2 Elbow Injuries
Pediatric Elbow Injuries in the Throwing Athlete: Emphasis on Prevention
Robert C. Manske, PT, DPT, SCS, MEd, ATC, CSCS, and Mark Stovak, MD
Introduction
Approximately 30 million children and teenagers participate in organized sports in the United States (Adirim and Cheng 2003). Despite the fact that sports are the leading cause of injury in adolescent athletes, it is estimated that more than half of those injuries are preventable (Emery 2003). Pain in the elbow is a common occurrence in young baseball players, especially pitchers. Table 2-1 lists possible differential diagnoses in adolescents with elbow pain. One study found that elbow pain in youth baseball pitchers was associated with multiple factors including age, weight, height, number of pitches thrown during the season, satisfaction with performance, fatigue, lifting weights, and playing outside of the league (Lyman et al. 2001). Studies have found that, during a season, 26% to 35% of youth baseball players have either shoulder or elbow pain, with self-reported shoulder pain in more than 30% of pitchers and elbow pain in more than 25% immediately following a game (Lyman et al. 2001, Lyman et al. 2002). The simple act of throwing is violent because of the stresses it places on the elbow. Because ligaments and muscles are attached to the bone at the medial elbow at a time when the secondary ossification centers are not fused, a traction apophysitis can occur when this growth plate is not able to withstand the forces placed on it. Conversely, compression on the lateral side of the elbow commonly is a cause for Panner’s disease or osteonecrosis of the capitellum.
| Locale | Possible Diagnosis | Age (years) |
|---|---|---|
| Lateral | Avascular necrosis of capitellum (Panner’s) | 7–12 |
| Osteochondritis dissecans | 12–16 | |
| Medial | Medial apophysitis (Little Leaguer’s elbow) | 9–12 |
| Medial collateral ligament strain/sprain | All | |
| Flexor/pronator strain | All | |
| Medial epicondyle avulsion | <18 | |
| Ulnar neuritis | All | |
| Posterior | Olecranon apophysitis | |
| Olecranon (posterior) impingement | ||
| Olecranon osteochondrosis | ||
| Triceps/olecranon tip avulsions | ||
| Other | Fracture | All |
| Loose bodies | >18 | |
| Synovitis | All |
Little Leaguer’s elbow
Little Leaguer’s elbow is considered a host of elbow pathology in a young throwing athlete. The various types of injuries that can be considered Little Leaguer’s elbow are listed in Table 2-2.
| Medial epicondyle fragmentation |
| Medial epicondyle avulsion |
| Delayed apophyseal growth of medial epicondyle |
| Accelerated apophyseal growth of medial epicondyle |
| Delayed closure of the medial epicondylar apophysis |
| Delayed closure of the olecranon apophysis |
| Osteochondrosis of the capitellum |
| Osteochondritis of the capitellum |
| Osteochondrosis of the radial head |
| Osteochondritis of the radial head |
| Hypertrophy of the ulna |
| Olecranon apophysitis |
Medial tension injuries
Medial tension injuries most commonly include medial epicondylar apophysitis. With repetitive stress to the medial elbow in the throwing adolescent, the flexor pronator mass and the ulnar collateral ligament apply tensile forces that cause medial epicondyle apophysitis (Pappas 1982, Rudzki and Paletta 2004). This apophysitis is thought to occur rather than rupture of the ulnar collateral ligament (Joyce et al. 1995). Chronic attritional tears of the ulnar collateral ligament are fairly rare in adolescent athletes (Ireland and Andrews 1988). Despite this rarity, it appears that ulnar collateral injuries are increasing in high school athletes. Petty et al. (2004) reported that the percentage of high school athletes who required ulnar collateral ligament reconstruction in their center jumped from 8% between 1988 and 1994 to 13% between 1995 and mid-2003. Injuries to the ulnar collateral ligament in adolescent athletes generally occur as acute events, rather than through attrition as in older, more skeletally mature athletes.
Lateral compression injuries
Several conditions caused by compression of the lateral side of the elbow can occur in younger pitchers. Two of the more common are osteochondritis dissecans (OCD) and Panner’s disease. Although traditionally these have been thought to be the same condition by some, they are separate entities. Osteochondritis is a localized condition involving articular cartilage that has separated from the underlying subchondral bone and is caused by repetitive trauma (Yadao et al. 2004). Panner’s disease is a focal osteonecrosis of the entire capitellum seen primarily in boys aged 7 to 12 years old and is not associated with trauma (Yadao et al. 2004).
Posterior compression injuries
Whereas medial and lateral elbow pain occurs as a result of “valgus extension overload” during the late cocking–early acceleration phase of throwing, posterior pain occurs during the terminal phase of throwing as the elbow is locked into full extension. The synovium can be pinched in the olecranon when the elbow is in full extension, resulting in posterior impingement syndrome, or the posterior apophysis can be stressed by triceps traction, causing olecranon apophysitis (Crowther 2009).
Prevention
Several associations have provided recommendations regarding adolescent athletes and prevention of both elbow and shoulder problems. The American Academy of Pediatrics and USA Baseball each have guidelines regarding pitch counts. The American Academy of Pediatrics recommends limits of 200 pitches per week or 90 per outing, while the USA Baseball Medical and Safety Advisory Committee recommends a more stringent 75 to 125 pitches per week or 50 to 75 pitches per outing depending on age (Committee on Sports Medicine and Fitness, USA Baseball Medical and Safety Advisory Committee 2001).
USA baseball guidelines
Pitch Counts
Pitch counts should be carefully monitored and regulated in adolescents. Recommended limits vary depending on age of the pitcher (Table 2-3).
| Age (yrs) | 2006 USA Baseball Guidelines | 2010 Little League Baseball Regulations |
|---|---|---|
| Daily limits | ||
| 17–18 | n/a | 105/day |
| 15–16 | n/a | 95/day |
| 13–14 | 75/game | |
| 11–12 | 75/game | 85/day |
| 9–10 | 50/game | 75/day |
| 7–8 | n/a | 50/day |
| Weekly limits | ||
| 13–14 | 125/wk; 1000/season; 3000/yr | |
| 11–12 | 100/wk; 1000/season; 3000/yr | |
| 9–10 | 75/wk; 1000/season; 2000/yr | |
| 7–18 | ||
Additionally, pitchers 16 years of age or younger must adhere to the following rest requirements:
Pitchers 17 to 18 years of age should adhere to the following rest requirements:
Pitch Types
Because the risk of injury from throwing breaking pitches is increased in the adolescent athlete, curveballs and sliders are not recommended (Lyman et al 2002). These pitches become even more problematic when the athlete does not exhibit adequate throwing mechanics. Recommended ages to learn types of pitches are listed in Table 2-4.
| Pitch | Age |
|---|---|
| Fastball | 8–10 |
| Change-up | 10 |
| Curveball | 14 |
| Knuckleball | 14 |
| Slider | 16–18 |
| Forkball | 16–18 |
| Splitter | 16–18 |
| Screwball | 17–18 |
USA Baseball Medical and Safety Advisory Committee.
Medial Collateral Ligament and Ulnar Nerve Injury at the Elbow
Michael Levinson, PT, CSCS, and David W. Altchek, MD
Anatomy and biomechanics
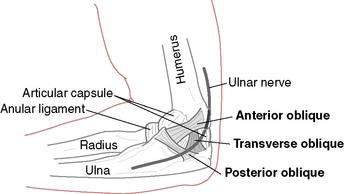
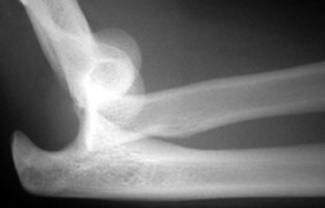
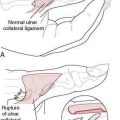
The MCL is composed of two primary bundles. The anterior bundle runs from the sublime tubercle of the ulna and inserts on the inferior surface of the medial epicondyle. The anterior bundle tightens in extension and loosens in flexion. The posterior band runs from the posterior portion of the medial epicondyle and inserts at the ulna proximal and posterior to the sublime tubercle (Fig. 2-1). The posterior bundle tightens in flexion and loosens in extension. The anterior bundle is the prime focus of the MCL reconstruction. The ulnar nerve runs in the space posterior to the medial epicondyle. The space is referred to as the cubital tunnel. The roof of the tunnel is referred to as the cubital tunnel retinaculum. At this location, the nerve is significantly exposed.
Mechanism of injury
Injury to the MCL is a result of the repetitive, extreme valgus loads to the elbow while throwing. The MCL is the primary restraint to valgus stress at the elbow. Dillman et al. (1995) demonstrated that a fastball thrown by an elite baseball pitcher produces a load that approaches the actual tensile strength of the MCL. The MCL attempts to withstand these forces during the late cocking and acceleration phases of throwing. Repetitive overloading can result in inflammation and microtears of the ligament, which can eventually lead to failure. Continuing to throw with instability can lead to degenerative changes in the elbow.
Surgical treatment
Medial Collateral Ligament Reconstruction
Reconstruction of the medial collateral ligament is performed using the “docking technique” described by Altchek et al. (2000). The anterior bundle is the primary focus of the reconstruction. The ipsilateral palmaris longus is the graft of choice. In the absence of this muscle, the gracilus is used. Our rehabilitation guidelines are not affected by graft choice; however, when using the gracilis, the affected lower extremity must be considered.
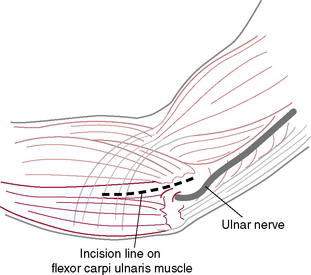
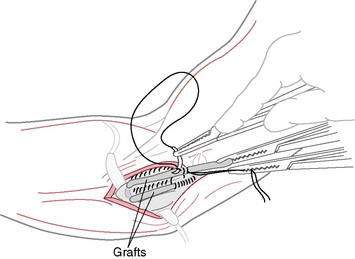
This procedure includes a routine arthroscopic evaluation of the elbow through a muscle-splitting approach that preserves the flexor–pronator origin (Fig. 2-2). Bone tunnels are created in the humerus and ulna. The graft is “docked” securely in the tunnels with sutures (Fig. 2-3). This technique also minimizes the number of tunnels and reduces the size of the drill holes. Finally, this technique avoids an obligatory ulnar nerve transposition.
Rehabilitation Overview and Principles
The rehabilitation program following MCL reconstruction is based on the healing restraints and functional demands of the graft (Rehabilitation Protocol 2-1). Time frames for returning to certain activities are based on allowing the graft to both strengthen adequately and regain adequate flexibility. The program features early, safe range of motion (ROM) to allow optimal tissue healing and minimize the effects of immobilization. Elbow ROM in a hinged brace is initiated after 1 week to prevent contracture, provide pain control, enhance collagen formation, and nourish articular cartilage. Range of motion is increased gradually in the brace over the initial 6-week postoperative period. Aggressive, passive stretching should be avoided throughout rehabilitation. Elbow extension is restored using a low-load, long-duration stretch, which has been demonstrated to be an effective method for restoring range of motion.
REHABILITATION PROTOCOL 2-1 Medial Collateral Ligament Reconstruction Guidelines
Rehabilitation following ulnar nerve transposition follows the same progression as the MCL reconstruction; however, the progression is generally shorter (Rehabilitation Protocol 2-2). The brace is discontinued after 3 weeks, at which time a formal strengthening program is begun. A throwing program normally can be initiated at 10 to 12 weeks.
Conservative Treatment of Medial Collateral Ligament Injuries
As mentioned previously, improved operative techniques and rehabilitation guidelines have made surgical intervention the treatment of choice, especially for throwing athletes. Little scientific data exist to support conservative treatment, especially in competitive throwers, for return to pre-injury activity level. However, at times conservative treatment may be an option (Rehabilitation Protocol 2-3).
Treating Flexion Contracture (Loss of Extension) in Throwing Athletes
Tigran Garabekyan, MD, and Charles E. Giangarra, MD
Recommended criteria for a safe return to sports include
See Rehabilitation Protocol 2-4 for the treatment protocol following elbow arthroscopy.
REHABILITATION PROTOCOL 2-4 After Elbow Arthroscopy
Phase 2: Intermediate Phase
Post-Traumatic Elbow Stiffness
Daniel Woods, MD, and Charles E. Giangarra, MD
Classification
The etiology of elbow stiffness has been classified by various authors. Kay (1998) based his scheme on the anatomic components involved. Type I involves soft tissue contractures; type II involves soft tissue contractures with ossification; type III involves nondisplaced articular fracture with soft tissue contracture; type IV involves displaced intra-articular fractures with soft tissue contracture; and type V involves post-traumatic bony bars blocking elbow motion.
Morrey (1990) classified elbow stiffness into intrinsic, extrinsic, and mixed causes (Table 2-5). Intrinsic causes are related to intra-articular pathology resulting from deformities or malalignment of the articular surface, intra-articular adhesions, loose bodies, impinging osteophytes, and fibrosis within the olecranon or coronoid fossa. Extrinsic causes are related to all entities aside from the articular surface. Examples include skin contracture from scars or burns, capsular and collateral ligament contracture, and heterotopic ossification. Another important extrinsic cause is injury to brachialis or triceps resulting in a hemarthrosis, which may cause scarring, fibrosis, and limitation of motion. Entrapment of the ulnar nerve can lead to pain resulting in loss of motion and eventual capsular contracture. Mixed etiologies are defined as extrinsic contractures resulting from intrinsic pathology.
Table 2-5 Morrey’s Causes of Elbow Stiffness by Location of Pathology
| Extrinsic |
Heterotopic ossification
Heterotopic ossification (HO) is an important cause of post-traumatic stiffness of the elbow. Direct trauma, neural axis injury, surgical intervention, and forceful passive manipulation may cause HO, which is directly related to the severity of the initial injury. Noted radiographically approximately 4 to 6 weeks following the event, HO presents with swelling, hyperemia, and loss of motion of the affected joint. HO in the upper extremity has been classified by Hastings and Graham (1994) into three types: I, without functional limitation, II, subtotal limitation, and III, complete bony ankylosis (Table 2-6). Treatment consists of physical therapy and indomethacin or a diphosphonate to begin shortly after the insult. If HO continues to progress, surgical excision of the heterotopic bone when the hyperemia and swelling begin to diminish is indicated. When the HO matures, prompt surgical treatment is important to avoid soft-tissue contractures that may result from prolonged loss of motion.
Table 2-6 Heterotopic Ossification Classification: Upper Extremity
| Class | Description |
|---|---|
| I | Without functional limitation |
| II | Subtotal limitation |
| IIA | Limitation in flexion/extension |
| IIB | Limitation in pronation/supination |
| IIC | Limitation in both planes of motion |
| III | Complete bony ankylosis |
Nonsurgical treatment
The next line of treatment for the stiff elbow is the use of splinting. Dynamic splinting in which a constant prolonged force is supplied through spring or rubber band tension has been used in patients with deficits in flexion and extension. Although positive outcomes have been reported by Sojbjerg (1996) and others, patient compliance is a problem because of the continuous strain and resultant painful muscle spasm of the antagonistic muscle groups.
Rehabilitation considerations
Anatomy and biomechanics
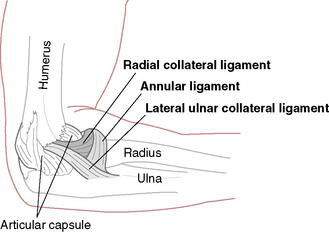
The elbow joint consists of two types of articulations and thus allows two types of motion. The ulnohumeral articulation resembles a hinge joint, allowing flexion and extension, whereas the radiohumeral and proximal radioulnar joint allows axial rotation (Morrey 1986). Stability of the elbow joint is provided by the osseous articulations, medial and lateral collateral ligaments, and traversing muscles.
Mechanism of injury
Evaluation and radiographs
Classification
Treatment
Operative Treatment
Complications
Rehabilitation considerations
REHABILITATION PROTOCOL 2-5 Rehabilitation Protocol After Elbow Dislocation
Phase 1 (Days 1–5)
Phase 2 (Days 6–14)
Results
Lateral and Medial Humeral Epicondylitis
Todd S. Ellenbecker, DPT, MS, SCS, OCS, CSCS, and George J. Davies, DPT, MEd, SCS, ATC, CSCS
Epidemiology and etiology
Reported in the literature as early as 1873 by Runge, humeral epicondylitis or “tennis elbow” as it is more popularly known, has been extensively studied by many authors. Cyriax (1936), listed 26 causes of tennis elbow, whereas an extensive study of this overuse disorder by Goldie (1964) reported hypervascularization of the extensor aponeurosis and an increased quantity of free nerve endings in the subtendinous space. Leadbetter (1992) described humeral epicondylitis as a degenerative condition consisting of a time-dependent process including vascular, chemical, and cellular events that lead to a failure of the cell-matrix healing response in human tendon. This description of tendon injury differs from earlier theories where an inflammatory response was considered as a primary factor; hence, the term “tendinitis” was used as opposed to the term recommended by Leadbetter (1992) and Nirschl (1992).
Nirschl and Ashman (2003) defined humeral epicondylitis as an extra-articular tendinous injury characterized by excessive vascular granulation and an impaired healing response in the tendon, termed “angiofibroblastic hyperplasia.” In a thorough histopathologic analysis, Kraushaar and Nirschl (1999) studied specimens of injured tendon obtained from areas of chronic overuse and reported that they did not contain large numbers of lymphocytes, macrophages, and neutrophils. Instead, tendinosis appears to be a degenerative process characterized by large populations of fibroblasts, disorganized collagen, and vascular hyperplasia. It is not clear why tendinosis is painful, given the lack of inflammatory cells, and it is also unknown why the collagen does not mature.
Nirschl (1992) described the primary structure involved in lateral humeral epicondylitis as the tendon of the extensor carpi radialis brevis. Approximately one third of cases involve the tendon of the extensor communis. Additionally, the extensor carpi radialis longus and extensor carpi ulnaris can be involved. The primary site of medial humeral epicondylitis is the flexor carpi radialis, pronator teres, and flexor carpi ulnaris tendons. Finally, Nirschl (1992) reported that the incidence of lateral humeral epicondylitis is far greater than that of medial humeral epicondylitis in recreational tennis players and in the leading arm (left arm in a right-handed golfer), whereas medial humeral epicondylitis is far more common in elite tennis players and throwing athletes because of the powerful loading of the flexor and pronator muscle tendon units during the valgus extension overload inherent in the acceleration phase of those overhead movement patterns. Additionally, the trailing arm of the golfer (right arm in a right-handed golfer) is reportedly more likely to have medial symptoms than lateral.
Anatomical adaptations in the athletic elbow
Several classic studies have reported on elbow range of motion adaptations.
Several studies have also been cited regarding osseous adaptations in the athletic elbow.
Elbow examination special tests
In addition to accurate measurement of both distal and proximal upper extremity joint range of motion, radiographic screening, and muscular strength assessment, several other tests should be included in the comprehensive examination of the elbow. Although it is beyond the scope of this section to completely review all necessary tests, several are highlighted based on their overall importance. The reader is referred to Morrey (1993), Ellenbecker and Mattalino (1997), and Magee (1997) for more complete information on examination of the elbow.
Clinical testing of the joints proximal and distal to the elbow allows the examiner to rule out referred symptoms and ensure that elbow pain is from a local musculoskeletal origin. Overpressure of the cervical spine in the motions of flexion–extension and lateral flexion–rotation, and the quadrant or Spurling test combining extension with ipsilateral lateral flexion and rotation, are commonly used to clear the cervical spine and rule out radicular symptoms. Tong et al. (2002) tested the Spurling maneuver to determine the diagnostic accuracy of this examination maneuver and found a sensitivity of 30% and specificity of 93%. Caution therefore must be used when basing the clinical diagnosis on this examination maneuver alone. The test is not sensitive but is specific for cervical radiculopathy and can be used to help confirm this diagnosis.
In addition to clearing the cervical spine centrally, clearing the glenohumeral joint is important. Determining the presence of concomitant impingement or instability is also recommended. Use of the sulcus sign to determine the presence of multidirectional instability of the glenohumeral joint, along with the subluxation–relocation sign and load and shift test, can provide valuable insight into the status of the glenohumeral joint. The impingement signs of Neer (1983) and Hawkins and Kennedy (1980) are also helpful to rule out proximal tendon pathology.
Therefore, removal of the patient’s shirt or examination of the patient in a gown with full exposure of the upper back is highly recommended. Kibler et al. (2002) devised a classification system for scapular pathology. Careful observation of the patient at rest and with the hands placed on the hips, and during active overhead movements, is recommended to identify prominence of particular borders of the scapula and a lack of close association with the thoracic wall during movement. Bilateral comparison forms the primary basis for identifying scapular pathology; however, in many athletes, bilateral scapular pathology can be observed.
Some of the most useful tests for identifying humeral epicondylitis include the use of provocation tests to screen the muscle tendon units of the elbow. Provocation tests consist of manual muscle tests to determine pain reproduction. The specific tests used to screen the elbow joint of a patient with suspected elbow pathology include wrist and finger flexion and extension (Fig. 2-8) and forearm pronation and supination. These tests can be used to provoke the muscle tendon unit at the lateral or medial epicondyle. Testing of the elbow at or near full extension can often recreate localized lateral or medial elbow pain secondary to tendon degeneration. Reproduction of lateral or medial elbow pain with resistive muscle testing (provocation testing) may indicate concomitant tendon injury at the elbow and would direct the clinician to perform a more complete elbow examination. In addition to the provocation tests themselves, careful palpation of the extensor origin at the lateral epicondyle and medial epicondyle is also indicated. Careful inspection of the orientation of the tendons on the lateral epicondyle shows that the primary insertion of the extensor carpi radialis longus is actually on the lateral supracondylar ridge proximal to the lateral humeral epicondyle. Additionally, the extensor carpi radialis brevis (ECRB) can be palpated on the medial aspect of the lateral epicondyle just proximal to the extensor digitorum communis (EDC), with the extensor carpi ulnaris being just distal to the EDC.
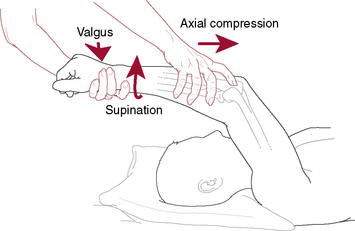
One of the more recent elbow special tests described in the literature is the moving valgus test. This test is performed with the patient’s upper extremity in approximately 90 degrees of abduction (Fig. 2-9). The elbow is maximally flexed and a moderate valgus stress is imparted to the elbow to simulate the late cocking phase of the throwing motion. Maintaining the modest valgus stress on the elbow, the elbow is extended from the fully flexed position. A positive test for ulnar collateral ligament injury is confirmed when reproduction of the patient’s pain occurs and is maximal over the medial ulnar collateral ligament between 120 and 70 degrees in what we have termed the “shear angle” or pain zone. O’Driscoll et al. (2005) examined 21 athletes with a primary complaint of medial elbow pain from medial collateral ligament insufficiency or other valgus overload abnormality using the moving valgus test. The moving valgus test was found to be highly sensitive (100%) and specific (75%) when compared with arthroscopic exploration of the medial ulnar collateral ligament. The mean angle of maximal pain reproduction in their study was 90 degrees of elbow flexion. This test can provide valuable clinical input during the evaluation of the patient with medial elbow pain.
Treatment
Tendinitis versus Tendinosis
Lateral humeral epicondylitis represents a frequent overuse injury. Wilson and Best (2005) noted that there is a common misconception that symptomatic tendon injuries are inflammatory; because of this, these injuries often are mislabeled as “tendinitis.” Acute inflammatory tendinopathies exist, but many patients have chronic symptoms, suggesting a degenerative condition that should be labeled as “tendinosis” or tendinopathy.” A number of terms have been used to describe lateral humeral epicondylitis, including tennis elbow, epicondylalgia, tendinitis, tendinosis, and tendinopathy (Stasinopoulos and Johnson 2006), often preceded by extensor or lateral elbow. Lateral elbow tendinopathy seems to be the most appropriate term to use in clinical practice because other terms make reference to inappropriate etiologic, anatomic, and pathophysiologic terms. The correct diagnostic term is important for the right treatment.
Zeisig et al. (2006) and Riley (2008) noted that tennis elbow or ECRB tendinosis is a condition with an unknown etiology and pathogenesis that is difficult to treat. Croisier et al. (2007) reported that, in spite of the many conservative treatment procedures, prolonged symptoms and relapse are frequent. Most treatment options have yet to be evaluated for efficacy in well-designed clinical trials, yet there is a generally favorable response to nonoperative or conservative management. Wilson and Best (2005) and Gabel (1999) indicated that most patients with overuse tendinopathies (about 80%) fully recover within 3 to 6 months.
Definitions: tendinitis and tendinosis
Several studies have described the histopathologic findings with tennis elbow as chronic degeneration, regeneration, and microtears of the tendinous tissue called tendinosis. Neurochemicals including glutamate, substance P, and calcitonin gene-related peptides have been identified in patients with chronic tennis elbow and in animal models of tendinopathy. More recent research shows that tendons exhibit areas of degeneration and a distinct lack of inflammatory cells (Ashe et al. 2004). Consequently, tendinosis is degeneration of the collagen tissue as a result of aging, microtrauma, or vascular compromise. Riley (2005) described the tendon matrix as being maintained by the resident tenocytes, and there is evidence of a continuous process of matrix remodeling, although the rate of turnover varies at different sites. A change in remodeling activity is associated with the onset of tendinopathy and some changes are consistent with repair, but they may also be an adaptive response to changes in mechanical loading. Additionally, repeated minor strain is thought to be the major precipitating factor in tendinopathy. Metalloproteinase enzymes have an important role in the tendon matrix; the role of these enzymes in tendon pathology is unknown, and further work is required to identify novel and specific molecular targets for therapy. Riley (2008) also reported that the neuropeptides and other factors released by stimulated cells or nerve endings in or around the tendon might influence matrix turnover and could provide novel targets for therapeutic intervention.
Alfredson and Ohberg (2005) using color Doppler examination showed structural tendon changes with hypoechoic areas and a local neovascularization, corresponding to the painful area. They demonstrated that treatment with sclerosing injections, targeting the area with neovessels, has the potential to eliminate pain in the tendons and allow patients to go back to full patellar tendon loading activity. Ohberg and Alfredson (2004) examined the occurrence of neovascularization in the Achilles tendon before and after eccentric training. After 12 weeks of painful eccentric calf muscle training, there was a more normal tendon structure, and in the majority of the tendons there was no remaining neovascularization.
Additionally, Ohberg et al. (2004) reported that after a 12-week eccentric calf muscle training program most patients with mid-portion painful chronic Achilles tendinosis showed a localized decrease in tendon thickness and a normalized tendon structure in most patients. Remaining structural tendon abnormalities seemed to be associated with residual pain in the tendon. Fredberg and Stengaard-Pedersen (2008) stated that, although the prevailing opinion is that no histologic evidence of acute inflammation has been documented, newer studies using immunohistochemistry and flow cytometry inflammatory cells have been detected. Consequently, the “tendinitis myth” needs to continue to be investigated. Existing data indicate that the initiators of the tendinopathic pathway include many proinflammatory agents. Because of the complex interaction between the classic proinflammatory agents and neuropeptides, it seems impossible and somewhat irrelevant to distinguish between chemical and neurogenic inflammation. Furthermore, glucocorticoids are, at the moment, an effective treatment in tendinopathy with regard to reduction of pain, tendon thickness, and neovascularization. An inflammatory process may be related not only to the development of tendinopathy, but also to chronic tendinopathy.
Wilson and Best (2005) described many of the clinical findings of tendinopathy. The natural history is gradually increasing load-related localized pain coinciding with increased activity. The examination should check for the signs of inflammation (swelling, pain, erythema, and heat), which would be indicative of a tendinitis response, asymmetry, ROM testing, palpation for tenderness, and examination maneuvers that simulate tendon loading and reproduce pain. Despite the absence of inflammation, patients with tennis elbow present with pain. Zeisig et al. (2006) suggested that the pain involves a neurogenic inflammation mediated via the neuropeptide substance P. Furthermore, the area with vascularity found in the extensor origin seems to be related to pain. Most likely, the findings correspond with the vasculo-neural in-growth that has been demonstrated in other painful tendinosis conditions.
There is no consensus regarding the optimal treatment for tendinitis or tendinosis. Paoloni et al. (2003) indicated that no treatment has been universally successful. Nirschl (1992) and Nirschl and Ashman (2004) described the primary goal of nonsurgical treatment as revitalization of the unhealthy tissue that produces pain. Revascularization and collagen repair of the pathologic tissue are keys to a successful rehabilitation program. Successful nonsurgical treatment involves rehabilitative resistance exercises and progression of the exercise program. A variety of treatment interventions have been reported in the literature, including hypospray, topical nitric oxide, oxygen free radicals, ice, phonophoresis and ultrasound, low-level laser, extracorporeal shock wave therapy, deep transverse friction massage (DTFM), manipulation and mobilization, acupuncture, bracing, orthotics, combined low-level laser and plyometrics, eccentric training programs, eccentric isokinetic program, and a combined exercise program.
Manias and Stasinopoulos (2006) compared an exercise program alone to the same program supplemented by icing. There were no significant differences in the magnitudes of reduction between the groups at the end of treatment and at the 3-month followup. However, because of the confounding variables with multiple treatment interventions, it is difficult to determine the efficacy of icing. Klaiman et al. (2007) demonstrated that ultrasound resulted in decreased pain and increased pressure tolerance in selected soft-tissue injuries. The addition of phonophoresis with fluocinonide did not increase the benefits of ultrasound alone.
Bjordal et al. (2008) performed a systematic review and meta-analysis of studies reporting low-level laser therapy (LLLT) for the treatment of humeral epicondylitis. Twelve randomized controlled trials satisfied the methodological inclusion criteria. LLLT administered with optimal doses of 904 nm and possibly 632 nm wavelengths directly to the lateral elbow tendon insertions seemed to offer short-term pain relief and less disability in humeral epicondylitis, both alone and in conjunction with an exercise regimen. Stasinopoulos and Johnson (2005) in a qualitative analysis of nine studies found poor results with LLLT for humeral epicondylitis because it is a dose-response modality and the optimal treatment dosage has not been identified.
Rompe and Maffulli (2007) performed a qualitative study-by-study assessment that was thought to be of greater relevance than a pooled meta-analysis of statistically and clinically heterogeneous data of randomized controlled studies, which are difficult to interpret. In a qualitative systematic per-study analysis identifying common and diverging details of 10 randomized controlled trials that included 948 participants, evidence was found for effectiveness of shockwave treatment for tennis elbow under well-defined, restrictive conditions only.
Brosseau et al. (2002) in a Cochrane review determined that deep tendon friction massage (DTFM) combined with other physiotherapy modalities did not show consistent benefit in the control of pain or improvement of grip strength and functional status for patients with extensor carpi radialis tendinitis. LLLT and plyometrics were more effective using a variety of outcome measures than plyometrics by themselves for treatment of lateral humeral epicondylitis.
Eccentric training programs
One variable studied with specific regard to the treatment of tendon pathology is the use of eccentric exercise. There is limited research regarding the efficacy of eccentric overload training for humeral epicondylitis and treatment of other tendon overuse injuries. Kingma et al. (2007) performed a systematic review of eccentric overload training in patients with chronic Achilles tendinopathy. The nine included trials showed an improvement in pain after eccentric overload training; however, because of the methodological shortcomings of the trials, no definite conclusion could be drawn concerning the effects of eccentric overload training. Although the effects of eccentric exercise training in tendinopathy on pain are promising, the magnitude of the effects cannot be determined. Knobloch et al. (2007) using a laser Doppler system for capillary blood flow, tissue oxygen saturation, and postcapillary venous filling pressure evaluated the tendon’s microcirculation in response to a 12-week daily painful home-based eccentric training regimen (3 × 15 repetitions per tendon each day). They found daily eccentric training for Achilles tendinopathy to be a safe and easy measure, with beneficial effects on the microcirculatory tendon levels without any adverse effects in both mid-portion and insertional Achilles tendinopathy. Malliaras et al. (2008), in a review of eccentric training programs for humeral epicondylitis, determined that eccentric training has demonstrated encouraging results, although the literature is limited and eccentric programs are varied.
Combined exercise programs
Stasinopoulos et al. (2005) described strengthening and stretching exercise programs for the treatment of humeral epicondylitis. They recommended slow progressive eccentric exercises done with the elbow in extension, forearm in pronation, and wrist in an extended position. However, the speed of loading and the details (repetitions, sets, volume) of the eccentric exercise programs were not defined. They also recommended static stretching exercises to the lateral muscle-tendon unit before and after the eccentric exercises for 30 to 45 seconds with a 30-second rest interval between exercises. The details of the optimal parameters for treating humeral epicondylitis have yet to be elucidated in a well-designed trial.
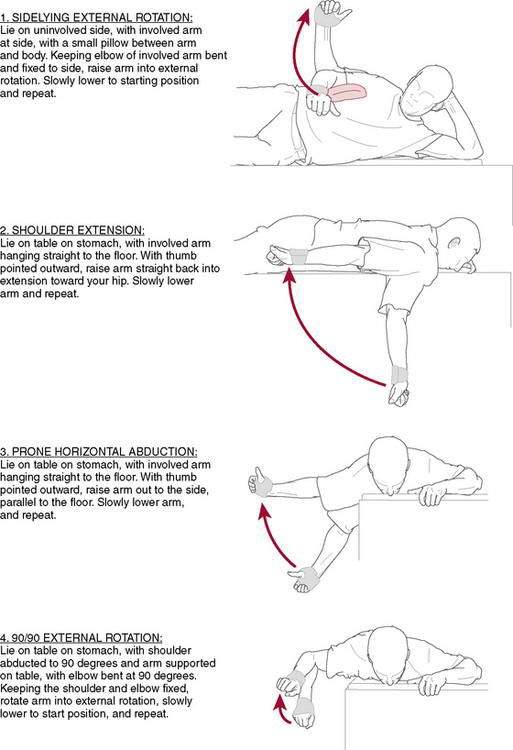
Rotator cuff and scapular stabilization
In addition to the use of therapeutic modalities and eccentric exercise to directly treat the injured tendon at the elbow, proximal stabilization and exercise techniques also are warranted during the treatment of an athlete with an overuse elbow injury. Several key scapular strengthening exercises are recommended that target strengthening of the lower trapezius and serratus anterior force couple. Scapular stabilization exercises are emphasized and include external rotation with retraction, an exercise shown to recruit the lower trapezius at a rate 3.3 times more than the upper trapezius and utilize the important position of scapular retraction. Multiple seated rowing variations are recommended. These include the lawn mower exercise and low row variations, which have been studied with electromyographic quantification by Kibler et al. (2008).
Progression to closed-chain exercise using the “plus” position, which is characterized by maximal scapular protraction, has been recommended by Moesley et al. (1992) and Decker et al. (1999) for its inherent maximal serratus anterior recruitment. Closed-chain step-ups, quadruped position rhythmic stabilization, and variations of the pointer position (unilateral arm and ipsilateral leg extension weightbearing) are all used in endurance-oriented formats (timed sets of 30 seconds or more) to enhance scapular stabilization. Uhl et al. (2003) demonstrated the effects of increasing weightbearing and successive decreases in the number of weightbearing limbs on muscle activation of the rotator cuff and scapular musculature and provide guidance to closed-chain exercise progression in the upper extremity.
Strengthening the posterior rotator cuff to provide strength, fatigue resistance, and optimal muscle balance is of paramount importance when working with athletic individuals. Figure 2-10 shows our recommended exercises for rotator cuff strengthening. These exercises are based on EMG research showing high levels of posterior rotator cuff activation. Use of the prone horizontal abduction exercise is emphasized because research has shown this position creates high levels of supraspinatus muscular activation, making it an alternative to the widely used empty can exercise, which often can cause impingement because of the combined inherent movements of internal rotation and elevation. Three sets of 15 to 20 repetitions are recommended to create a fatigue response and improve local muscular endurance. For patients with elbow dysfunction, these exercises can be performed using a cuff weight attached proximal to the elbow if the distal weight attachment provokes pain or stresses the healing elbow structures. These isotonic exercises are coupled with an external rotation exercise with elastic resistance to provide resistance to the posterior rotator cuff in both neutral and 90-degree abducted positions in the scapular plane.
Carter et al. (2007) studied the effects of an 8-week program of plyometric upper extremity exercise and external rotation strengthening with elastic resistance. They found increased eccentric external rotation strength, concentric internal rotation strength, and improved throwing velocity in collegiate baseball players. Figure 2-11 shows a prone 90/90 plyometric exercise with the athlete maintaining a retracted scapular position with the shoulder in 90 degrees of abduction and 90 degrees of external rotation. The plyo ball is rapidly dropped and caught over a 2- to 3-inch (3 to 6 cm) movement distance for sets of 30 to as much as 40 seconds to increase local muscular endurance. This exercise also provides a fatigue response to the wrist flexors and extensors as a result of the rapid grasping and releasing of the ball during the exercise. Another exercise used in elbow rehabilitation is the reverse-catch plyometric exercise that is performed with the glenohumeral joint in the 90/90 position. The ball is tossed from behind the patient to eccentrically load the posterior rotator cuff (external rotators) with a rapid concentric external rotation movement performed as the patient throws the ball back, keeping the abducted position of the shoulder with 90 degrees of elbow flexion. These one-arm plyometric exercises can be preceded by two-arm catches over the shoulder to determine readiness for the one-arm loading. Small (0.5 kg, 1-pound) medicine balls or soft weights (Theraband, Hygenic Corporation, Akron, OH) are used initially with progression to 1 to 1.5 kg as the patient progresses in both skill and strength development.
Advanced distal upper extremity exercises for rehabilitation of humeral epicondylitis
More advanced, ballistic-type exercises can be integrated for end-stage strengthening in patients returning to aggressive work activity or in athletes who need high levels of muscular strength and endurance. Rapid ball dribbling in sets of 30 seconds with a basketball or small physio ball both off the ground and in an elevated position off the wall (Fig. 2-12) is recommended. Additionally, specific plyometric drills for the forearm musculature include wrist flexion flips and wrist flexion snaps.
Return to sport/interval return programs
An interval tennis program has been published and the reader is referred to these publications for additional discussion of this important process (Ellenbecker et al. 2006). Additionally, similar concepts are used in the interval throwing program, which has been published previously (Reinhold et al. 2002). Similar to the interval tennis program, having the patient’s throwing mechanics evaluated using video and by a qualified coach or biomechanist is a very important part of the return-to-activity phase of the rehabilitation process.
Elbow Arthroplasty
Tigran Garabekyan, MD, and Charles E. Giangarra, MD
Indications for elbow arthroplasty include the following:
Contraindications for elbow arthroplasty include the following:
Relative
Elbow prostheses are classified as semiconstrained (loose-hinge or sloppy-hinge), nonconstrained (minimally constrained), or fully constrained. Fully constrained prostheses are no longer used because of their unacceptably high failure rate. See Rehabilitation Protocol 2-6 for rehabilitation following total elbow replacement.
REHABILITATION PROTOCOL 2-6 Rehabilitation Protocol After Total Elbow Replacement
Week 1
Week 2
Pediatric elbow injuries in the throwing athlete: emphasis on prevention
Adirim T.A., Cheng T.L. Overview of injuries in the young athlete. Sports Med. 2003;33:75-81.
Committee on Sports Medicine and Fitness. American Academy of Pediatrics: risk of injury from baseball and softball in children. Pediatrics. 2001;107:782-784.
Cox K., Manske R.C., Stovak M. Unpublished research. Do high school coaches follow the recommendations of USA Baseball Medical and Safety Advisory Committee?; 2009.
Crowther M. Elbow pain in pediatrics. Curr Rev Musculoskelet Med. 2009;2:83-87.
Emery C.A. Risk factors for injury in child and adolescent sport: a systematic review of the literature. Clin J Sport Med. 2003;13:256-268.
Ireland M.L., Andrews J.R. Shoulder and elbow injuries in the young athlete. Clin Sports Med. 1988;7:473-494.
Joyce M.E., Jelsma R.D., Andrews J.R. Throwing injuries to the elbow. Sports Med Arthroscopy Rev. 1995;3:224-236.
Lyman S., Fleisig G.S., Waterbor J.W., et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33:1803-1810.
Lyman S., Fleisig G.S., Andrews J.R., et al. Effect of pitch type, pitch count and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468.
Pappas A.M. Elbow problems associated with baseball during childhood and adolescence. Clin Orthop. 1982;164:30-41.
Petty D.H., Andrews J.R., Fleisig G.S. Ulnar collateral ligament reconstruction in high school baseball players. Clinical results and injury risk factors. Am J Sports Med. 2004;32:1158-1164.
Rudzki J.R., Paletta G.A. Juvenile and adolescent elbow injuries in sports. Clin Sports Med. 2004;23:581-608.
USA Baseball Medical and Safety Advisory Committee. Position statement on youth baseball injuries. Accessed online at http://www.usabaseball.com/pt/usab-med-safety-list.html.
Yadao M.A., Field L.D., Savoie F.H. Osteochondritis dissecans of the elbow. AAOS Instructional Course Lectures. 2004;53:599-606.
Altchek D.W., Andrews J.R. The Athlete’s Elbow, ed 1. Philadelphia,: Lippincott Williams & Wilkins, 2001.
Altchek D.W., Levinson M. Rehab after MCL reconstruction. Biomech. 2001;5:22-28.
Dines J.S., Frank J.B., Akerman M., et al. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566-570.
Dodson C.C., Thomas A., Dines J.S., et al. Medial ulnar collateral reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34:1926-1933.
Keefe D.T., Lintner D.M. Nerve injuries in the throwing elbow. Clin Sports Med. 2004;23:723-742.
Levinson M. Ulnar collateral ligament reconstruction. In Cioppa-Mosca J., Cahill J., Young Tucker C., editors: Postsurgical Rehabilitation Guidelines for the Orthopedic Clinician, ed 1, St. Louis: Elsevier, 2006.
Rettig A.C., Sherill C., Dale S., et al. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29:15-17.
Rouhrbough J.T., Altchek D.W., Hyman J., et al. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541-548.
Wilk K.E., Levinson M. Rehabilitation of the athlete’s elbow. In Altchek D.A., Andrews J.R., editors: The Athlete’s Elbow, ed 1, Philadelphia: Lippincott Williams & Wilkins, 2001.
Gelinas J.J., Faber K.J., Patterson S.D., et al. The effectiveness of turnbuckle splinting for elbow contractures. J Bone Joint Surg Br. 2000;82(1):74-78.
Hastings H.2nd, Graham T.J. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;10(3):417-437.
Kay N.R. Arthrolysis of the post-traumatic stiff elbow. In: Stanley D., Kay N.R., editors. Surgery of the elbow. London: Arnold, 1998.
Morrey B.F. Total elbow arthroplasty did not differ from open reduction and internal fixation with regard to reoperation rates. J Bone Joint Surg Am. 2009;91(8):2010.
Morrey B.F., Askew L.J., Chao E.Y. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872-877.
Søjbjerg J.O. The stiff elbow. Acta Orthop Scand. 1996;67:262-331.
Bennett J.B., Mehlhoff T.L. Total elbow arthroplasty: surgical technique. J Hand Surg Am. 2009;34(5):933-939.
Bruno R.J., Lee M.L., Strauch R.J., et al. Posttraumatic elbow stiffness: evaluation and management. J Am Acad Orthop Surg. 2002;10(2):106-116.
Cain E.L.Jr, Dugas J.R., Wolf R.S., et al. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621-635.
Chen F.S., Rokito A.S., Jobe F.W. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9(2):99-113.
Cheung E.V., Adams R., Morrey B.F. Primary osteoarthritis of the elbow: current treatment options. J Am Acad Orthop Surg. 2008;16(2):77-87.
Evans P.J., Nandi S., Maschke S., et al. Prevention and treatment of elbow stiffness. J Hand Surg Am. 2009;34(4):769-778.
Gramstad G.D., Galatz L.M. Management of elbow osteoarthritis. J Bone Joint Surg Am. 2006;88(2):421-430.
Kauffman J.I., Chen A.L., Stuchin S., et al. Surgical management of the rheumatoid elbow. J Am Acad Orthop Surg. 2003;11(2):100-108.
Kokkalis Z.T., Schmidt C.C., Sotereanos D.G. Elbow arthritis: current concepts. J Hand Surg Am. 2009;34(4):761-768.
Lindenhovius A.L., Jupiter J.B. The posttraumatic stiff elbow: a review of the literature. J Hand Surg Am. 2007;32(10):1605-1623.
Morrey B.F. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am. 1990;72(4):601-618.
O’Holleran J.D., Altchek D.W. The thrower’s elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J. 2006;2(1):83-93.
van der Lugt J.C., Rozing P.M. Systematic review of primary total elbow prostheses used for the rheumatoid elbow. Clin Rheumatol. 2004;23(4):291-298.
Broberg M.A., Morrey B.F. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;216:109-119.
Durig M., Muller W., Ruedi T.P., et al. The operative treatment of elbow dislocation in the adult. J Bone Joint Surg Am. 1979;61:239-244.
Hastings H.I.I., Graham T.J. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;10:417-438.
Husband J.B., Hastings H.I.I. The lateral approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg Am. 1990;72:1353-1358.
Josefsson P.O., Johnell O., Gentz C.F. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66:927-930.
Josefsson P.O., Johnell O., Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop. 1987;221:221-225.
Josefsson P.O., Nilsson B.E. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57:537-538.
Lansinger O., Karlsson J., Korner L., et al. Dislocation of the elbow joint. Arch Orthop Trauma Surg. 1984;102:183-186.
Linscheid R.L., Wheeler D.K. Elbow dislocations. JAMA. 1965;194:1171-1176.
Mehloff T.L., Noble P.C., Bennett J.B., et al. Simple dislocation of the elbow in the adult: Results after closed treatment. J Bone Joint Surg Am. 1988;70:244-249.
Mezera K., Hotchkiss R.N. Fractures and dislocations of the elbow. In Rockwood C.A., Bucholz R.W., Heckman J.D., Green D.P., editors: Rockwood and Green’s Fractures in Adults, ed 5, Philadelphia, PA: Lippincott-Raven, 2001.
Morrey B.F. Applied anatomy and biomechanics of the elbow joint. Instr Course Lect. 1986;35:59-68.
Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. J Bone Joint Surg Am. 1995;77:316-327.
Morrey B.F., editor. The Elbow and Its Disorders, ed 2, Philadelphia: WB Saunders, 1993.
O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73:440-446.
Pugh D.M.W., Wild L.M., Schemitsch E.H., et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86:1122-1130.
Cohen M.S., Hastings H.H. Rotatory instability of the elbow: The role of the lateral stabilizers. J Bone Joint Surg Am. 1997;79:225-233.
Josefsson P.O., Gentz C.F., Johnell O., et al. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint: A prospective randomized study. J Bone Joint Surg Am. 1987;69:605-608.
Josefsson P.O., Gentz C.F., Johnell O., et al. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. Clin Orthop. 1987;214:165-169.
Osborne G., Cotterill P. Recurrent dislocation of the elbow. J Bone Joint Surg Br. 1966;48B:340-346.
Lateral and medial humeral epicondylitis
Alfredson H., Ohberg L. Neovascularization in chronic painful patellar tendinosis-promising results after sclerosing neovessels outside the tendon challenge the need for surgery. Knee Surg Sports Traumatol Arthrosc. 2005;13:74-80.
Andrews J.R., Wilk K.E., Satterwhite Y.E., et al. Physical examination of the thrower’s elbow. J Orthop Sport Phys Ther. 1993;6:296-304.
Ashe M.C., McCauley T., Khan K.M. Tendinopathies in the upper extremity: a paradigm shift. J Hand Ther. 2004;17:329-334.
Bjordal J.M., Lopes-Martins R.A., Joensen J., et al. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskelet Disord. 2008;9:75.
Brosseau L., Casimiro L., Milne S., et al. Deep transverse friction massage for treating tendinitis. Cochrane Database Syst Rev. 4, 2002. CD003528,
Carter A.B., Kaminski T.W., Douex A.T.Jr, et al. Effects of high volume upper extremity plyometric training on throwing velocity & functional strength ratios of the shoulder rotators in collegiate baseball players. J Strength Cond Res. 2007;21(1):208-215.
Chinn C.J., Priest J.D., Kent B.E. Upper extremity range of motion, grip strength, and girth in highly skilled tennis players. Phys Ther. 1974;54:474-482.
Croisier J.L., Foidart-Dessalle M., Tinant F., et al. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007;41:269-275.
Decker M.J., Hintermeister R.A., Faber K.J., et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med. 1999;27:784-791.
Dines J.S., Frank J.B., Akerman M., et al. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament deficiency. Am J Sports Med. 2009;37(3):566-570.
Ellenbecker T.S. A total arm strength isokinetic profile of highly skilled tennis players. Isokinet Exerc Sci. 1991;1:9-21.
Ellenbecker T.S., Mattalino A.J. The Elbow in Sport. Champaign, IL: Human Kinetics Publishers, 1997.
Ellenbecker T.S., Roetert E.P., Bailie D.S., et al. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34(12):2052-2056.
Ellenbecker T.S., Roetert E.P. Age specific isokinetic glenohumeral internal and external rotation strength in elite junior tennis players. J Sci Med Sport. 2003;6(1):63-70.
Ellenbecker T.S., Roetert E.P. Unpublished material, Data from the USTA on range of motion of the elbow and wrist in senior tennis players, 1994.
Ellenbecker T.S., Roetert E.P. Isokinetic profile of elbow flexion and extension strength in elite junior tennis players. J Orthop Sports Phys Ther. 2003;33(2):79-84.
Ellenbecker T.S., Wilk K.E., Reinold M.M., et al. Use of interval return programs for shoulder rehabilitation. In: Ellenbecker T.S., editor. Shoulder Rehabilitation: Non Operative Treatment. New York: Thieme, 2006.
Fredberg U., Stengaard-Pedersen K. Chronic tendinopathy tissue pathology, pain mechanisms, and etiology with a special focus on inflammation. Scand J Med Sci Sports. 2008;18:3-15.
Gabel G.T. Acute and chronic tendinopathies at the elbow. Curr Opin Rheumatol. 1999;11:138-143.
Goldie I. Epicondylitis lateralis humeri. Acta Chir Scand Suppl. 1964;339:1.
Gould J.A. The spine. In: Gould J.A., Davies G.J., editors. Orthopaedic and Sports Physical Therapy. St Louis: Mosby, 1985.
Hawkins R.J., Kennedy J.C. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151-158.
Kibler W.B., Sciascia A.D., Uhl T.L., et al. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36:1789-1798.
Kibler W.B., Uhl T.L., Maddux J.W.Q., et al. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550-556.
King J.W., Brelsford H.J., Tullos H.S. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res. 1969;67:116-123.
Kingma J.J., deKnikker R., Wittink H.M., et al. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med. 2007;41:E3.
Klaiman M.D., Shrader J.A., Danoff J.V., et al. Phonophoresis versus ultrasound in the treatment of common musculoskeletal conditions. Med Sci Sports Exerc. 1998;30:1349-1355.
Knobloch K. Eccentric training in Achilles tendinopathy: is it harmful to tendon microcirculation? Br J Sports Med. 2007;41:e2.
Knobloch K., Kraemer R., Jagodzinski M., et al. Eccentric training decreases paratendon capillary blood flow and preserves paratendon oxygen saturation in chronic Achilles tendinopathy. J Orthop Sports Phys Ther. 2007;37:269-276.
Kraushaar B.S., Nirschl R.P. Tendinosus of the elbow (tennis elbow). Clinical features and findings of histopathological, immunohistochemical and electron microscopy studies. J Bone Joint Surgery Am. 1999;81:259-278.
Leadbetter W.B. Cell matrix response in tendon injury. Clin Sports Med. 1992;11:533-579.
Magee D.J. Orthopedic Physical Assessment, ed 3. Philadelphia: Saunders, 1997.
Malliaras P., Maffulli N., Garau G. Eccentric training programs in the management of lateral elbow tendinopathy. Disabil Rehabil. 2008;30:1590-1596.
Manias P., Stasinopoulos D.A. Controlled clinical pilot trial to study the effectiveness of ice as a supplement to the exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med. 2006;40:81-85.
Moesley J.B., FW Jobe M. Pink M: EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20:128.
Morrey B.F. The Elbow and Its Disorders, ed 2. Philadelphia: Saunders, 1993.
Neer C.S. Impingement lesions. Clin Orthop. 1983;173:70-77.
Nirschl R.P. Elbow tendinosis/tennis elbow. Clin Sports Med. 1992;11:851-870.
Nirschl R.P., Ashman E.S. Elbow tendinopathy: tennis elbow. Clin Sports Med. 2003;22:813-836.
Nirschl R.P., Ashman E.S. Tennis elbow tendinosis (epicondylitis). Instr Course Lect. 2004;53:587-598.
Nirschl R.P., Rodin D.M., Ochiai D.H., et al. Iontophoretic administration of dexamethasone sodium phosphate for acute epicondylitis: a randomized, double blind, placebo controlled study. Am J Sports Med. 2003;31(2):189-195.
Nirschl R.P., Sobel J. Conservative treatment of tennis elbow. Phys Sportsmed. 1981;9:43-54.
O’Driscoll S.W., Lawton R.L., Smith A.M. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33(2):231-239.
Ohberg L., Alfredson H. Effects of neovascularization behind the good results with eccentric training in chronic mid-portion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc. 2004;12:465-470.
Ohberg L., Lorentzon R., Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: a normalized tendon structure and decreased thickness at follow up. Br J Sports Med. 2004;38:8-11.
Paoloni J.A., Appleyard R.C., Nelson J., et al. topical nitric oxide application in the treatment of chronic tendinosis at the elbow: a randomized, double-blinded, placebo controlled clinical trial. Am J Sports Med. 2003;31:915-920.
Priest J.D., Jones H.H., Nagel D.A. Elbow injuries in highly skilled tennis players. J Sports Med. 1974;2(3):137-149.
Priest J.D., Jones H.H., Tichenor C.J.C., et al. Arm and elbow changes in expert tennis players. Minn Med. 1977;60:399-404.
Reinold M.M., Wilk K.E., Reed J., et al. Internal sport programs: guidelines for baseball, tennis, and golf. J Orthop Sports Phys Ther. 2002;32:293-298.
Riley G. Chronic tendon pathology: molecular basis and therapeutic implications. Expert Rev Mol Med. 2005;7:1-25.
Riley G. Tendinopathy—from basic science to treatment. Nat Clin Pract Rheumatol. 2008;4:82-89.
Rompe J.D., Maffulli N. Repetitive shock wave therapy for lateral tendinopathy: tennis elbow: a systematic and qualitative analysis. Br Med Bull. 2007;83:355-378.
Runge F. Zur genese unt behand lung bes schreibekramp fes. Berl Klin Woschenschr. 1873;10:245.
Safran M.R., McGarry M.H., Shin S., et al. Effects of elbow flexion and forearm rotation on valgus laxity of the elbow. J Bone Joint Surg Am. 2005;87(9):2065-2074.
Stasinopoulos D., Johnson M.I. “Lateral elbow tendinopathy” is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis. Med Hypotheses. 2006;67:1400-1402.
Stasinopoulos D., Stasinopoulos I., Johnson M.I. An exercise program for the management of lateral elbow tendinopathy. Br J Sports Med. 2005;39:944-947.
Stasinopoulos D.I., Johnson M.I. Effectiveness of low-level laser therapy for lateral elbow tendinopathy. Photomed Laser Surg. 2005;23:425-430.
Tong H.C., Haig A.J., Yamakawa K. The Spurling test and cervical radiculopathy. Spine. 2002;27(2):156-159.
Uhl T.L., Carver T.J., Mattacola C.G., et al. Shoulder musculature activation during upper extremity weightbearing exercise. J Orthop Sports Phys Ther. 2003;33(3):109-117.
Waslewski G.L., Lund P., Chilvers M., et al. MRI evaluation of the ulnar collateral ligament of the elbow in asymptomatic, professional baseball players, 2002. Paper presented at the AOSSM Meeting
Wilk K.E., Arrigo C.A., Andrews J.R. Rehabilitation of the elbow in the throwing athlete. J Orthop Sports Phys Ther. 1993;17:305-317.
Wilson J.J., Best T.M. Common overuse tendon problems: a review and recommendations for treatment. Am Fam Physician. 2005;72:811-818.
Wright R.W., Steeger May K., Wasserlauf B.I., et al. Elbow range of motion in professional baseball pitchers. Am J Sports Med. 2006;34(2):190-193.
Zeisig E., Ohberg L., Alfredson H. Extensor origin vascularity related to pain in patients with tennis elbow. Knee Surg Sports Traumatol Arthrosc. 2006;14:659-663.
Adelsberg S. An EMG analysis of selected muscles with rackets of increasing grip size. Am J Sports Med. 1986;14:139-142.
Bagg S.D., Forrest W.J. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane. Arch Phys Med Rehabil. 1988:238-245.
Blackburn T.A., McLeod W.D., White B., et al. EMG analysis of posterior rotator cuff exercises. Athletic Training. 1990;25:40.
Borsa P.A., Dover G.C., Wilk K.E., et al. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38(1):21-26.
Boyer M.I., Hastings H. Lateral tennis elbow: is there any science out there? J Shoulder Elbow Surg. 1999;8:481-491.
Carroll R. Tennis elbow: incidence in local league players. Br J Sports Med. 1981;15:250-255.
Coonrad R.W., Hooper W.R. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg. 1973;55-A:1177-1182.
Cyriax J.H., Cyriax P.J. Illustrated Manual of Orthopaedic Medicine. London: Butterworth, 1983.
Dunn J.H., Kim J.J., Davis L., et al. Ten- to 14-year follow-up on the Nirschl surgical procedure for lateral epicondylitis. Am J Sports Med. 2008;36(2):261-266.
Ellenbecker T.S. Rehabilitation of shoulder and elbow injuries in tennis players. Clin Sports Med. 1995;14(1):87-110.
Ellenbecker T.S., Mattalino A.J., Elam E.A., et al. Medial elbow laxity in professional baseball pitchers: a bilateral comparison using stress radiography. Am J Sports Med. 1998;26(3):420-424.
Eygendaal D., Rahussen F.T., Diercks R.L. Biomechanics of the elbow joint in tennis players and relation to pathology. Br J Sports Med. 2007;41:820-823.
Fedorczyk J.M. Tennis elbow: blending basic science with clinical practice. J Hand Ther. 2006;19:146-153.
Fleck S.J., Kraemer W.J. Designing Resistance Training Programs. Champaign, IL: Human Kinetics Publishers, 1987.
Fleisig G.S., Andrews J.R., Dillman C.J., et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233.
Glousman R.E., Barron J., Jobe F.W., et al. An electromyographic analysis of the elbow in normal and injured pitchers with medial collateral ligament insufficiency. Am J Sports Med. 1992;20:311-317.
Greenbaum B., Itamura J., Vangsness C.T., et al. Extensor carpi radialis brevis. J Bone Joint Surgery Br. 1999;81(5):926-929.
Groppel J.L., Nirschl R.P. A biomechanical and electromyographical analysis of the effects of counter force braces on the tennis player. Am J Sports Med. 1986;14:195-200.
Hang Y.S., Peng S.M. An epidemiological study of upper extremity injury in tennis players with particular reference to tennis elbow. J Formos Med Assoc. 1984;83:307-316.
Hughes G.R., Currey H.L. Hypospray treatment of tennis elbow. Ann Rheum Dis. 1969;28:58-62.
Ilfeld F.W., Field S.M. Treatment of tennis elbow. Use of a special brace. JAMA. 1966;195:67-70.
Jobe F.W., Kivitne R.S. Shoulder pain in the overhand or throwing athlete. Orthop Rev. 1989;18:963-975.
Kamien M. A rational management of tennis elbow. Sports Med. 1990;9:173-191.
Kibler W.B. Clinical biomechanics of the elbow in tennis. Implications for evaluation and diagnosis. Med Sci Sports Exerc. 1994;26:1203-1206.
Kibler W.B. Role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22(5):525-532.
Kibler W.B. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325-337.
Kibler W.B., Chandler T.J., Livingston B.P., et al. Shoulder range of motion in elite tennis players. Am J Sports Med. 1996;24(3):279-285.
Kulund D.N., Rockwell D.A., Brubaker C.E. The long term effects of playing tennis. Phys Sportsmed. 1979;7:87-92.
Maffulli N., Wong J., Almekinders L.C. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22:675-692.
Malanga G.A., Jenp Y.N., Growney E.S., et al. EMG analysis of shoulder positioning in testing and strengthening the supraspinatus. Med Sci Sports Exercise. 1996;28(6):661-664.
McCabe R.A., Tyler T.F., Nicholas S.J., et al. Selective activation of the lower trapezius muscle in patients with shoulder impingement. J Orthop Sports Phys Ther. 2001;31(1):A-45. (Abstract)
McFarland E.G., Torpey B.M., Carl L.A. Evaluation of shoulder laxity. Sports Med. 1996;22:264-272.
Morrey B., An K.N. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319.
Murrell G.A. Oxygen free radicals and tendon healing. J Shoulder Elbow Surg. 2007;16:S208-S214.
Ollivierre C.O., Nirschl R.P. Tennis elbow: Current concepts of treatment and rehabilitation. Sports Med. 1996;22(2):133-139.
Pfefer M.T., Cooper S.R., Uhl N.L. Chiropractic management of tendinopathy: a literature synthesis. J Manipulative Physiol Ther. 2009;32:41-52.
Reinhold M.M., Wilk K.E., Fleisig G.S., et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34(7):385-394.
Roetert E.P., Ellenbecker T.S., Brown S.W. Shoulder internal and external rotation range of motion in nationally ranked junior tennis players: a longitudinal analysis. J Strength Cond Res. 2000;14(2):140-143.
Rompe J.D., Furia J., Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional Achilles tendinopathy. A randomized controlled trial. J Bone Joint Surg. 2008;90-A:52-61.
Ryu K.N., McCormick J., Jobe F.W., et al. An electromyographic analysis of shoulder function in tennis players. Am J Sports Med. 1988;16:481-485.
Seil R., Wilmes P., Nuhrenborger C. Extracorporal shock wave therapy for tendinopathies. Expert Rev Med Devices. 2006;3:463-470.
Sems A., Dimeff R., Iannotti J.P. Extracorporeal shock wave therapy in the treatment of chronic tendinopathies. J Am Acad Orthop Surg. 2006;14:195-204.
Stasinopoulos D., Stasinopoulos I. Comparison of effects of exercise programme, pulsed ultrasound, and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil. 2004;18:347-352.
Stergioulas A. Effects of low-level laser and plyometric exercises in the treatment of lateral epicondylitis. Photomed Laser Surg. 2007;25:205-213.
Stergioulas A., Stergioula M., Aarskog R., et al. Effects of low-level laser therapy and eccentric exercises in the treatment of recreational athletes with chronic Achilles tendinopathy. Am J Sports med. 2008;36:881-887.
Stoddard A. Manipulation of the elbow joint. Physiother. 1971;57:259-260.
Townsend H., Jobe F.W., Pink M., et al. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1991;19:264.
United States Tennis Association: Unpublished Data.
Wainstein J.L., Nailor T.E. Tendinitis and tendinosis of the elbow, wrist and hands. Clin Occup Environ Med. 2006;5:299-322.
Winge S., Jorgensen U., Nielsen A.L. Epidemiology of injuries in Danish championship tennis. Int J Sports Med. 1989;10:368-371.