CHAPTER 21 Elbow blocks
Clinical anatomy
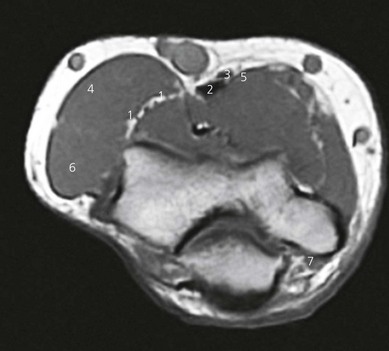
The three major nerves of the forearm can be blocked at the elbow (Fig. 21.1), and also the three cutaneous nerves of the forearm.
The median nerve, which lies anteromedially to the brachial artery near the axilla, crosses medial to the artery in the arm. At the elbow it lies between the tendons of brachialis and pronator teres, and deep to the bicipital aponeurosis. It passes between both heads of pronator teres to enter the forearm (Fig. 21.2). The median nerve provides sensory innervation to the lateral half of the palm, flexor aspect of the thumb, index finger, middle finger, and radial side of the ring finger.
The radial nerve passes between the long and medial head of the triceps to travel around the humerus and emerges on the anterior aspect of the arm above the brachioradialis. It passes deep to the brachioradialis over the lateral epicondyle, where it divides into a deep and a superficial branch (Fig. 21.2). The radial nerve provides sensation for the radial half of the dorsum of the hand, the back of the thumb, and part of the dorsum of the index finger.
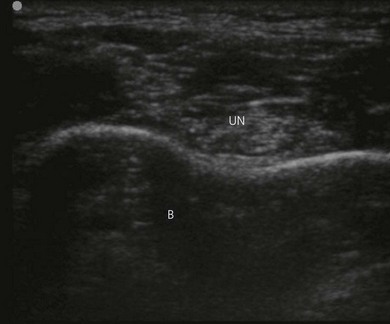
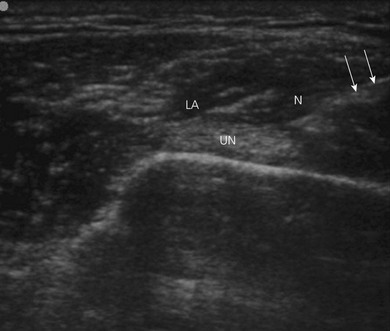
The ulnar nerve leaves the brachial artery halfway down the arm and passes behind the medial epicondyle in a fibrous tunnel. It passes between the two heads of flexor carpi ulnaris to enter the forearm (Fig. 21.3). The ulnar nerve provides sensation for the ulnar half of the dorsum of the hand, little finger, and ulnar side of the ring finger.
Surface anatomy
Important structures include the medial and lateral epicondyles of the humerus, olecranon process, intercondylar skin crease, biceps tendon, brachioradialis muscle, and brachial artery (Fig. 21.4). The biceps tendon can be palpated with elbow flexion beneath the intercondylar crease, and it runs laterally to the head of the radius. The brachioradialis muscle can be palpated lateral to the biceps tendon. The brachial artery is palpated medial to the biceps muscle.
Sonoanatomy
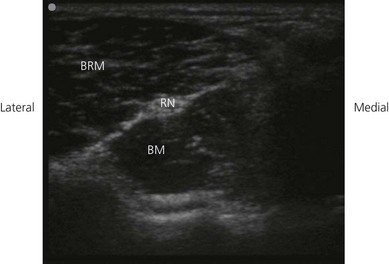
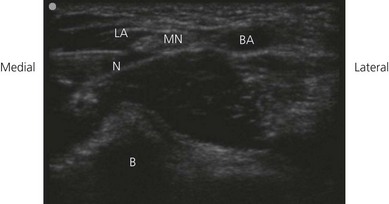
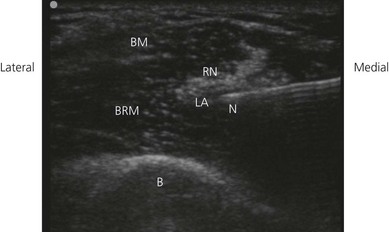
The examination begins with the patient supine, the arm abducted, the forearm supinated, and the wrist halfway between pronation and supination (Fig. 21.5). A systematic survey should be performed from superficial to deep and medial to lateral. A high frequency ultrasound transducer is used. With a transverse orientation, the median nerve is found medial to the brachial artery at the elbow as a hyperechoic structure (Fig. 21.6). This is on the medial side of the antecubital fossa. The radial nerve, after winding around the humerus, descends in the intermuscular septum between the brachialis and brachoradialis initially, and then the extensor carpi radialis. The radial nerve is easily seen with ultrasound, as the deep and superficial branches between the brachioradialis and brachialis muscles at the elbow. This nerve appears as a hyperechoic oval structure on the radial side of the antecubital fossa. The two key structures to identify include the hypoechoic brachioradialis and brachialis muscles. The radial nerve lies in the fascial thickening between these (Fig. 21.7). The ulnar nerve is seen posterior to the medial epicondyle at the elbow level in the condylar groove (Fig. 21.8).
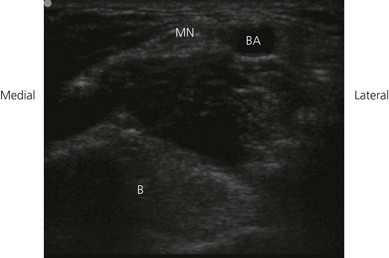
Figure 21.6 Sonosatomy relevant to median nerve block at the elbow. MN: median nerve; BA: brachial artery; B: bone.
Technique
Landmark-based approach
Median nerve block
Needle insertion for median nerve block is medial to the brachial pulse at the level of the intercondylar crease (Fig. 21.9). Needle orientation is cephalad and toward the humerus. The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms. The needle is advanced slowly until the appropriate muscle response is obtained: finger rather than wrist flexion. A loss of resistance is felt as the bicipital aponeurosis is punctured. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response. Wrist flexion may be due to direct muscle stimulation. Incremental injections of local anesthetic (4–6 mL) are made with repeated aspiration. If no twitch is found, ‘walk’ the needle in a medial to lateral plane.
Radial nerve block
Needle insertion for radial nerve block is halfway between the biceps tendon and lateral border of the arm (or 1 cm lateral to the biceps tendon), in the gutter between the biceps tendon and brachioradialis at the level of the intercondylar skin crease (Fig. 21.10). Needle orientation is cephalad and aimed toward the humerus (toward the lateral epicondyle). At a depth of 2–3 cm, the radial nerve will be encountered. Finger and thumb extension, rather than wrist extension due to possible direct stimulation of extensor carpi radialis, results in greatest block success. Incremental injections of local anesthetic (4–6 mL) are made with repeated aspiration.
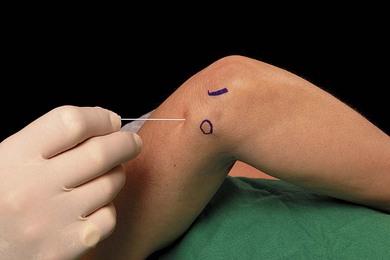
Ulnar nerve block
The elbow is flexed 90° and the arm internally rotated across the upper body for ulnar nerve block. Needle orientation is 45° to the skin in a cephalad direction (Fig. 21.11). The ulnar nerve is very superficial and contacted within 0.5–1 cm. Little finger flexion and ulnar deviation of the hand, rather than wrist flexion due to possible direct flexor carpi ulnaris stimulation, results in greatest block success. Incremental injections of local anesthetic (4 mL) are made with repeated aspiration. The needle is walked in a medial to lateral direction if the ulnar nerve is not stimulated. With elbow flexion, the ulnar nerve may slip over the medial epicondyle.
Ultrasound-guided approach
Intravenous access, electrocardiogram (ECG), pulse oximetry and blood pressure monitoring are established. Maximized comfort for the operator and patient is an important step in pre-procedure preparation. For ultrasound-guided nerve blocks at the elbow, the patient is placed in the supine position, the arm abducted, the forearm supinated, and the wrist halfway between pronation and supination. The operator sits adjacent to the side to be blocked. The ultrasound screen, transducer, needle, and plane of imaging should all be placed in one view for the operator. For ultrasound-guided nerve blocks at the elbow, the ultrasound screen is placed above the elbow on the side to be blocked (Fig. 21.12). Room lights may be turned down to enhance image viewing. The operating lights can be used to maintain some working lighting in the background.
Developing and maintaining a predetermined basic scanning routine is of enormous help in improving operator confidence and success. On the medial side of the antecubital fossa, the median nerve is identified on the medial side of the brachial artery. A 21-GA × 50-mm insulated needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 21.13). The operator can slide and tilt the transducer to maintain the needle tip within the plane of imaging as much as possible. The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the median nerve. Once the needle tip has been confirmed by ultrasonography to lie in close proximity to the median nerve, this can be confirmed by using a nerve stimulator. Characteristic motor activity in the hand is seen. Test injections for assessment of local anesthetic spread should be small (0.5–2 mL). If the local anesthetic spread is not seen on the ultrasound screen, the injection should be stopped. The needle is readjusted to allow complete encirclement of the nerve with local anesthetic (5 mL). Local anesthetic appears as a hypoechoic image (Fig 21.14).
On the lateral side of the antecubital fossa, the radial nerve is identified as deep and superficial branches between the brachioradialis and brachialis muscles. A 21-GA × 50-mm insulated needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 21.15). The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the radial nerve. The needle is readjusted to allow complete encirclement of the nerve with local anesthetic (5 mL). Local anesthetic appears as a hypoechoic image (Fig. 21.16).
The ulnar nerve is seen posterior to the medial epicondyle at the elbow level in the condylar groove (Fig. 21.8). A 21-GA × 50-mm insulated needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 21.17). The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the ulnar nerve. The needle is readjusted to allow complete encirclement of the nerve with local anesthetic (5 mL). Local anesthetic appears as a hypoechoic image (Fig. 21.18).
Adverse effects
Amoiridis G, Vlachonikolis IG. Verification of the median-to-ulnar and ulnar-to-median nerve motor fiber anastomosis in the forearm: an electrophysiological study. Clin Neurophysiol. 2003;114:94-98.
Loewy J. Sonoanatomy of the median, ulnar and radial nerves. Can Assoc Radiol J. 2002;53(1):33-38.
McCartney CJ, Xu D, Constantinescu C, et al. Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med. 2007;32(5):434-439.