EMERGENCY CHILDBIRTH
When a woman is ready to give birth, the contractions of labor are usually intense and uninterrupted, or separated by intervals of less than 3 to 5 minutes. If the child to be born is not the woman’s first, labor can progress very quickly, so don’t wait until the last minute to set up. On the other hand, don’t deliver a baby in the woods if it isn’t necessary. If the child is the mother’s first, if the contractions are more than 5 minutes apart, if the waters have not “broken” (a gush of fluid from the ruptured amniotic sac) and there has been no passage of bloody mucus, and if no bulging is present in the vaginal area, consider whether you have time to make it to the hospital. If the waters have broken and labor has not begun, it is best to evacuate the mother, because delivery must occur or be induced within 24 hours to avoid the onset of an infection that could jeopardize the infant and mother. If the umbilical cord or any other part of the infant other than the head is showing at the vagina, the delivery will be difficult and should be performed if at all possible by a skilled obstetrician.
A baby is delivered in (ideally) two stages. First, the head and face appear, usually with the face down (Figure 104). Once the infant has appeared to the level of his eyebrows, instruct the mother to stop pushing. The baby will be extremely slippery. When his face appears, run your fingers around the infant’s neck to see if the umbilical cord is wrapped around it. If it is, see if you can slip it over the head. If not, tie (clamp) it off tightly twice, with about 1 ½ in (3.8 cm) between ties, and cut carefully between the ties. The ties must be tight and not slip off, or the baby could suffer severe bleeding.
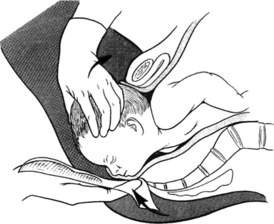
The baby’s head and body will spontaneously rotate 90 degrees (don’t twist them) to one side as the body starts to emerge. Have the mother resume pushing. While supporting the head, grasp the uppermost (with respect to the ground) shoulder and apply gentle downward pressure until the upper shoulder is delivered from the vagina (Figure 105). Don’t tug on the head or pull from underneath the infant’s armpits. After the upper shoulder is out, exert gentle upward pressure to free the lower shoulder (Figure 106). At this point, be prepared to hang on tight, because the rest of the baby will shoot out, usually with a big gush of amniotic fluid and some blood.
The long end of the umbilical cord, which is still attached to the placenta that is attached to the inside wall of the uterus, will be hanging from the mother’s vagina. The placenta will deliver spontaneously, so do not pull on the umbilical cord. Do not massage the mother’s abdomen (uterus) until after the placenta is delivered. Place the placenta in a plastic bag and bring it to civilization for inspection. After the placenta is delivered, gently massage the mother’s abdomen for 30 minutes. This stimulates the uterus to contract and helps control bleeding. It will feel like a firm, rounded, grapefruit-sized mass in the middle of the lower abdomen just above the pubic bone. If bleeding starts again, massage more vigorously. You may have to repeat this a few times during the hours immediately following childbirth. It may be uncomfortable for the mother.
If bleeding seems profuse after the placenta is delivered, or if the placenta does not spontaneously deliver after 60 minutes, be prepared to treat for shock (see page 60).
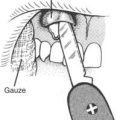
If the vagina is torn, apply pressure with a sterile compress. After the bleeding slows, the vaginal area can be gently washed, with the mother on her back, so that rinse water flows away from the vagina toward the anus. Take care to keep any contaminating material or solutions out of the vagina. Lay a sterile compress or clean sanitary napkin over the vagina.