Chapter 24 Endoscopy-Assisted Thoracic Microdiscectomy
Historically, spinal surgeons have sought to find a surgical procedure of choice to treat thoracic disc herniations [1–14]. The threat of spinal cord, neural, vascular, and pulmonary injuries has stimulated many attempted approaches, including posterior laminectomy (seldom performed because it is too likely to result in neurologic injury), costotransversectomy, transthoracic, transpleural, posterolateral, transfacet pedicle-sparing, transpedicular, and, more recently, transthoracic endoscopic and posterolateral endoscopic procedures [4,5,11–17].
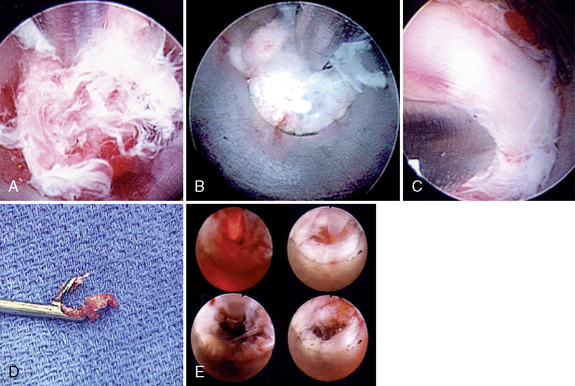
Many clever, minimally invasive surgical endoscopic thoracic procedures, including video-assisted thoracic surgery (VATS) [1,2,4,5] and thoracic sympathectomy, have been developed in an attempt to reduce operative trauma. Endoscopy-assisted thoracic discectomy (EATD) (i.e., posterolateral endoscopic thoracic discectomy) is an alternative procedure for treating symptomatic herniated thoracic discs through an endoscope to cause less tissue trauma than current conventional thoracic disc surgery and thoracoscopic procedures [5,11–21]. In laser thermodiscoplasty, tissue modulation technology of a lower-energy non-ablative laser is applied for shrinkage and tightening of the disc [5,10–15,18].
A significant number of patients with thoracic disc herniations complain of intractable thoracic spinal and paraspinal pain, intercostal or chest wall pain, upper abdominal pain, and, occasionally, low back pain due to thoracic disc protrusions without severe neurologic deficit. With improved diagnostic methods such as magnetic resonance imaging (the method of choice), computed tomography myelograms, and computed tomography scans, the diagnosis of these thoracic disc herniations or protrusions is now far more common [5,11–15]. Usually, patients with such conditions undergo some period of physical therapy, injection therapy, and analgesics, but if these treatments are not effective, the patients are often expected to live with their discomfort because of the fear of the potentially severe postoperative complications associated with surgical treatment [5,11–15].
Treatment objective of endoscopy-assisted thoracic discectomy
 The objective of EATD is the microdecompressive endoscopy-assisted thoracic discectomy of herniated thoracic disc and foraminal disc herniation. It is a minimally invasive, outpatient procedure with minimal tissue trauma and much less morbidity than open thoracic spinal surgery. There is no bone graft or fusion hardware to cause secondary problems, and the is procedure is associated with significantly lower associated convalescence periods and costs. Also, multiple thoracic discs may be treated at one sitting [5,11–15,19–21].
The objective of EATD is the microdecompressive endoscopy-assisted thoracic discectomy of herniated thoracic disc and foraminal disc herniation. It is a minimally invasive, outpatient procedure with minimal tissue trauma and much less morbidity than open thoracic spinal surgery. There is no bone graft or fusion hardware to cause secondary problems, and the is procedure is associated with significantly lower associated convalescence periods and costs. Also, multiple thoracic discs may be treated at one sitting [5,11–15,19–21].Indications
The indications for EATD are as follows [5,11–16]:
 Pain along the thoracic spine, often radiating to the chest wall, with possible numbness and paresthesia in an intercostal distribution related to thoracic disc herniation.
Pain along the thoracic spine, often radiating to the chest wall, with possible numbness and paresthesia in an intercostal distribution related to thoracic disc herniation.Contraindications
EATD is contraindicated by the following findings or conditions [5,11–16]:
 Demonstration of severe cord compression or total block on radiographic studies secondary to severe thoracic disc extrusions that cause cord compression with severe neurologic deficit (paraparesis).
Demonstration of severe cord compression or total block on radiographic studies secondary to severe thoracic disc extrusions that cause cord compression with severe neurologic deficit (paraparesis).Advantages
The advantages of EATD over open procedures are as follows:
 Is commonly performed with use of local anesthesia and intravenous conscious sedation; usually no general anesthesia required
Is commonly performed with use of local anesthesia and intravenous conscious sedation; usually no general anesthesia required Does not require dissection of muscle, bone, or ligaments or manipulation of the dural sac, spinal cord, or nerve roots
Does not require dissection of muscle, bone, or ligaments or manipulation of the dural sac, spinal cord, or nerve roots Does not involve resection of rib, so there is no need to collapse the lung or open the pleural cavity
Does not involve resection of rib, so there is no need to collapse the lung or open the pleural cavityInstrumentation
The following instruments and equipment are needed for EATD:
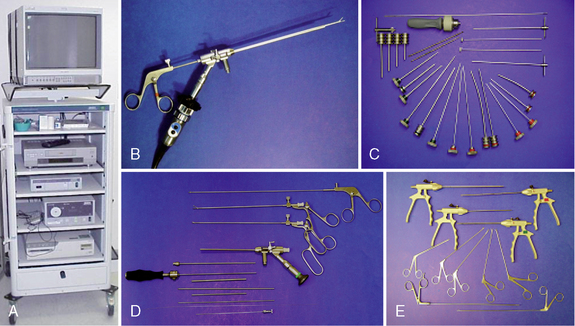
 Endoscopic tower equipped with digital video monitor, DVD recorder, light source, and photo printer, with tri-chip digital camera system (Karl Storz, Tuttlingen, Germany) (Fig. 24-2)
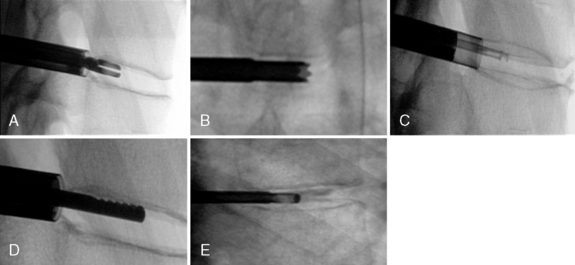
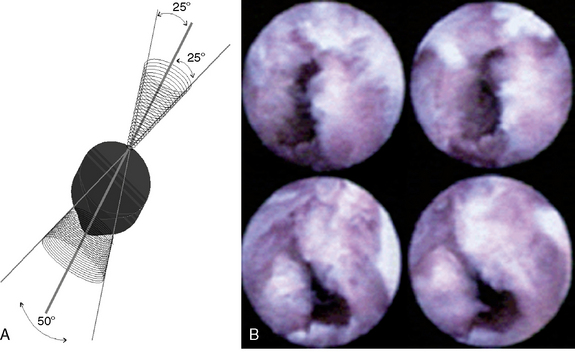
Endoscopic tower equipped with digital video monitor, DVD recorder, light source, and photo printer, with tri-chip digital camera system (Karl Storz, Tuttlingen, Germany) (Fig. 24-2) Thoracic operating endoscope (3.5-mm 6-degree) and diagnostic endoscopes (2.5-mm 0-degree and 30-degree) (Karl Storz)
Thoracic operating endoscope (3.5-mm 6-degree) and diagnostic endoscopes (2.5-mm 0-degree and 30-degree) (Karl Storz) Thoracic discectomy sets (2.5- and 3.5-mm) (Blackstone Medical, Inc., Springfield, MA) with short and long discectomes
Thoracic discectomy sets (2.5- and 3.5-mm) (Blackstone Medical, Inc., Springfield, MA) with short and long discectomes More aggressively toothed trephines used for spurs and spondylitic ridges at the anterior and posterior disc space (Karl Storz)
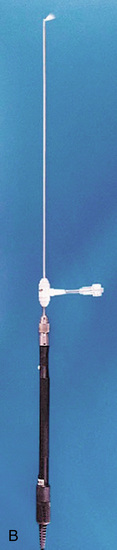
More aggressively toothed trephines used for spurs and spondylitic ridges at the anterior and posterior disc space (Karl Storz) Holmium:yttrium-aluminum-garnet (Ho:YAG) laser generator (Trimedyne, Inc., Irvine, CA) with and 550-μm holmium bare fiber with flat-tip right-angle (side-firing) probe (Fig. 24-3)
Holmium:yttrium-aluminum-garnet (Ho:YAG) laser generator (Trimedyne, Inc., Irvine, CA) with and 550-μm holmium bare fiber with flat-tip right-angle (side-firing) probe (Fig. 24-3)Preoperative preparation
Anesthesia
 Local anesthesia with monitored IV conscious sedation is used; restless patients may be given general anesthesia
Local anesthesia with monitored IV conscious sedation is used; restless patients may be given general anesthesiaPatient Positioning
The patient is positioned as follows for EATD [5,11–16]:
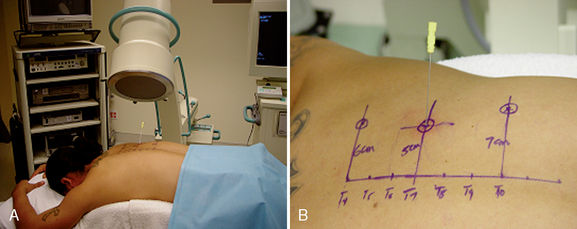
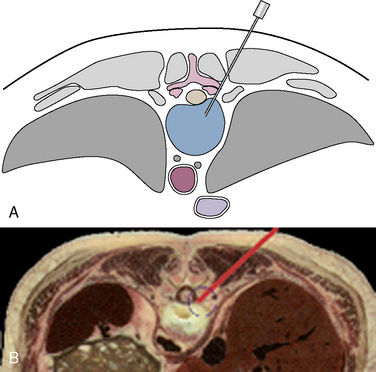
 The patient is positioned prone on the table with a radiolucent 20-degree angled sponge under the symptomatic side of the chest to angle it obliquely upward (Fig. 24-1A). The arms are supported on arm boards over the head.
The patient is positioned prone on the table with a radiolucent 20-degree angled sponge under the symptomatic side of the chest to angle it obliquely upward (Fig. 24-1A). The arms are supported on arm boards over the head.Fluoroscopy and Neurophysiologic Monitoring
The following instruments and equipment are used for monitoring and visualization during EATD [5,11–16]:
 Digital C-arm fluoroscopy is used in anteroposterior and lateral planes to control the placement of all instruments throughout the operation (see Fig. 24-1A).
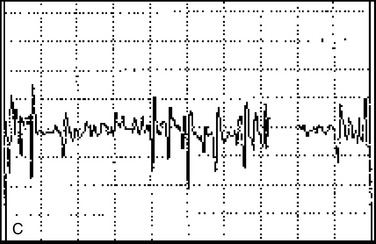
Digital C-arm fluoroscopy is used in anteroposterior and lateral planes to control the placement of all instruments throughout the operation (see Fig. 24-1A). Electromyography needles are placed for neurophysiologic monitoring within the areas of distribution of the nerve roots from the spinal levels being operated on, to provide continuous neurophysiologic-neuromuscular monitoring throughout the procedure for added safety.
Electromyography needles are placed for neurophysiologic monitoring within the areas of distribution of the nerve roots from the spinal levels being operated on, to provide continuous neurophysiologic-neuromuscular monitoring throughout the procedure for added safety.Procedure
Localization and Point of Entry
Localization of structures and point of entry are established as follows [5,11–16]:
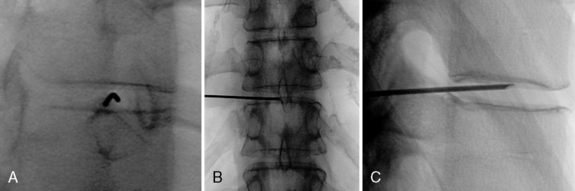
Alternately, with sterile technique, the level of the disc can be accurately identified by insertion of an 18-gauge spinal needle into a disc under fluoroscopic guidance (see Fig. 24-1B).
Surgical Technique
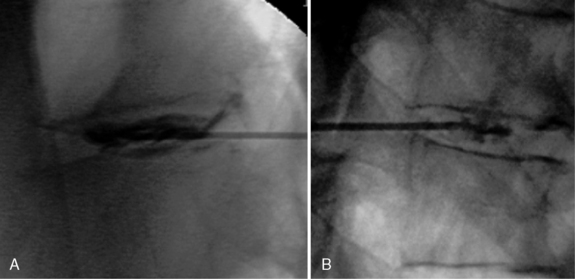
The surgical technique for EATD is as followws [5,11–16]:
Table 24.1 Laser Settings for Thoracic Laser Thermodiscoplasty*
| Stage | Watts | Joules |
|---|---|---|
| First | 10 | 500 |
| Second | 5 | 300 |
* Nonablative levels of laser energy are used—at 10 Hz for 5 seconds on and 5 seconds off.
Postoperative Management
Patients should receive a neurologic examination prior to leaving the operating room; upright portable chest radiographs are obtained in the recovery room to rule out pneumothorax. Ambulation begins immediately after recovery, and patients are usually discharged 1 hour after surgery. Patients are told that they may shower the following day; also that it may be helpful to apply an ice pack and that mild analgesics and muscle relaxants are required at times. A progressive exercise program is begun the second postoperative day. Usually patients are allowed to return to work in 1 to 2 weeks, provided heavy labor and prolonged sitting are not involved. Most patients found this procedure to be beneficial [5,11–16].
Complications
The complications of EATD, as well as their prevention or treatment, are as follows [5,11–17]:
Neural injury is extremely rare with EATD; no spinal cord injuries have been reported. Nerve root injury (intercostal nerve) causing intercostal neuralgia, or chest pain, though possible, can be avoided with the use of intraoperative electromyographic/neurophysiologic monitoring [22] of the intercostal muscles at and immediately below the operated levels. With use of direct endoscopic visualization, intercostal injuries related to open chest surgery and thorascopic surgery can be avoided. No nerve injuries were noted in 300-plus cases at our center. The initial spinal needle placement can be onto the posterior, superior surface of the rib into the “safety zone” at the neuroforamen to avoid the intercostal nerve lying in the inferior surface of the rib, in the costal groove. This maneuver and observing the strict boundaries of the interpedicular lines protect the spinal cord.
A thorough knowledge of the procedure and surgical anatomy of the thorax and thoracic spine, careful selection of patients, and preoperative surgical planning with appropriate diagnostic evaluations facilitate EATD and prevent and avoid potential complications. All the potential complications of open approaches for thoracic disc surgery are possible but are either rare or much less frequent in EATD, in which no rib resection or deliberate collapse of the lung is required [5,11–17].
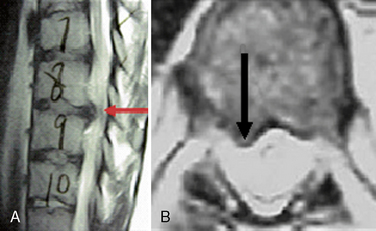
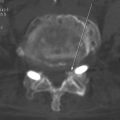
CASE STUDY 24.1
As the result of an auto accident, a 39-year-old man experienced intractable thoracic spinal pain and right T8 radiculopathy along the right lower chest wall radiating anteriorly. Neurologic examination revealed moderate parathoracic T8 and T9 vertebral muscle tenderness and muscle spasm as well as a moderate decrease in pain and touch sensation along the right T8 dermatome. Magnetic resonance imaging of the thoracic spine demonstrated a large (4-mm) T8-T9 disc herniation toward the right (Fig. 24-11). Endoscopy-assisted thoracic T8 microdiscectomy gave the patient immediate relief of all pain and symptoms.
1. Savitz M., Alli B., Chiu J. History of minimalism in spinal medicine and surgery. In: Savitz M., Chiu J., Rauschning W., Yeung A., editors. The Practice of Minimally Invasive Spinal Technique. 2005 ed. New City, NY: AAMISS Press; 2005:2-16.
2. Jaikumar S., Kim D., Kam A. History of minimally invasive spine surgery. Neurosurgery. 2002;51(Suppl. 2):1-14.
3. Perez-Cruet M., Fessler R., Perin N. Review: Complications of minimally invasive spinal surgery. Neurosurgery. 2002;51(Suppl. 2):26-36.
4. Dickman C., Mican C. Thoracoscopic approaches for the treatment of anterior thoracic spinal pathology. Barrow Neur Inst Quart. 1996;12:4-19.
5. Chiu J. Posterolateral endoscopic thoracic discectomy. In: Kim D., Fessler R., Regan J., editors. Endoscopic Spine Surgery and Instrumentation. New York: Thieme; 2004:125-136.
6. Nicholas T., Curtis A.D. Current management of thoracic disc herniation. Cont Neurosurg. 1996;18:1-7.
7. Chiu J., Clifford T., Princenthal R. The new frontier of minimally invasive spine surgery through computer assisted technology. In: Lemke H.U., Vannier M.N., Invamura R.D., editors. Computer Assisted Radiology and Surgery. New York: Springer-Verlag; 2002:233-237.
8. Simpson J.M., Silveri C.P., Simeone F.A., et al. Thoracic disc herniation: Re-evaluation of the posterior approach using a modified costotransversectomy. Spine. 1993;18:1872-1877.
9. Schellhas K.P., Pollei S.R., Dorwart R.H. Thoracic discography: A safe and reliable technique. Spine. 1994;18:2103-2109.
10. Chiu J., Clifford T., Greenspan M. Percutaneous microdecompressive endoscopic cervical discectomy with laser thermodiskoplasty. Mt Sinai J Med. 2000;67:278-282.
11. Chiu J., Clifford T., Sison R. Percutaneous microdecompressive endoscopic thoracic discectomy for herniated thoracic discs. Surg Technol Int. 2002;10:266-269.
12. Chiu J., Clifford T. Percutaneous endoscopic thoracic discectomy. In: Savitz M.H., Chiu J.C., Yeung A.D., editors. The Practice of Minimally Invasive Spinal Technique. Richmond, VA: AAMISMS Education, LLC; 2000:211-216.
13. Chiu J., Clifford T. Posterolateral approach for percutaneous thoracic endoscopic discectomy. J Minim Invas Spinal Tech. 2001;1:26-30.
14. Chiu J., Clifford T. Microdecompressive percutaneous discectomy: Spinal discectomy with new laser thermodiskoplasty for non-extruded herniated nucleus pulposus. Surg Technol Int. 1999;8:343-351.
15. Chiu J. Posterolateral endoscopic thoracic microdiscectomy. In Proceedings of World Spine III: The Third Interdisciplinary Congress on Spine Care. Brazil: Rio de Janeiro; 2005. July 31–Aug 3
16. Chiu J. Potential complications of minimally invasive spine surgery and their avoidance. Khamlichi, A. (Ed.). 13th World Congress of Neurological Surgery, Marrakesh (Morocco), June 19–24, 2005: International Proceedings. Bologna, Italy: Medimond; 2005:69-76.
17. Boriani S., Biagini R., Delure F. Two level thoracic disc herniations. Spine. 1994;21:2461-2466.
18. Chiu J., Savitz M.H. Use of laser in minimally invasive spinal surgery and pain management. In: Kambin P., editor. Arthroscopic and Endoscopic Spinal Surgery—Text and Atlas. 2nd ed. Totowa, NJ: Humana Press; 2005:259-269.
19. Dickman C., Mican C. Multilevel anterior thoracic discectomies and anterior interbody fusion using a microsurgical thoracoscopic approach: Case report. J Neurosurg. 1996;84:104-109.
20. Shikata J., Yamamuro T., Kashiwagi N. Multiple thoracic disc herniations: Case report. Neurosurgery. 1988;22:1068-1070.
21. Chiu J., Clifford T. Multiple herniated discs at single and multiple spinal segments treated with endoscopic microdecompressive surgery. J Minim Invas Spinal Tech. 2001;l:15-19.
22. Chiu J., Yeung A., Lekht Z. Monitoring during percutaneous endoscopic discectomy. In: Savitz M., Chiu J., Rauschning W., Yeung A., editors. The Practice of Minimally Invasive Spinal Technique. 2005 ed. New City, NY: AAMISS Press; 2005:597-602.