxication, central nervous system injury, and medication. Heart rate and respiratory rate can be notoriously misleading (Table 1). Anxiety, pain, and stress secondary to the emotional impact of trauma can falsely elevate these physiologic parameters. This can confuse the picture and mask the underlying severity of shock. The diagnosis of shock is best made by observing the body’s main compensatory mechanism: redistribution of blood flow.
Invasive Monitoring
Many have attempted to define the oxygen consumption/delivery endpoint itself, but with no clear results. The Fick equation states that DO2 and VO2 are functions of cardiac performance (CI), hemoglobin (Hb), and arterial and venous oxygen saturations (SaO2 and SvO2, respectively):
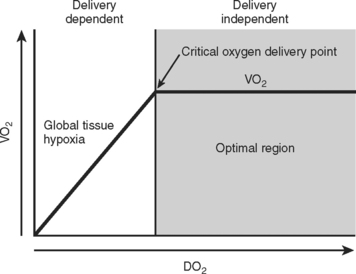
Unfortunately, DO2 and VO2 are both derived from cardiac output, and the stable plateau described in Figure 1 is virtually impossible to obtain. Goal-directed therapy, aimed at ensuring CI greater than 4.5 l/min/m2, DO2 index greater than 600 ml/min/m2, and VO2 index greater than 170 ml/min/m2, has been advocated by Shoemaker and others, showing reduced morbidity and mortality in critically ill patients. However, Gattinoni in a multicenter randomized controlled trial, and Heyland in a meta-analysis, have shown that no such benefit exists. Furthermore, a prospective, randomized controlled trial by Velmahos comparing conventional versus supranormal endpoints demonstrated that despite all efforts, only 70% of patients were able to reach these endpoints. They concluded that regardless of the resuscitation strategy, the ability of the patient to achieve “optimal hemodynamic values” significantly affected outcome. Looking at O2 delivery alone, McKinley et al. found that there was no difference in outcome between groups resuscitated to an O2 delivery goal of 600 ml/min/m2 versus 500 ml/min/m2.
METABOLIC PARAMETERS
Base Deficit
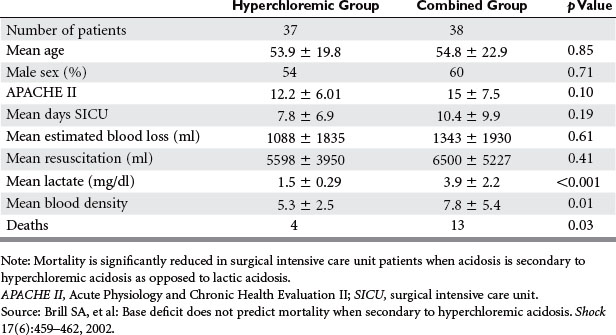
Base deficit has been advocated as a useful clinical marker for assessing reduced tissue perfusion and as a convenient marker of elevated lactate levels. It is defined as the amount of base (millimoles) required to raise 1 liter of whole blood to a normal pH. Davis first classified the base deficit according to severity: mild (2–5 mmol/l), moderate (6–14 mmol/l), or severe (>15 mmol/l). The severity of the deficit directly correlated with the volume of crystalloid and blood replaced within the first 24 hours. It has been shown that serum bicarbonate levels, which may be more readily available, correlate well with base deficits, but they are affected by the patient’s ventilatory status. Similar to lactate, the absolute base deficit can estimate the severity of shock, but no single value can be used as an endpoint. Persistently high or worsening base deficits may be an indicator of complications such as abdominal compartment syndrome or ongoing hemorrhage. Greater severity of base deficit does predict diminished oxygen consumption, increased risk of multiple organ dysfunction syndrome, and greater mortality. However, base deficit secondary to hyperchloremic acidosis is not associated with increased mortality or complications as demonstrated by Brill et al. (Table 2). The inaccurate interpretation of an elevated base deficit that is truly related to hyperchloremic acidosis may result in unnecessary interventions such as ongoing fluid resuscitation, blood transfusion, or even operative interventions. As with lactate, the trend of the base deficit over time is more useful in predicting outcomes.
REGIONAL PERFUSION ENDPOINTS
A multitude of devices that directly measure the tissue microcirculation have been developed. These include gastric tonometry, sublingual capnography, and near-infrared spectroscopy (NIRS). Gastric tonometry monitors the gastric intramucosal pH (pHi), by measuring the level of tissue pCO2. pHi decreases as splanchnic perfusion decreases. For this test to be accurate, gastric feedings need to be withheld and gastric acid secretion needs to be suppressed. Unfortunately, it correlates poorly with lactate and base deficit, and has a prolonged calibration time. It has been suggested in studies that a lower pHi correlates with the development of multiorgan dysfunction syndrome and increased mortality. Sublingual capnography uses the premise that global tissue hypoperfusion causes systemic hypercarbia. It has been proven to correlate with lactate levels, as well as the severity of shock, and has been used as a predictor of mortality. Finally, NIRS can be used to determine tissue oxygen saturation (StO2) (Figure 2). The NIRS technology allows the simultaneous measurement of tissue pO2, pCO2, and pH. In animal models of hemorrhagic shock, StO2 closely correlated with measured oxygen delivery, and was a superior measurement of shock compared to lactate, base excess, or SvO2. McKinley et al. found that StO2 correlated with oxygen delivery, base deficit, and lactate levels in severely injured trauma patients. NIRS can also monitor mitochondrial function by monitoring the redox state of cytochrome aa3, which reflects mitochondrial oxygen consumption. Under normal conditions, tissue oxyhemoglobin levels (HbO2) and cytochrome aa3 levels are tightly coupled. Cairns et al. noted that in a study of 24 severely injured trauma patients, 9 patients who developed multiorgan failure (MOF) had HbO2 and cytochrome aa3 decoupling. Only 2 of 16 patients who did not develop MOF had decoupling. Many of these devices have failed to gain widespread use and have not been standardized.
Abramson MD, et al. Lactate clearance and survival following injury. J Trauma. 1993;35(4):584-589.
Bishop MH, et al. Prospective, randomized trial of survivor values of cardiac index, oxygen delivery, and oxygen consumption as resuscitation end-points in severe trauma. J Trauma. 1998;38(5):780-787.
Boyd O, Grounds R, Bennett ED. A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk surgical patients. JAMA. 1993;270(22):2699-2707.
Brain Trauma Foundation, American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care. Hypotension. J Neurotrauma. 2000;17(6–7):591-595.
Brill SA, et al. Base deficit does not predict mortality when secondary to hyperchloremic acidosis. Shock. 2002;17(6):459-462.
Chang MC, et al. Gastric tonometry supplements information provided by systemic indicators of oxygen transport. J Trauma. 1994;37:488-494.
Cheatham ML, et al. Right ventricular end-diastolic volume index as a predictor of preload status in patients on positive end-expiratory pressure. Crit Care Med. 1998;26:1801-1806.
Connors AFJr, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA. 1996;276(11):889-897.
Davis JW, et al. Base deficit as a guide to volume resuscitation. J Trauma. 1988;28:1464-1467.
DeFigueiredo LF, et al. Cardiac output determination during experimental hemorrhage and resuscitation using a transesophageal Doppler monitor. Artif Organs. 2004;28:338-342.
Gattinoni L, et al. A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med. 1995;333(16):1025-1032.
Hussain FA, et al. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185:485-491.
Ivatury RR, et al. A prospective randomized study of end points of resuscitation after major trauma: global oxygen transport indices versus organ-specific gastric mucosal pH. J Am Coll Surg. 1996;183:145-154.
Kincaid EH, et al. Elevated arterial base deficit in trauma patients: a marker of impaired oxygen utilization. J Am Coll Surg. 1998;187(4):384-392.
Miller PR, Meredith JW, Chang MC. Randomized, prospective comparison of increased preload versus inotropes in the resuscitation of trauma patients: effects on cardiopulmonary function and visceral perfusion. J Trauma. 1998;44:107-113.
Shah MR, et al. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA. 2005;294(13):1664-1670.
Schreiber MA, et al. Determinants of mortality in patients with severe blunt head injury. Arch Surg. 2002;137(3):285-290.
Shoemaker WC, et al. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176-1186.
Velmahos GC, et al. Endpoints of resuscitation of critically injured patients: normal or supranormal? A prospective randomized trial. Ann Surg. 2000;232(3):409-418.
Weil MH, et al. Sublingual capnometry: a new noninvasive measurement for diagnosis and quantitation of severity of circulatory shock. Crit Care Med. 1999;27:1225-1229.