Embryology, Anatomy, Normal Findings, and Imaging Techniques
Embryology
External Ear
The pinna (auricle) develops from six mesenchymal proliferations, called hillocks, which are located at the dorsal ends of the first and second pharyngeal arches. They surround the first pharyngeal cleft (the future external auditory meatus). These hillocks gradually fuse and form the definitive auricle.1
Middle Ear
The tympanic cavity is derived from endoderm and develops from the first pharyngeal pouch. This pouch grows laterally until it comes in contact with the floor of the first pharyngeal cleft. The lateral part of the pouch gives rise to the primitive tympanic cavity. The medial part of the pouch is smaller and forms the eustachian tube. The malleus and incus are derived from the cartilage of the first pharyngeal arch, whereas the stapes is derived from the second pharyngeal arch. The ossicles remain embedded in the mesenchyme until the eighth month, when the surrounding tissue dissolves. The tympanic cavity expands dorsally to form the mastoid antrum late during fetal life. Pneumatization of the mastoid process continues after birth.1
Inner Ear
Between the sixth and eighth weeks of gestation, the cochlear duct, arising from the saccule, penetrates the surrounding mesenchyme and completes the two and a half turns. The thin residual connection between the cochlea and saccule is the ductus reuniens. At the tenth week, the cartilage that differentiated from the mesenchyme surrounding the cochlear duct undergoes vacuolization and two perilymphatic spaces are formed: the scala tympani and the scala vestibuli. The cochlear duct (scala media) is separated from the scala vestibuli by the vestibular membrane and from the scala tympani by the basilar membrane. The lateral wall of the cochlear duct remains attached to the surrounding cartilage by the spiral ligament. Medially, the cochlear duct is attached to the modiolus, which is the axis of the bony cochlea. At 6 weeks gestation, semicircular canals appear as outpouchings of the utricular (posterior) component of the otic vesicle.1
Anatomy and Normal Findings
The temporal bone consists of tympanic, squamous, petrous, and mastoid parts and a styloid process.2 The temporal bone may be divided into compartments when studying its anatomy or reviewing imaging studies. These compartments are described from lateral to medial.
Pinna and External Auditory Canal
Detecting subtle abnormalities of the pinna with imaging may be difficult, but in general it is possible to identify gross malformations or absence of pinna on CT. Ossicular abnormalities are present in 98% of the temporal bones with microtia and external auditory canal (EAC) abnormality.3
In cross section, the EAC is oval in shape. Its walls (anterior and posterior; superior and inferior) run parallel to each other throughout the course of the EAC. The EAC consists of two segments: a membranous (fibrocartilaginous) segment that makes up the lateral third of the EAC, and a medial bony segment that forms the remainder of it.4
The tympanic membrane separates the EAC from the middle ear cavity and is attached to the tympanic annulus, which is a circumferential bony prominence at the medial-most aspect of the bony EAC. Superiorly, the tympanic membrane attaches to the scutum (e-Fig. 9-1), which is an important bony landmark in the diagnosis and evaluation of cholesteatoma. If the tympanic membrane is not thickened, wide window settings on CT are required to visualize it.
Middle Ear Cavity (Cleft)
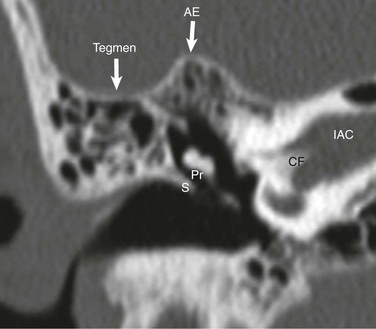
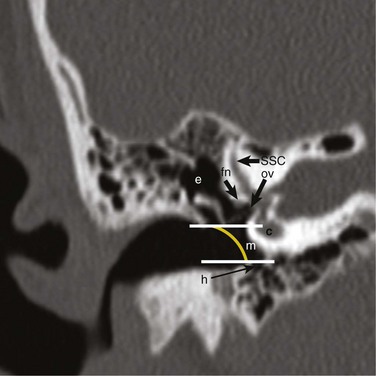
The tympanic cavity is an aerated space medial to the tympanic membrane. Air reaches the middle ear cavity from the nasopharynx via the eustachian tube. The middle ear cavity is arbitrarily divided into three compartments: epitympanum (attic), mesotympanum, and hypotympanum. With lines drawn parallel to the superior and inferior walls of the bony segment of the EAC on the coronal plane, the part of the middle ear cavity above the upper line is the epitympanum (attic), which is the largest portion and houses the bulk of the ossicular chain. The mesotympanum lies between the two lines. The hypotympanum is below the lower line and normally is nonexistent or very small in children (Fig. 9-2).
Ossicles
The malleus, incus, and stapes form the ossicular chain, which is responsible for amplification (~30%) and transmission of sound waves from the tympanic membrane to the oval window on the vestibule.5
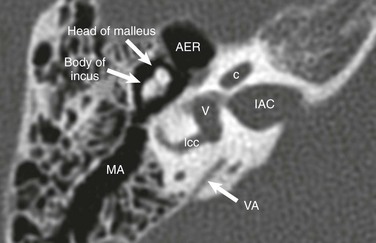
The manubrium (handle) and the lateral process of the malleus are embedded in the tympanic membrane. The tympanic membrane has two parts, divided by the lateral process of the malleus: a smaller pars flaccida superiorly, and a larger pars tensa inferiorly.6 Cranial to the manubrium is the neck of the malleus, to which the tendon of the tensor tympani muscle attaches. The tensor tympani muscle is derived from the first branchial arch and is innervated by the only branch of the trigeminal nerve that has motor fibers: V3 (mandibular branch). The head of the malleus forms the “ice cream” of the familiar “ice cream and cone” appearance and articulates with the body of the incus (Fig. 9-3). The malleoincudal joint is a diarthrodial (synovial) articulation, as is the incudostapedial joint (Figs. 9-3 and 9-4).
The incus is the largest of the three middle ear ossicles. Its body articulates with the head of the malleus and forms the “cone.” The short process of the incus (which is better appreciated on the axial images) extends from the body dorsally and resides in the fossa incudis, to which it is secured by ligaments that are invisible on CT. The long process of the incus extends inferiorly from the body. The lenticular process of the incus joins the long process, forming a nearly 90° angle. The long and lenticular processes of the incus are very delicate and are more prone to erosion as a result of infection and/or inflammation than are other parts of the ossicular chain. The lenticular process is cup shaped medially and articulates with the head (capitulum) of the stapes. The head of the stapes is connected to the crura (anterior and posterior), which subsequently join the footplate of the stapes. The opening between the crura of the stapes is the obturator foramen, where the stapedial artery is located in fetal life. The stapes footplate articulates with the oval window, forming the syndesmotic (fibrous) stapediovestibular joint.5
Recesses and Ridges of the Middle Ear Cavity
The anterior epitympanic recess (Figs. 9-3 and 9-4) is contiguous with the middle ear cavity through an incomplete septum, named “cog,” the integrity of which may be lost because of infection or inflammation.5
Mastoid Air Cells
The interconnected, air-filled mastoid air cells open into the mastoid antrum, which in turn communicates with the middle ear cavity (Figs. 9-3 and 9-4). The connection between the middle ear cavity and mastoid antrum is the aditus ad antrum (opening to antrum). The mastoid air cells are separated by innumerable thin septa. The Körner septum is the bony thickening that runs obliquely through the mastoid air cells; it is an important surgical landmark. The roof of the middle ear cavity is the tegmen tympani (e-Fig. 9-1).
Facial and Vestibulocochlear Nerves and Internal Auditory Canal
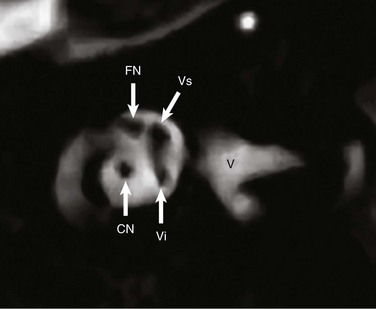
The facial nerve has motor, parasympathetic, and special sensory (taste) fibers. Its nucleus lies in the dorsal pons. It is important to remember that the facial nerve has a rather long intraaxial segment extending from the nucleus through the nerve exit zone at the surface of the lateral pons. The cisternal and canalicular segments of the facial nerve are evaluated on high-resolution T2-weighted images of the temporal bone. The cisternal segment, the longest segment of the facial nerve, can be identified routinely on high-resolution MRI. The facial nerve enters the internal auditory canal (IAC) through the porus acusticus and is named the canalicular segment thereafter. In the IAC, the facial nerve lies in the anterior-superior quadrant. The lateral-most aspect of the IAC is the fundus, which is divided by the crista falciformis (e-Fig. 9-1) into superior and inferior compartments. The superior compartment is further divided into anterior and posterior parts by vertical, variably ossified arachnoid tissue, known as the Bill bar. The cochlear nerve occupies the anterior-inferior quadrant, and the vestibular nerve (superior and inferior branches) is seen in the posterior quadrants7 (e-Figs. 9-5 and 9-6).
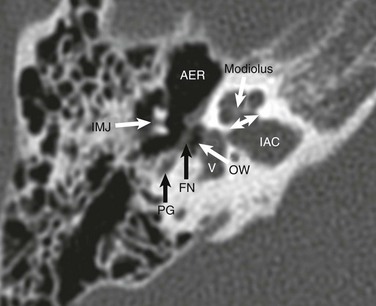
The facial nerve enters the labyrinthine canal and fills approximately 95% of this canal. The labyrinthine segment of the facial nerve is particularly susceptible to ischemia because its bony confines do not permit swelling during inflammation. The labyrinthine segment synapses at the geniculate ganglion, from which the parasympathetic greater superficial petrosal nerve arises. The greater superficial petrosal nerve recruits some sympathetic fibers and become the vidian nerve, providing the parasympathetic innervation of the lacrimal gland. Distal to the geniculate ganglion, the facial nerve makes a dorsal turn and becomes the tympanic segment. The distal labyrinthine segment, geniculate ganglion, and proximal tympanic segment make up the anterior genu. The tympanic segment of the facial nerve lies at the medial wall of the tympanic cavity and below the lateral semicircular canal. The tympanic segment has a thin, inconsistent bony covering. The tympanic segment lies in close proximity but lateral to the oval window. The posterior genu is a nearly 90° bend where the tympanic segment meets the mastoid (or descending) segment (Fig. 9-4). The mastoid segment exits the temporal bone through the stylomastoid foramen. Just proximal to the stylomastoid foramen, the chorda tympani arises from the mastoid segment, extends into the middle ear cavity in its own canal, and traverses the middle ear cavity within the tympanic membrane, between the manubrium of the malleus and incus. The chorda tympani contains the taste sensation fibers from the anterior two thirds of the tongue, as well as the parasympathetic fibers to the submandibular and sublingual glands.2 After exiting the temporal bone, the facial nerve traverses the parotid gland (but does not innervate it) and innervates the facial musculature. The parotid gland is divided by the facial nerve into deep and superficial lobes.
Oval Window/Round Window
The stapes footplate rests on the oval window (Fig. 9-4). It can be appreciated easily on both axial and coronal CT images. The abnormalities of the oval window include atresia and stenosis, which usually are associated with abnormalities of the ossicles and external ear. The round window is easier to appreciate on coronal images because of the fluid-air interface at the inferior aspect of the vestibule.
Vestibular Aqueduct/Cochlear Aqueduct
The vestibular aqueduct (seen on CT) is the bony housing of the endolymphatic duct and sac. It is seen on MRI when enlarged (Fig. 9-3). The vestibular aqueduct is considered enlarged when it measures greater than 1.0 mm at its midpoint.8 Although its enlargement is commonly associated with sensorineural hearing loss, this observation does not alter the management if the patient is otherwise a good candidate for cochlear implantation.
Inner Ear
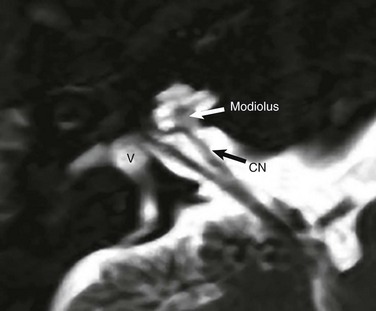
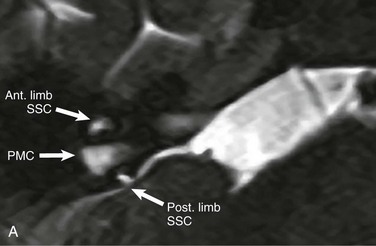
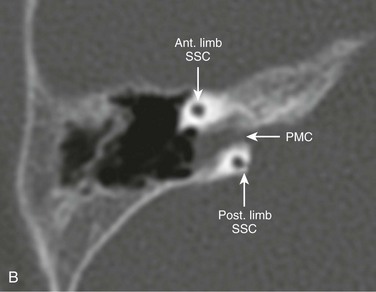
MRI is the modality of choice in the assessment of the inner ear; however, many inner ear abnormalities also may be appreciated by examining the bony labyrinth with CT. The cochlea lies anterior to the IAC and is made up of basal, middle, and apical turns. The basal and middle turns are complete 360-degree turns, whereas the apical turn covers 180 degrees, hence the normal two and a half turns. The modiolus is the bony axis of the cochlea; it has a “star” or “crown” shape and can be seen atop the cochlear aperture (Fig. 9-4 and e-Fig. 9-5). The vestibule has a delicate, nearly cylindrical shape (Fig. 9-3 and e-Fig. 9-5). The semicircular canals (superior, posterior, and lateral) are at right angles to each other and connect to the vestibule. Although six openings in the inner surface of the vestibule (two for each semicircular canal) are expected, five openings exist because the posterior limb of the superior semicircular canal and the superior limb of the posterior semicircular canal unite to form the common crus, which has its own opening to the vestibule. The lateral semicircular canal is slightly larger than the other two semicircular canals.
Petromastoid (Subarcuate) Canal
The petromastoid canal is almost always visualized on CT. It lies underneath the arch of the superior semicircular canal and is closer to its posterior limb. Its size decreases with age. When fluid is present in the petromastoid canal (due to cerebrospinal fluid in the dural sleeve about the subarcuate artery that travels in the canal to reach the mastoid air cells and middle ear cavity), the petromastoid canal occasionally can be identified on MRI examinations of young children (e-Fig. 9-7). It is a normal structure and should not be confused with a pathologic lesion.
Imaging Techniques
CT is reserved for conductive hearing loss, whereas MRI is used in the evaluation of sensorineural hearing loss.9 A low-dose technique is used in volumetric CT acquisition; the imaging parameters include a kVp of 90 and an mA of 80, resulting in a dose length product of approximately 90 mGy/cm. Attention is required to keep the lenses outside the field of the primary beam. Coronal and, if necessary, oblique-sagittal reformations are generated.
Fatterpekar, GM, Doshi, AH, Dugar, M, et al. Role of 3D CT in the evaluation of the temporal bone. Radiographics. 2006;26(suppl 1):S117–S132.
Lane, JI, Lindell, EP, Witte, RJ, et al. Middle and inner ear: improved depiction with multiplanar reconstruction of volumetric CT data. Radiographics. 2006;26(1):115–124.
Niu, Y, Wang, Z, Liu, Y, et al. Radiation dose to the lens using different temporal bone CT scanning protocols. AJNR Am J Neuroradiol. 2010;31(2):226–229.
Shah, LM, Wiggins, RH, 3rd. Imaging of hearing loss. Neuroimaging Clin N Am. 2009;19:287–306.
References
1. Sadler, TW. Ear. In: Sadler TW, ed. Langman’s medical embryology. Baltimore: Williams & Wilkins, 1990.
2. Warwick, R, Williams, PL, The temporal bones. Br. Warwick R, Williams PL, eds. Gray’s anatomy, 35th ed, Philadelphia: Longman Group Ltd, 1973.
3. Mayer, TE, Brueckmann, H, Siegert, R, et al. High-resolution CT of the temporal bone in dysplasia of the auricle and external auditory canal. AJNR Am J Neuroradiol. 1997;18(1):53–65.
4. Castillo, M, Valerie, LJ, Buchman, C. The external auditory canal and pinna. In Swartz JD, Loevner LA, eds.: Imaging of the temporal bone, 4th ed, New York: Thieme, 2009.
5. Swartz, JD. The middle ear and mastoid. In Swartz JD, Loevner LA, eds.: Imaging of the temporal bone, 4th ed, New York: Thieme, 2009.
6. Warwick, R, Williams, PL. The auditory and vestibular apparatus. In: Warwick R, Williams PL, eds. Gray’s anatomy. Philadelphia: Longman Group Ltd, 1973.
7. Raghavan, P, Mukherjee, S, Phillips, CD. Imaging of the facial nerve. Neuroimaging Clin North Am. 2009;19(3):407–425.
8. Vijayasekaran, S, Halsted, MJ, Boston, M, et al. When is the vestibular aqueduct enlarged? A statistical analysis of the normative distribution of vestibular aqueduct size. AJNR Am J Neuroradiol. 2007;28(6):1133–1138.
9. Shah, LM, Wiggins, RH, 3rd. Imaging of hearing loss. Neuroimaging Clin North Am. 2009;19(3):287–306.