Chapter 43 Endoscopic coblation lingual tonsillectomy
1 INTRODUCTION
For the clinician and surgeon treating patients with obstructed sleep apnea and related maladies, the retrolingual airway is of much importance. This area, often difficult to examine and identify as an area of concern, has recently been the site of much academic and surgical attention. For with its difficult location comes increased complexity in surgical cure, plagued with both intraoperative and postoperative challenges. Although the palatal–pharyngeal area is often the site of primary obstruction in patients with sleep apnea, there are often areas of secondary blockage, andthe tongue base may be an area of interest with the added concern of hypertrophic lingual tonsils.
2 PATIENT SELECTION
Obstruction may not be the only presenting sign of hypertrophic lingual tonsils. Symptoms may be classified into two main categories, resulting from problems with either inflammation and infection or hypertrophy and hyperplasia. Inflammation may present with dysphagia and odynophagia with complaints originating at the tongue base or suprahyoid region. These symptoms may occasionally result in lingual tonsillar abscess and recurrent epiglottitis.1–3 Hypertrophic or hyperplastic tonsils may plague the patient with dysphagia and globus. These patients may have increased symptoms in the supine position, with those afflicted with obstructive sleep apnea having a worsening obstructive process in the deeper stages of sleep. Interestingly, lingual tonsil enlargement is a relatively common finding in children with persistent obstructive sleep apnea following adenotonsillectomy,4 further intensifying the finding of compensatory lingual tonsil hypertrophy after such a procedure.
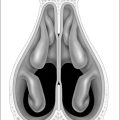
The differentiation of lingual tonsil and tongue base pathology is often difficult. Furthermore, the very definition of lingual tonsil hypertrophy has not been standardized. However, if the lingual tonsils are greater than ‘10 mm in diameter and abutting both the posterior border of the tongue and the posterior pharyngeal wall,’ they may be considered clearly enlarged, due to a known relationship to patients with obstructive sleep apnea.5 Determination between lingual tonsil hypertrophy and an enlarged tongue base is critical, for these two entities often require different therapies with both needing attention. Careful history taking and physical examination when combined with ancillary studies may help the surgeon successfully treat the patient with retrolingual pathology.
There are multiple descriptions of how to surgically address the lingual tonsils, including scalpel, electrocautery, snares, laser and removal with the suction debrider.6–8 However, these procedures are often fraught with difficult exposure, painstaking dissection, poor visualization, difficult hemostasis, excessive postoperative pain and possible airway edema. A recent report from Robinson et al. describes the novel technique of utilizing bipolar radiofrequency plasma excision, or the coblator, for direct visual removal of the lingual tonsil pad using suspension laryngoscopy and an operating microscope.9 Advantages of this technique include improved exposure, visualization and hemostasis with decreased postoperative edema and pain when compared to previously described techniques. However, after multiple cases, we find the suspension laryngoscopy and the use of the operating microscope to be burdensome and unnecessary. Of note, the laryngoscope is bulky, distorts the lingual anatomy and requires intraoperative adjustment and re-suspension. Also, even bivalved laryngoscopes may restrict full surgical access to the lateral portion of the tonsil, and may increase the risk of laryngoscope associated complications, including injury to the patient’s dentition, temporary dysgeusia and altered tongue mobility. Adding to the difficulty, use of the microscope is tedious and it only works in the straightforward position. Here, we offer our experience with endoscopic coblation lingual tonsillectomy. Being otolaryngologists, already comfortable with the increased visualization and applications offered from our endoscopes, why not apply these superior optics to surgery in a difficult spot?
Due to the difficulty in examining the retrolingual airway by the front-line primary care health provider, it is critical that the otolaryngologist be familiar with the different tools of preoperative assessment. Examination with laryngeal mirror and flexible endoscopy is critical, for these are the best methods of visualization. Finger palpation is also standard, for tongue base concerns may occasionally stem from foreign bodies or tumor. Visualization is also important in the clinical differentiation of lingual tonsil and tongue base musculature hypertrophy. Since these entities are treated differently, incorrect identification of the area of concern may lead to decreased treatment success. Enlarged lingual tonsils may appear with multiple enlarged follicles, soft to the touch and occasionally filling the vallecula to the point of glottis concealment from a posterior pushed epiglottis. One must characterize the space between the lingual tonsils posterior extent to the posterior oral and hypopharyngeal wall. The Mueller maneuver may add additional clues to the responsible levels of obstruction.10 Lateral neck radiographs may offer information on tongue position and relative size of the lingual tonsils;11 however, when in question, we find magnetic resonance imaging (MRI) with gadolinium enhancement to be crucial in imaging the tongue base. This modality, which characteristically enhances the lingual tonsils from tongue base musculature, helps to determine the nature of retrolingual obstruction, be it lingual tonsil hypertrophy or tongue base enlargement, while appropriately exposing other possibilities, such as tumor.12 If lingual tonsil hypertrophy is suspected, and there are no clinical contraindications, a short burst of oral steroids with re-examination in one week is another way to determine culpability of the lingual tonsil; if the retrolingual airspace widens, the lingual tonsils are likely the perpetrator. If there is no difference, suspect the tongue base. This method may provide a quicker and less expensive clinical method than MRI; however, the chosen modality is ultimately up to the clinician.
In addition, great care must be given to addressing the non-surgical treatments of lingual tonsil hypertrophy which is often due to allergies, sinusitis and gastroesophageal reflux, of which hypertrophy may be a presentingsign with the latter.5 Often, after appropriate medicinal treatment, such as with an empiric trial of proton pump inhibitors and/or topical nasal steroids, clinical improvement over 4–6 weeks may eradicate the need for surgery. Finally, polysomnogram is the gold standard exam for evaluating concerns of sleep disorder breathing. Extra cautionmust be given to patients with suspected neuromuscular abnormalities; hypotonia and related disorders (such as cerebral palsy and Down’s syndrome) may suffer from obstructive as well as central apnea.
3 OUTLINE OF PROCEDURE
Our method of lingual tonsillectomy synergies the technique recently described by Robinson9 (see Chapter 41)with the otolaryngologist’s utilizing endoscopic-assisted surgery. If dealing with obstructive retrolingual anatomy, standard anesthesia precautions are employed. Perioperative antibiotics and steroids are given. After placing the patient in proper Rose position, nasotracheal intubation is employed, and after proper position, a retraction 2.0 silk suture is placed in the anterior tongue. Multiple stitches may ultimately be necessary for improved retraction and visualization; these may even be placed later during the procedure. A standard rubber bite block keeps the mouth open and one or two rubber oronasal catheters may be placed to retract the soft palate if needed. A standard 70° sinus endoscope is placed periorally to directly view the lingual tonsil. The malleable Evac 70 tonsil and adenoid coblation wand is gently bent. The lingual tonsils are ablated under endoscopic guidance (setting 9 on ablate; Arthrocare Corp, ENTec Division, Sunnyvale, CA). The endoscope alone provides an excellent panoramic view of the lingual tonsil with virtually any patient body type. The procedure is dynamic; small changes in amount and direction of tongue retraction change the view and tension of the lingual tonsil and aid in a complete excision. The tonsil is ablated until the tongue musculature is encountered, and care is taken to avoid coblation of the epiglottis or other supraglottic structures. The addition of the endoscopic view enables intra-operative photos and video to be taken, as well as allowing others in the operating room the opportunity to observe the procedure. The ability of the anesthetist to see the resection adds extra benefits. Visualization of the airway often reveals a larger, improved airway at the conclusion of the case and may add confidence to involved providers if extubation is decided upon at the conclusion of the case.
4 POSTOPERATIVE MANAGEMENT AND COMPLICATIONS
We routinely extubate at the completion of the tonsillectomy, though this decision must be determined by the surgeon based on the individual characteristics of the patient, the observational hospital setting as well as one’s ownpreference. This decision may also change if other procedures are performed such as tongue base reduction or palatal procedures. Patients are observed for at least 24 hours postoperative in an intensive care setting, being given postoperative antibiotics and steroids. Close follow-up, as well as continued allergy and gastroesophageal reflux medicines, may be continued, as patients are symptomatically followed. If a complete excision is performed, regrowth is unlikely. Success depends on completeness of excision as well as the lingual tonsil’s role in preoperative symptoms such as globus or obstruction.
1. Elia JC. Lingual tonsillitis. Ann NY Acad Sci. 1959;82:52-56.
2. Newman RK, Johnson JT. Abscess of the lingual tonsil. Arch Otolaryngol Head Neck Surg. 1979;105:277-278.
3. Lewis M, McClay JE, Schochet P. Lingual tonsillectomy for refractory paroxysmal cough. Int J Pediatr Otorhinolaryngol. 2000;53:63-66.
4. Fricke BL, Donnelly LF, Shott SR, et al. Comparison of lingual tonsil size as depicted on MR imaging between children with obstructive sleep apnea despite previous tonsillectomy and adenoidectomy and normal controls. Pediatr Radiol. 2006;36(6):518-523.
5. Carr MM, Nagy ML, Pizzuto MP, et al. Correlation of findings at direct laryngoscopy and bronchoscopy with gastroesophageal reflux disease in children: a prospective study. Arch Otolaryngol Head Neck Surg. 2001;127(4):369-374.
6. Yonekura A, Kawakatsu K, Suszuki K, et al. Laser midline glossectomy and lingual tonsillectomy as treatments for sleep apnea syndrome. Acta Otolaryngol Suppl. 2003;550:56-58.
7. Wouters B, van Overbeek JJ, Buiter CT, et al. Laser surgery in lingual tonsil hyperplasia. Clin Otolaryngol Allied Sci. 1989;14:291-296.
8. Conache ID, Meikle D, O’Brien C. Tracheostomy. lingular tonsillectomy and sleep-related breathing disorders, Br J Anaesth. 2002;88:724-726.
9. Robinson S, Ettema SL, Brusky L, et al. Lingual tonsillectomy using bipolar radiofrequency plasma excision. Otolaryngol Head Neck Surg. 2006;134(2):328-330.
10. Faber CE, Grymer L. Available techniques for objective assessment of upper airway narrowing in snoring and sleep apnea. Sleep Breath. 2003;7(2):77-86.
11. Bower CM. Lingual tonsillectomy. Operative Tech Oto. 2005;16:238-241.
12. Shott SR, Donnelly LF. Cine magnetic resonance imaging: evaluation of persistent airway obstruction after tonsil and adenotonsillectomy in children with Down syndrome. Laryngoscope. 2004;114:1724-1729.