CHAPTER 14 Endoscopic Distal Biceps Repair
Tears of the distal biceps tendon represent a diagnostic and imaging challenge for the orthopedic surgeon and sports physician.1–8 Complete tears of the distal tendon account for approximately 3% of all tears involving the muscle, and partial tears are less common, although their exact incidence is unknown.1–5 The symptoms may be subtle (e.g., antecubital pain) and signs difficult to illicit (e.g., weakness of elbow flexion and supination). Physicians who remain alert to the possibility are most likely to suspect the diagnosis. Use of correct imaging and of surgical endoscopy can lead to the correct diagnosis and management of the condition.
ANATOMY
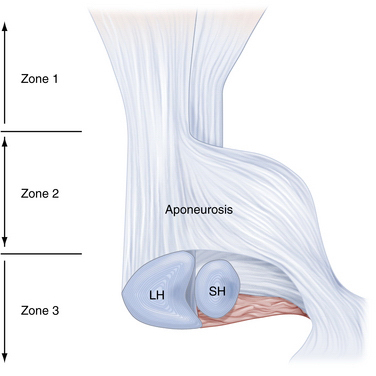
Biceps brachii is the most superficial of the muscles in the anterior compartment of the arm, and it has two heads of origin. It acts across three articulations: the shoulder, the elbow, and the proximal radioulnar joint.9 The short head takes a tendinous origin from the tip of the coracoid process of the scapula, immediately lateral to the origin of the coracobrachialis muscle. The long head arises from the supraglenoid tubercle and adjacent glenoid labrum. The two tendons expand into fleshy fusiform bellies, held together by loose epimysial tissue.9,10 As they traverse parallel through the upper arm, the belly of the short head always remains to the ulnar side and the long head to the radial side.9 It was once held that the two bellies fused below their main convexity, just above the elbow joint,4,9,10 but anatomic cadaver studies have revealed a variable amount of interdigitation.10 Eames and Bain10 also described the distal tendon as having two distinct components held together by loose adventitia, one arising from each belly. Eames and Bain10 further divide the distal biceps tendon into three zones.
In zone 1, the pre-aponeurosis, a variable amount of muscular interdigitation of the two bellies occurs, with many cadavers showing none at all (7 of 17 specimens). Where it was present, the raphe was easily overcome by blunt finger dissection (Fig. 14-1).
Zone 2, the aponeurosis or lacertus fibrosus, consists of three layers. The superficial layer arises from the anterior, radial aspect of the long head at the level of the distal musculotendinous junction. It spreads distally and ulnarward, coursing anterior to the musculotendinous junction of the short head. The middle layer acts as a mesentery to the short head tendon, embracing it before it passes distally and ulnarward and merges with the superficial layer. The deep layer arises from the deep radial aspect of the long head and sweeps distally and ulnarward, deep to the short head tendon. The three layers subsequently merge and continue distally as a single aponeurosis. The lacertus fibrosus has wide and deep involvement in the flexor compartment of the forearm—it completely encircles the flexors and has fascial attachments, particularly to the ulnar flexors, and it incorporates the median nerve and brachial artery.10
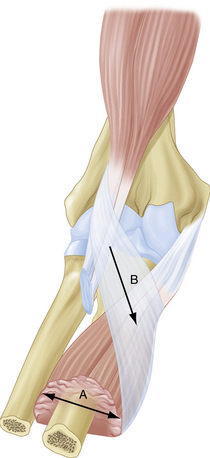
In zone 3, the post-aponeurosis, the two tendons continue distally past the lacertus fibrosus and insert onto the radial tuberosity. The distal biceps tendon footprint on the radial tuberosity is 2 × 14 mm.11 In all specimens, the long head tendon passed deep to the short and inserted more proximally.10 This point is also farthest away from the point of rotation of the radius. The tendon of the short head curves anterior to the long and inserts in a fanlike fashion on the distal portion of the radial tuberosity and extends distal to it (Fig. 14-2). With these different insertions, the long head provides greater supination power, and the short head may provide more flexion power, which can help in clinical evaluation of partial tears to localize the tear by power testing.
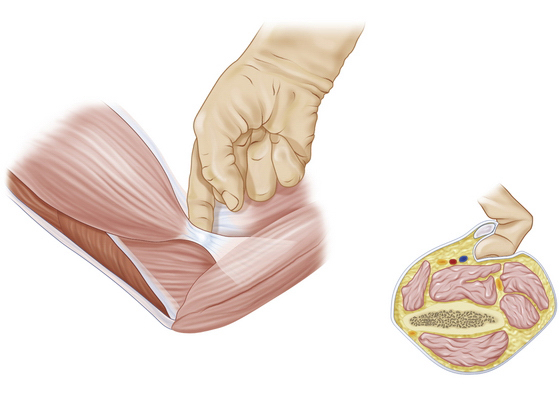
Surrounding the tendon insertions is the bicipitoradial bursa.7,8,10,12 This structure is of great clinical importance in endoscopic evaluation of the distal tendon after injury. Eames and Bain10 found that the bursa encircled the tendons in all cases of their anatomic study. They observed that the bursa was easily distended by approximately 7 mL of normal saline from its deep radial side. The bursa drapes over the tendons, is teardrop shaped, and lies between the groove in the brachialis muscle and the distal tendons with the elbow extended and between the proximal radius and biceps tendon during pronation (Fig. 14-3).8,10
PATIENT EVALUATION
History and Physical Examination
Complete tears of the distal biceps tendon are uncommon, accounting for 3% of all tears involving the biceps.1–5 Partial tears are less common, but descriptions of this type of tear in the literature is increasing, probably as recognition of the pathology improves. Maintaining clinical suspicion of tears of the distal tendon (particularly partial tears) is likely key, particularly in the presence of sometimes very subtle clinical signs.
The age of presentation of patients with partial tears is slightly higher than that of those with complete tears—mid-50s and mid-40s, respectively.10,13 Almost all complete tears reported in the literature have occurred in male patients, whereas partial tears have been reported for both sexes.1–3
In complete and partial tears, the dominant limb is most often affected.4 In the case of complete tears, the injury occurs through sudden, forced, eccentric contraction of the biceps muscle, such as a sudden and unexpected extension load on a flexed elbow.4,6,10,13 Partial tears are associated with mixed etiologic factors.
Partial tears are caused by acute traumatic and chronic degenerative mechanisms.1,2,4,13 The mechanism of injury of acute partial tears is the same as for complete tears, but the force causing the injury is interrupted before complete avulsion occurs. Various mechanisms for degeneration have been proposed, including abnormal friction forces, impingement, repetitive strain with supination and pronation, and vascular changes in the tendons.4,10 It is our experience that degenerate tears of the biceps tendon can occur in the older patient and occurs more often in female patients.
The patient often reports pain in the antecubital fossa, weakness of flexion or supination and possible limitation of elbow range of motion, particularly flexion.1-6,8,10,13 Inspection may reveal swelling and bruising at the antecubital fossa. This can be an inconsistent finding, particularly in partial tears.4 Tenderness is elicited on palpation of the antecubital fossa. Pain with resisted supination is a common finding. With complete ruptures, the distal biceps tendon is not palpable in the antecubital fossa, and the physician must be careful that the biceps tendon is being examined, not mistakenly an intact lacertus fibrosus.
The hook test for distal biceps was described by O’Driscoll and colleagues.14 While the patient actively supinates with the elbow flexed 90 degrees, a positive hook test result permits the examiner to hook his or her index finger under the intact biceps tendon from the lateral side. With an abnormal hook test result, indicating distal avulsion, there is no cordlike structure under which the examiner may hook a finger (Fig. 14-4).14 The hook test is highly sensitive and specific for complete tears of the distal biceps tendon (as good as or better than magnetic resonance imaging), and it is easy to perform.
A large area of bursitis can compress the median nerve3 and may produce neurologic signs distally. Imaging can differentiate other diagnoses in the absence of trauma (e.g., antecubital lipoma, other tender lesions) from distal biceps tendinitis or bursitis.
Diagnostic Imaging
Plain radiography usually is not helpful in the diagnosis of distal biceps tendon tears. Some calcification of degenerate tendons may be seen at the radial tuberosity, but this is not a reliable diagnostic finding and has been reported only for complete tears.15
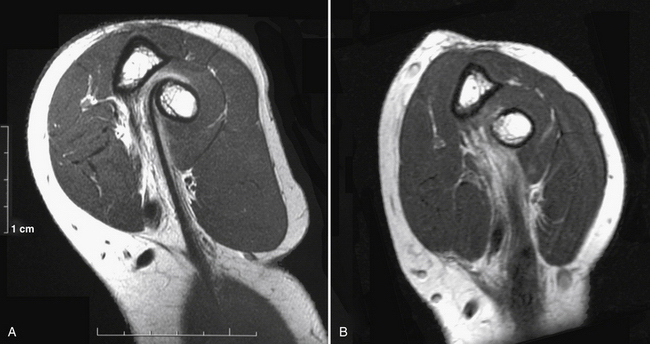
Traditional positioning techniques for MRI of the distal biceps tendon yielded images that were difficult to interpret,5,6 because axial images are obtained from an extended arm for a tendon with an oblique course in the antecubital fossa. Giuffre and Moss5 described a method for optimal patient positioning that allows full-length views of the biceps brachii tendon from the musculotendinous junction (i.e., Eames and Bain’s zone 1) to its insertion on the radial tuberosity (Eames and Bain’s zone 3) in one or at most two sections.5,6,8 This position has become known as the flexed abducted supinated (FABS) view, and it is used in addition to conventional views of the biceps brachii (Fig. 14-5).5,6
The patient is positioned prone with the shoulder abducted 180 degrees and the arm positioned adjacent to the head. The elbow is then flexed to 90 degrees, with the forearm supinated and the patient’s thumb pointing upward. A shoulder phased-array coil is placed at the elbow, making it the center-of-magnet position; this makes fat-suppressed imaging optimal, allowing improved visualization of small amounts of fluid (Fig. 14-6).6
Ultrasonography has several advantages over other modalities. It is far cheaper than MRI and can be performed in most clinical circumstances. It can be used to confirm continuity of the distal tendon or measure changes in the caliber of the tendinous structures. Dynamic ultrasound evaluation of the distal tendon can differentiate partial from complete ruptures.6 Peritendinous fluid, such as blood or edema, can be visualized.6 However, it is operator dependent and therefore less reproducible. Imaging is often performed from the antecubital fossa and volar surface of the elbow, where the anatomic structures are easily palpable. Positioning the forearm in supination brings the distal tendon and its insertion on the radial tuberosity into view on the medial aspect of the radius.6 Dynamic assessment can then be performed by moving through slight flexion-extension and supination-pronation ranges of motion. The pronator window can be used from the medial side of the proximal forearm through the pronator teres muscle bed (Fig. 14-7).
TREATMENT
Indications and Contraindications
A complete tear of the distal biceps tendon can be diagnosed clinically with more ease than partial tears, and imaging can aid in clarifying the diagnosis in both instances. Endoscopic investigation of the bicipitoradial bursa allows dynamic assessment of the distal biceps tendon, giving a clear magnified view of the pathology by a comparatively minimally invasive procedure.8,12
Patients who have been diagnosed with a complete tear of the distal biceps tendon are usually managed with an open procedure to repair the torn tendon and therefore do not require endoscopic evaluation. For patients who have been diagnosed with a partial tear or tenosynovitis of the distal biceps tendon, we perform an endoscopic assessment. This approach for patients with abnormal anatomy, such as from previous injury or surgery at the elbow and antecubital fossa, is relatively contraindicated.12 The functional demands and comorbidities of the patient must also be taken into account.
Treatment Alternatives
Although complete tears of the distal biceps tendon require immediate surgical repair to maximize functional outcome, the same may not be true of partial tears.3,4,8,10,12 Quantifying the percentage of tendon involved in the injury is important. The literature states that tears involving less than 50% of the total insertional footprint do not require surgical reattachment because no functional deficit results.3,12 Tears involving more than 50% of the insertional footprint require formal surgical division and reattachment using standard techniques.1-3,8,12,13,16 What is not known is the functional outcomes of tears of long head versus short head tears with regard to operative or nonoperative management.8 Distal biceps endoscopy allows further assessment of the pathology and treatment of partial tears. Classification of the injury can aid management decisions (Table 14-1).
TABLE 14-1 Classification of Insertional (Zone 3) Distal Biceps Tendon Injury
| Grade | Injury | Signs | Examples | Treatment |
|---|---|---|---|---|
| 0 | Distal biceps tendinosis | Pain on resisted supination and flexion |
Conservative Management
Tears of less than 50% of the insertional footprint may not require initial surgical management.3,8,12 Bourne and Morre1 treated clinically diagnosed partial tears with 3 weeks of immobilization, 3 weeks of flexion, and then assisted brace with modified duties for 3 months. Durr and colleagues3 reported treatment with a plaster splint in neutral for 2 weeks in conjunction with systemic anti-inflammatory drugs, followed by physiotherapy. This study found that conservative management of these injuries was successful for patients not requiring forearm strength for professional activities.3 Local anesthetic injected into the distal tendon insertion site has had satisfactory effects.3 Each of these series reports decreased pain and functional improvement over the course of several months after the initial injury.
Arthroscopic Technique
The benefits of immediate surgical repair for complete ruptures are well established.4 Through the course of its evolution, surgical treatment of partial tears has involved double- and single-incision open techniques, which were used to complete the partial tear, débride the insertion and torn tendon, and proceed with primary anatomic repair of tendon to bone. Débridement alone of the tendon with a tear greater than 50% of its fibers is not successful.1,4,15 The various techniques described over the years are directed at reducing the complications encountered by repair (see Table 14-1).16
Endoscopy and Partial Tears
Endoscopic investigation of the bicipitoradial bursa enables dynamic assessment of the distal biceps tendon (which cannot be achieved with open techniques), giving a clear, magnified view of the pathology by means of a comparatively minimally invasive procedure.8,12
Our preferred technique8,12 consists of endoscopy of the bicipitoradial bursa performed with the patient under general anesthesia. The arm is exsanguinated, and a proximal tourniquet is inflated to 250 mm Hg. The arm is positioned in extension and supination. A small (2.5-cm), longitudinal incision is made over the palpable biceps tendon 2 cm distal to the elbow crease (Fig. 14-8). The lateral cutaneous nerve of the forearm needs to be identified and protected. Using this mini-open approach, the distal biceps tendon and its bursa are identified with finger dissection. The bursa is insufflated with 7 to 10 mL of normal saline, and a small entry point is made on its radial side at the apex for the arthroscope. Constant insufflation of the bursa is achieved by gravity feed only to avoid excessive extravasation into the forearm. Keeping radial to the entry point enables the surgeon to avoid damaging the median nerve and brachial artery that lie on the ulna aspect of the tendon.
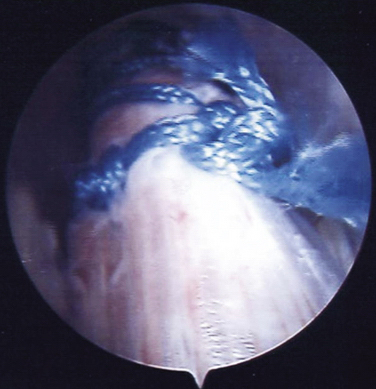
FIGURE 14-8 Arthroscopic view of the repaired tendon.
(From Sharma S, MacKay G. Endoscopic repair of distal biceps tendon using an EndoButton. Arthroscopy. 2005;21:897.e891-897.e894.)
The tendons are identifiable in the field of view and can be followed distally to their insertion into the radial tuberosity, with the long head tendon inserting proximally and the short head distally.8–10,12 Because the bursa encircles the tendons at their insertion, evaluation can be obtained for tendon patency and for any synovitis and bursitis. The tendons can be viewed dynamically through forearm rotation or with traction applied to a nylon tape placed around the tendon. A hook probe may be introduced through the same portal to examine the distal insertion. A practice point is to appreciate that the bursa may be adherent to tendon on the ulnar side, and it may not inflate on this side in some individuals. Carefully reviewing the tendon, the extent (percentage) of rupture can be determined (Fig. 14-9).
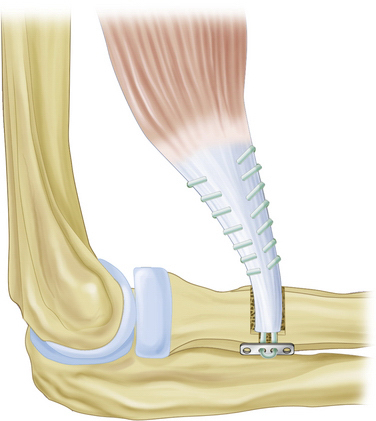
FIGURE 14-9 EndoButton technique for repair of a distal biceps tendon tear.
(Modified from Bain GI, Prem H, Heptinstall RJ, Verhellen R, Paix D. Repair of distal biceps tendon rupture: a new technique using the Endobutton. J Shoulder Elbow Surg. 2000;9:120-126.)
After the extent of injury has been determined, further treatment decisions can be made. Synovitis and tears involving less than 50% of the insertion may be débrided by employing an oscillating chondrotome through the same portal. To avoid damaging neurovascular structures, a full-radius resector without teeth and without suction is used, minimizing the chance of these structures being suctioned into the resector’s aperture.12 By moving the forearm through supination and pronation during the procedure, the surgeon can inspect the entire area of injury and débride it under endoscopic vision. Tears found to be larger than 50% of the tendon insertion can be formally repaired with an open technique by extending the existing endoscopy incision.
A systematic review of repair techniques concluded that EndoButton repairs consistently performed biomechanically better than other repair methods.17 The same review found that a significantly larger proportion of unsatisfactory results were obtained for the two-incision approach group for repairs to the distal biceps tendon. It appears that single-incision repairs using an EndoButton give the best results in terms of biomechanical stability and strength and produce fewer unsatisfactory results.
Bain and colleagues17 described a technique for repair using the EndoButton (Accufex Microsurgical, Mansfield, MA). It is a relatively simple technique that minimizes many of the complications associated with repair, such as stiffness, radioulnar synostosis, and weakness of supination (Fig. 14-10).16 The superior mechanical strength of this technique compared with other methods of repair allows early active mobilization.
Endoscopy and Complete Tears
Sharma and MacKay18 described an endoscopic technique for repair of complete tears using the EndoButton technique. The technique is performed with the patient under general anesthesia and with the patient’s arm on an arm board. A 1.5-cm, longitudinal incision is made in the midline of the anterior aspect of the arm at a point 5 cm proximal to the transverse anterior elbow crease. The ruptured distal end of the biceps tendon is then delivered out of the wound. The ruptured end of the tendon is freshened and sutured to a fixed-loop 20-mm EndoButton using a continuous loop of no. 5 Ethibond (Ethicon, Somerville, NJ), which is interlocked and secured 3 cm proximal to the end of the ruptured tendon.18 Leading and trailing sutures are applied to the EndoButton as previously described.
The EndoButton is toggled as previously described, and the endoscope is again introduced into the portal to confirm reattachment. The native footprint of the biceps tendon is ulnar in the fully supinated forearm. With the cannulated technique described by Sharma and McKay,18 it is not possible to place the tunnel at the ulnar side, in addition to risking the radial nerve on the posterolateral forearm. As a consequence, we continue to use the open repair technique for distal biceps repair as originally described.
Postoperative Rehabilitation
Partial tears of the distal biceps tendon that undergo endoscopic débridement only may be mobilized as comfort allows immediately postoperatively.12 Heavy lifting and resistance activities should be avoided for 6 weeks, and a short course of nonsteroidal anti-inflammatory drugs may be considered for patients with considerable synovitis or those who have a history of heterotopic ossification.12 Strengthening activities may commence after 6 weeks.
Partial or complete tears that have undergone repair using the EndoButton technique are routinely provided with a sling for comfort.8,16 After the first postoperative appointment at 1 week, the patient is encouraged to perform range-of-motion exercises as tolerated. The patient is advised not to perform heavy lifting or heavy-resistance work for 3 months, but light duties can commence at 3 weeks.8,16 Nonsteroidal anti-inflammatory drugs are not routinely used because they may compromise tendon healing, but they should be considered for patients with considerable synovitis or those who have a history of heterotopic ossification.12
CONCLUSIONS
We suggest that distal biceps tendon endoscopy be undertaken only by surgeons who are thoroughly familiar with elbow anatomy and who have a high proficiency with endoscopic equipment.8 The proximity of major neurovascular structures to working portals must be appreciated.
It is unknown whether short or long head distal biceps tendon tears are important subgroups with regard to nonoperative management. The surgeon must to take into account patient factors (e.g., age, occupation) and tendon tear factors (e.g., percentage, dominant arm, chronic or acute injury) before a final decision is made about treatment.8
1. Bourne MH, Morrey BF. Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 1991;271:143-148.
2. Rokito AS, McLaughlin JA, Gallagher MA, Zuckerman JD. Partial rupture of the distal biceps tendon. J Shoulder Elbow Surg. 1996;5:73-75.
3. Durr HR, Stabler A, Pfahler M, et al. Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 2000;374:195-200.
4. Bernstein AD, Breslow MJ, Jazrawi LM. Distal biceps tendon ruptures: a historical perspective and current concepts. Am J Orthop. 2001;30:193-200.
5. Giuffre BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol. 2004;182:944-946.
6. Chew ML, Giuffre BM. Disorders of the distal biceps brachii tendon. Radiographics. 2005;25:1227-1237.
7. Sassmannshausen G, Mair SD, Blazar PE. Rupture of a bifurcated distal biceps tendon. A case report. J Bone Joint Surg Am. 2004;86A:2737-2740.
8. Bain GI, Johnson LJ, Turner PC. Treatment of partial distal biceps tendon tears. Sports Med Arthrosc. 2008;16:154-161.
9. McMinn RMH. Last’s Anatomy, Regional and Applied, 9th ed. New York, NY: Churchill Livingstone; 2003.
10. Eames MH, Bain GI, Fogg QA, van Riet RP. Distal biceps tendon anatomy: a cadaveric study. J Bone Joint Surg Am. 2007;89:1044-1049.
11. Mazzocca AD, Burton KJ, Romeo AA, et al. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35:252-258.
12. Eames MHA, Bain GI. Distal biceps tendon endoscopy and anterior elbow arthroscopy portal. Tech Shoulder Elbow Surg. 2006;7:139-142.
13. Vardakas DG, Musgrave DS, Varitimidis SE, et al. Partial rupture of the distal biceps tendon. J Shoulder Elbow Surg. 2001;10:377-379.
14. O’Driscoll SW, Goncalves LB, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35:1865-1869.
15. Ramsey ML. Distal biceps tendon injuries: diagnosis and management. J Am Acad Orthop Surg. 1999;7:199-207.
16. Bain GI, Prem H, Heptinstall RJ, et al. Repair of distal biceps tendon rupture: a new technique using the EndoButton. J Shoulder Elbow Surg. 2000;9:120-126.
17. Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: a systematic review. Am J Sports Med. 2008;36:1618-1624.
18. Sharma S, MacKay G. Endoscopic repair of distal biceps tendon using an EndoButton. Arthroscopy. 2005;21:897.e1-897.e4.