Emergency Oxygen Administration
Emergency medical oxygen (O2) administration is a critical part of wilderness emergency care. Every provider of wilderness medicine must be familiar with the therapeutic value, indications, hazards, equipment, and technique of oxygen administration (Box 11-1).
Indications
Indications for the use of supplemental O2 include (but are not limited to) the following:
• Hypoxemia (low blood oxygen)
• Pulmonary gas exchange impairment as a result of trauma, edema, asthma, infection, embolism
• Acute myocardial infarction, cerebrovascular accident
• Decompression illness, including both decompression sickness and arterial gas embolism
• High-altitude pulmonary edema
Contraindications
Pulmonary Oxygen Toxicity
Prolonged exposure to high concentration of O2 is also associated with the following:
1. Intratracheal and bronchial irritation
2. Substernal or retrosternal burning
3. Chest tightness, cough, and dyspnea
4. Continued prolonged exposure to high O2 concentrations may result in adult respiratory distress syndrome. Early pulmonary changes associated with pulmonary O2 toxicity are reversible with cessation of O2 therapy.
Equipment
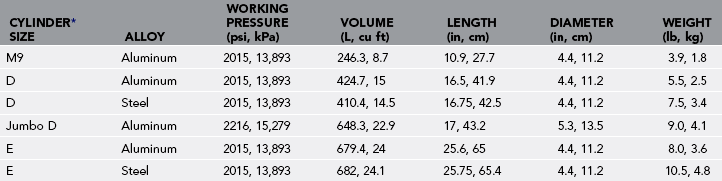
Medical O2 cylinders or tanks are made of aluminum or steel and come in a variety of sizes (Table 11-1). In the United States, any pressure vessel that is transported on public roads is subject to U.S. Department of Transportation (DOT) regulations. The DOT requires that cylinders be visually and hydrostatically tested every 5 years and either be destroyed if they fail or be stamped and labeled appropriately if they pass. Gas suppliers will not fill cylinders that have not been appropriately tested and stamped. The working pressure of steel medical O2 cylinders is 2015 psi (13,893 kPa). The working pressure of aluminum O2 cylinders is either 2015 psi or 2216 psi (13,893 kPa or 15,279 kPa), depending on the type. High-pressure, lightweight cylinders used for high-altitude climbing are not discussed here.
Devices for Ventilation of Nonbreathing Patients
FROPV/Positive Pressure Demand Valve
1. Older-style positive pressure demand valves (PPDVs), such as the LSP 063-05 or Elder CPR/demand valve, function both in positive pressure mode (pushing the button to ventilate a nonbreathing patient) and in demand mode.
2. When used in demand mode, the recipient simply holds the mask to his or her face. When he or she inhales, negative pressure in the mask and demand valve opens the valve and gas flows. The flow of gas stops when the person stops inhaling or exhales, similar to other demand regulators such as scuba and aviation regulators.
3. One misconception is that PPDVs will easily cause pulmonary overpressurization injury, and thus they have fallen out of favor with some health care providers. In fact, in positive pressure mode, all PPDVs manufactured in the United States are required to have an overpressure relief valve that stops the flow of gas at a pressure of 55 to 65 cm H2O (a little more than half the pressure required to overpressurize a human lung). This is done to avoid pulmonary overpressurization injury. The most recent model, the MTV-100 FROPV introduced in 1993, has two overpressure relief valves, the first set at 60 cm H2O and the second at 65 to 80 cm H2O.
4. With respect to the positive pressure mode, earlier PPDVs were originally designed to meet the Emergency Cardiac Care Committee (ECC) cardiopulmonary resuscitation (CPR) guidelines before 1986, which called for “four quick initial breaths and then two quick breaths after every 15 compressions.” This faster rate of ventilation was equivalent to 160 L/min.
5. In 1986, CPR standards were changed to “two slow breaths, each one and one-half seconds in duration.” The standard changed again in 1992 to the current one of “two slow, full breaths, with duration of  to 2 seconds each” (equivalent to 40 L/min). This was changed to reduce the possibility of gastric insufflation, regurgitation, and aspiration of gastric contents. To meet this guideline of a
to 2 seconds each” (equivalent to 40 L/min). This was changed to reduce the possibility of gastric insufflation, regurgitation, and aspiration of gastric contents. To meet this guideline of a  – to 2-second breath, the manufacturers of PPDVs added a restricting orifice that limited the flow rate to 40 L/min. Unfortunately, this created increased breathing resistance to the demand feature.
– to 2-second breath, the manufacturers of PPDVs added a restricting orifice that limited the flow rate to 40 L/min. Unfortunately, this created increased breathing resistance to the demand feature.
6. In 1993, a new-style PPDV, called the FROPV (MTV-100), was introduced. Its specifications include a flow rate of 40 L/min while being used in positive pressure mode and 115 L/min in demand mode, eliminating the difficulties of the earlier models.
7. The mask adapter is a standard 15-mm (0.6-inch) fitting that fits a variety of masks and can also be used directly with an endotracheal tube. The disadvantages of the FROPV are that a supply of O2 is required for its use and that in intubated patients the health care provider will not be able to “feel” decreased lung compliance.
Bag-Valve-Mask
1. The bag-valve-mask (BVM) consists of a mask, bag, and valves that control or direct the flow of air and O2. Like the FROPV, the mask can be changed to different styles to accommodate different faces or can be used directly with an endotracheal tube. The volume of the bag is 1000 to 1200 mL, depending on the manufacturer. Some have an outlet and reservoir for use with supplemental O2.
2. An advantage to the BVM is that although it works best with supplemental O2, it will function on room air if the O2 supply is depleted. In addition, in intubated persons, some health care providers are able to “feel” decreased lung compliance.
3. The primary disadvantage is that it requires training and practice to effectively use a BVM, and even with much practice, many find it is difficult to maintain adequate mask seal and ventilate sufficient volumes when only one rescuer is available to use it. Even with proper training, few individuals can maintain adequate mask seal and a patent airway with one hand while squeezing the bag fully to achieve the 700- to 1000-mL standard volume. The DOT recommends that the BVM be used first with two rescuers (one maintaining mask seal and patency of the airway, the other squeezing the bag; Fig. 11-1). A BVM with one rescuer should be the last choice (after all other devices and techniques) in ventilating a patient. In addition, there is no overpressurization relief valve. This is rarely a concern in nonintubated persons because of the aforementioned difficulties in achieving even minimally acceptable ventilatory volumes, but it is of concern in intubated patients.
Resuscitation Mask
1. The pocket-type resuscitation mask consists of a clear, flexible plastic mask designed to fit over the mouth and nose of the patient while the health care provider ventilates by exhaling through the “chimney.” A one-way valve usually directs the rescuer’s breath into the patient while at the same time directing the exhaled breath of the patient away from the rescuer. It is a relatively simple device that requires minimal training, is lightweight, and is more likely to be available when equipment is at a minimum. It is available both with and without an outlet for supplemental O2.
2. The pocket-type mask is most effective when used with supplemental O2. It will also function on room air and does not have an overpressurization relief valve.
Constant Flow Devices for Adequately Breathing Patients
1. The nonrebreather mask is the first choice when considering constant-flow supplemental O2 in an acute medical emergency. It consists of a mask, reservoir bag, and two or three one-way valves, one separating the reservoir from the mask and the other one or two on the sides of the mask. Oxygen flows into the reservoir bag so that when the patient inhales, he or she inhales O2 from the reservoir. The one-way valves on the sides of the mask keep air from coming into the mask and diluting the O2. When the patient exhales, expired air goes out of the mask through the one or two valves on the face and is prevented from entering the reservoir.
2. The efficiency of this mask depends on the mask fit and seal and proper functioning of the valves. Under ideal conditions, this mask (when fitted with all three valves) may deliver an FIO2 of up to 0.95. Field studies show it may deliver an FIO2 as low as 0.60, but it is still the most effective constant-flow device available (except for O2 rebreathers).
3. To use the mask, it is attached to the O2 supply at a flow rate of 10 to 15 L/min. The reservoir bag must be inflated or “primed” before placing it on the person. This can be accomplished by placing a thumb or fingers on the valve between the reservoir and mask while the reservoir inflates. Care must be taken to not allow the O2 supply to be depleted while the mask is on the person. Because of the one-way valves, if there is no O2 supply, suffocation may result. The mask is available with either two one-way valves on the sides or with only one (labeled as “with safety outlet”). If the mask has only one valve on the side of the mask, it will deliver reduced FIO2.
4. The advantage of the nonrebreather mask is that it provides the highest FIO2 of the constant-flow devices. However, it also wastes O2 and may not deliver a high FIO2 under less than ideal conditions. Care must be taken to monitor the patient and O2 supply closely to avoid allowing the tank to empty while the mask is still on the patient’s face. If there is a risk for depleting the oxygen supply during patient evacuation or transportation, remove one of the one-way valves to prevent suffocation.
Nasal Cannula
1. The only other recommended constant-flow device for prehospital emergency O2 administration is the nasal cannula. This is recommended when the patient requires lower FIO2 or when the patient will not tolerate any kind of mask such as a person with a long history of COPD. It must be understood that a nasal cannula is capable of delivering FIO2 of only 0.24 to 0.29.
2. Flow rates for a nasal cannula are limited to 1 to 6 L/min for prolonged use. To use the nasal cannula, place the prongs in the patient’s nares and loop the tubing over the top of the ears to hold it in place. Adjust the tightness at the neck to a comfortable level. Flow rates exceeding 4 L/min are extremely uncomfortable and may result in drying of the nasal mucosa.
Oxygen Rebreathers
1. One of the problems with long transports commonly seen in the case of wilderness or remote emergency medical care is that all of the previously discussed O2 delivery devices waste O2 and require multiple portable or large nonportable cylinders if the transport time exceeds 1 hour. Breathing room air, a person inhales 21% O2 and exhales 16% O2. If a person inhales (under ideal conditions) 100% O2, the exhaled gas will contain 95% O2 and 5% CO2. The theory of the design of a rebreather is to remove CO2 from the exhaled gas, supplement for the 5% O2 that was metabolized, and reuse the exhaled O2.
2. Several manufacturers produce rebreathers for emergency medical O2 administration, all of which have the same basic components: a mask; breathing circuit (similar to anesthesia equipment); and canister with an absorbent chemical, usually soda lime or Sodasorb.
3. The soda lime chemically removes CO2 from the exhaled gas, allowing for the O2 to be rebreathed. Supplemental O2 is added at flow rates of less than 2 L/min to replace the metabolized O2. Thus a cylinder that can last 45 minutes with a nonrebreather mask or a little more than 1 hour on demand now can last for more than 6 hours, and the patient (with proper technique) will still receive FIO2 of 0.85 to 0.99. In a situation in which equipment is limited because of size and weight, this device may prove invaluable.
4. Different manufacturers recommend beginning the patient on O2 during assembly or while setting up the unit, then flushing the system of air and applying it to the patient. Others recommend air breaks to minimize the risk for pulmonary oxygen toxicity.
5. Thermal considerations are important because of the chemical reaction that takes place with the soda lime. The reaction produces heat and water, so it provides warmed and humidified O2. In cold climates this is an advantage, but in hot climates it may be a disadvantage. If one is in a hot climate, it is recommended to pass the breathing circuit hoses through cold or ice water to cool the gas. Rebreather setups are typically lightweight and allow high FIO2 (≈0.80) at constant flow rates of less than 2 L/min, thereby extending the life of the cylinder.
6. Disadvantages are the training requirement and that the breathing circuit and absorbent canister containing the soda lime are typically “single-patient use.” Like other O2 delivery devices, the rebreather also depends on an adequate mask seal to function effectively. Poor mask seal results in dilution of inhaled gas with air and lower FIO2. An increase in breathing resistance may also occur when compared with a constant-flow mask.
7. The most common types of resuscitators available on the market today are the American DAN REMO2 system, two German systems (the Wenoll and the Circulox), and an Australian system (OXI-Saver Resuscitator).
Nonbreathing Patients
1. Concerns for ventilating nonbreathing patients include rate (breaths per minute), volume, flow rate or speed, pressure, and oxygenation. The rate of ventilations per minute is 12 breaths/min for an adult (older than 8 years old) and 20 breaths/min for children and infants.
2. The recommended volume for ventilations for an adult is 700 to 1000 mL. If a ventilation device or technique does not have an overpressure relief valve and greater volumes are administered, pulmonary barotrauma (pulmonary overpressurization injury) may result. Ventilatory volumes less than 700 mL may not be sufficient to inflate the alveoli, and thus gas exchange will be inadequate. Each ventilation should be at least  to 2 seconds in duration (equivalent to 40 L/min). Faster ventilation rates or speeds force open the esophagus and push air into the stomach rather than the lungs. Increased gastric insufflation greatly increases the risk for regurgitation and aspiration of gastric contents.
to 2 seconds in duration (equivalent to 40 L/min). Faster ventilation rates or speeds force open the esophagus and push air into the stomach rather than the lungs. Increased gastric insufflation greatly increases the risk for regurgitation and aspiration of gastric contents.
3. A differential pressure of as little as 90 to 110 cm H2O is sufficient to rupture alveoli and allow gas to escape into interstitial spaces. Care must be taken to not exceed these pressures when ventilating a person. Humans can easily generate pressures exceeding 120 cm H2O by exhaling forcefully, and thus according to ECC CPR guidelines, one should “blow until the chest rises” to accommodate various sizes of individuals. The only device for ventilating adults that has an overpressure relief valve is the PPDV/FROPV.
4. The primary goal of ventilation is oxygenation. With mouth-to-mouth or mouth-to-mask breathing without supplemental O2, FIO2 will be the same as exhaled gas, which is 0.16, or 16% O2. Adding O2 at a flow rate of 15 L/min with a pocket mask may increase the FIO2 to up to 50%. A BVM on room air is 0.21, and with O2 at 15 L/min up to 0.9, depending on the equipment and the skill of the operator. An FROPV delivers close to 1, or 100% O2.
5. Both the volume and oxygenation achieved by ventilations depend on the quality of the mask seal and patency of the airway. The single most common cause of inadequate ventilation in a nonintubated person is poor mask seal. Great care must be taken to ensure that the airway is fully patent and that there is a good mask seal with each ventilation. If the patient is not intubated, an oropharyngeal, nasopharyngeal, or combination airway should be used if available.
6. Because an FROPV delivers the highest FIO2, is the only device that is limited to 40 L/min flow rate ( to 2 seconds in duration), and has an overpressure relief valve, it may be the best choice for ventilating a person in respiratory arrest, whether or not he is intubated. A BVM unit used by two rescuers (one to maintain the mask seal and the other to squeeze the bag) is the best alternative.
to 2 seconds in duration), and has an overpressure relief valve, it may be the best choice for ventilating a person in respiratory arrest, whether or not he is intubated. A BVM unit used by two rescuers (one to maintain the mask seal and the other to squeeze the bag) is the best alternative.
7. The following is the order of preference for ventilating a person in respiratory arrest: