CHAPTER 1 Elbow Arthroscopy: Positioning, Setup, Anatomy, and Portals
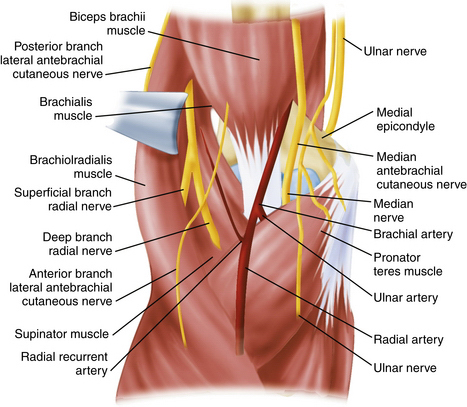
Elbow arthroscopy is a technically demanding procedure, and extensive hands-on training and supervised experience are needed to acquire proficiency. When performed with appropriate judgment and technique, elbow arthroscopy is an excellent tool for the correction of many lesions of the elbow joint with minimal risk.1 However, it poses greater technical challenges and neurologic risks than knee or shoulder arthroscopy. Arthroscopy of the elbow joint is perhaps the most hazardous in terms of its potential for causing injury to nearby nerves and vessels because of the complex relationship of these structures to the joint (Fig. 1-1).2 Because of the surrounding neurovascular structures, familiarity with the normal elbow anatomy and portals can decrease the risk of damage to important structures.3 Elbow arthroscopy provides an opportunity for diagnostic and therapeutic intervention with little morbidity.
Burman4 first described elbow arthroscopy in 1931, but he stated that the elbow is “… unsuitable for examination since the joint is so narrow for the relatively large needle.” In 1932, he revised his opinion based on the arthroscopic examination of 10 cadaveric elbows.5 After Burman’s studies were published, a small number of reports appeared in the German and Japanese literature, but it was not until the middle to late 1980s that reports began to appear in the American literature.6,7
In 1985, Andrews and Carson7 described the patient-supine technique and the use of various portals for elbow arthroscopy. In 1989, Poehling and colleagues8 described the patient-prone position for elbow arthroscopy. Since then, the techniques and indications for elbow arthroscopy have expanded, and there have been many more reports describing variations in operative technique.
ANATOMY
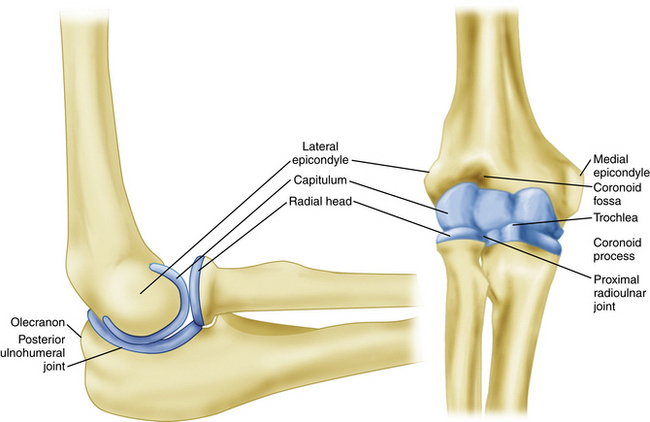
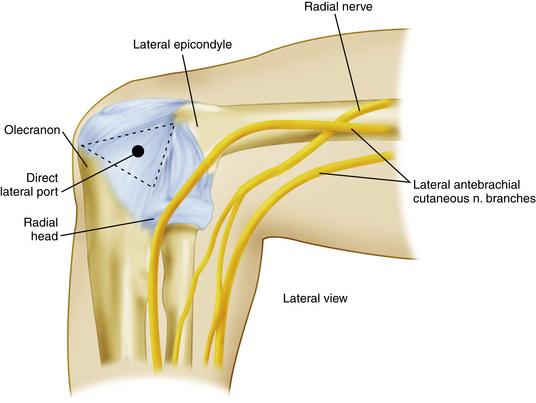
A clear understanding of the anatomy of the elbow is important before proceeding with arthroscopy. Important bony anatomic landmarks that should be palpated include the lateral and medial epicondyles, olecranon process, and radial head (Fig. 1-2). On the lateral side, the lateral epicondyle, olecranon process, and radial head form a triangle. Located in the center of this triangle is a soft spot called the anconeus triangle. It often is used to inflate the joint with fluid before introducing instruments or cannulas, and it can be the landmark for a direct lateral portal (Fig. 1-3). Posteriorly, important structures include the triceps muscle, tendon, and tip of the olecranon.
Sensory nerves around the elbow include the medial brachial cutaneous, the medial antebrachial cutaneous, the lateral antebrachial cutaneous, and the posterior antebrachial cutaneous nerves.9 The medial brachial cutaneous nerve penetrates the deep fascia midway down the arm on the medial side, and it supplies skin sensation to the posteromedial aspect of the arm to the level of the olecranon. The medial antebrachial cutaneous nerve supplies sensation to the medial side of the elbow and forearm. The lateral antebrachial cutaneous nerve is a branch of the musculocutaneous nerve, which exits between the biceps and brachialis muscles laterally to supply sensation to the elbow and lateral aspect of the forearm. The posterior antebrachial cutaneous nerve branches from the radial nerve and courses down the lateral aspect of the arm to supply sensation to the posterolateral elbow and posterior forearm.6
The main neurovascular structures about the elbow are the median nerve, radial nerve, ulnar nerve, and brachial artery.9 The radial nerve spirals around the posterior humeral shaft, penetrates the lateral intermuscular septum, and descends anteriorly to the lateral epicondyle between the brachioradialis and brachialis muscles. The radial nerve then branches to form the superficial radial nerve, which supplies sensation to the dorsoradial wrist and posterior surface of the radial three and one-half digits, and the posterior interosseous nerve, which provides motor branches to the wrists, thumb, and finger extensors. The ulnar nerve penetrates the medial intermuscular septum in the distal one third of the arm, courses posteriorly to the median epicondyle, and then descends distally between the flexor carpi ulnaris and flexor digitorum superficialis muscles. The brachial artery courses just medial to the biceps tendon in the antecubital fossa and then descends to the level of the radial head, where it bifurcates into the radial and ulnar arteries (see Fig. 1-1).6
PATIENT EVALUATION
History
The differential diagnosis for symptoms of the anterior elbow includes distal biceps tendon rupture, which can be partial or complete; anterior capsular strain; and brachioradialis muscle strain.10 Symptoms in the posterior compartment can reflect valgus extension overload syndrome, posterior impingement, osteochondral loose bodies, triceps tendonitis, triceps tendon avulsion, or olecranon bursitis.11 Deep, aching pain in the posterior region of the elbow may indicate an olecranon stress fracture.12
A careful neurovascular history is also important as ulnar nerve paresthesias can be the result of cubital tunnel syndrome, a subluxing ulnar nerve, or a traction injury from valgus instability.6
Throwing athletes are a unique patient population, and it is important to gather information about prior injury and any changes in the throwing mechanism or rehabilitation regimen.10 A patient whose symptoms are related to throwing and are located medially may have an injury to the medial collateral ligament. Throwing athletes who report lost velocity and control or an inability “to let the ball go” may have pain posterior on forced extension, which may signify posterior olecranon impingement caused by a medial collateral ligament injury. The typical patient is a baseball pitcher in his mid-20s who has posterior elbow pain during the acceleration and follow-through phases of pitching and complains of the inability to fully extend the elbow.6 Young throwing athletes (<18 years) with OCD lesions often report progressive lateral elbow pain during late acceleration and follow-through phases, with loss of extension and episodes of locking.11
Physical Examination
A careful physical examination of all three compartments of the elbow is critical to determine the correct diagnosis. Each compartment should be examined individually to fully evaluate the elbow. The physical examination starts with careful inspection of the skin and soft tissues to make sure there are no scars, swelling, ecchymosis, soft tissue masses, or bony abnormalities. The alignment of the elbow should be inspected, noticing any significant varus or valgus deformities. Range of motion of the elbow in flexion, extension, supination, and pronation should be observed and compared with the contralateral side. Those with posteromedial impingement or valgus extension overload may reveal a flexion contracture and pain over the posteromedial olecranon tip.6
The examiner should test for valgus instability with the elbow flexed to 30 degrees to relax the anterior capsule and free the olecranon from its bony articulation in the olecranon fossa. A valgus stress is then applied with the elbow in full supination. Discomfort along the medial aspect of the elbow can indicate ulnar collateral ligament injury. Valgus laxity, however, is often difficult to discern, particularly if there is tearing of the undersurface of the ulnar collateral ligament.13 Comparison with the contralateral elbow can help differentiate physiologic laxity from pathologic instability.14
The triceps muscle insertion and the posterolateral and posteromedial joint areas are palpated to assess for tenderness, bone spurs, and posterior impingement lesions. The so-called clunk test is performed to demonstrate posterior olecranon impingement.15 The upper arm is grasped and stabilized as the elbow is brought into full extension. Reproduction of pain at the posteromedial aspect of the joint suggests compression of the olecranon into the fossa and indicates valgus extension overload.
The lateral epicondyle and extensor origin are palpated to assess for lateral epicondylitis. The radiocapitellar joint is palpated while the forearm is pronated and supinated to elicit crepitus or catching, which can be caused by chondromalacial lesions or impingement from a lateral synovial fringe.16 The soft spot is also inspected to determine whether there is synovitis or an effusion in the elbow joint.6
Stability can be assessed with O’Driscoll’s posterolateral rotatory instability test.17 The test is best done under general anesthesia because of the patient’s apprehension while awake, which may give a false-negative result. However, it can be done with the patient awake with the extremity over the patient’s head and the shoulder in full external rotation. During the test, a valgus, supination, and axial compression load is applied to the elbow, which is flexed approximately 20 to 30 degrees. With the elbow in extension, subluxation or dislocation of the radius and of the proximal ulna creates a posterior prominence and sulcus sign. When the elbow is flexed, radiohumeral and ulnohumeral joints are visibly or palpably reduced.6 Details of this technique can be found in Chapter 11.
Diagnostic Imaging
Routine diagnostic radiographs include an anteroposterior view with the elbow in full extension and a lateral view with the joint in 90 degrees of flexion. An axial view can be obtained to outline the olecranon and its medial and lateral articulations. This is the best view for identifying and assessing a posteromedial osteophyte. When there is a history of trauma, an oblique view should be done, and careful attention should be paid to the radial head and the coronoid process for subtle fracture lines. Radiographs should be reviewed for more obvious anterior or posterior elbow dislocations, along with more subtle degenerative changes, osteophytes, and loose bodies. However, plain radiographs are not always able to demonstrate all loose bodies.18
A gravity stress test radiograph can be used to detect valgus laxity of the elbow.19 The patient is placed in a supine position, and the shoulder is abducted and brought to maximum external rotation so that the elbow is parallel to the floor. If there is an injury to the ligament or bony attachment, increased joint space can be seen on radiographs.6
Magnetic resonance imaging (MRI) and computed tomography (CT) arthrography (CTA) have are accurate in diagnosing a complete tear of the ulnar collateral ligament.13 However, in early studies, CTA was more sensitive in detecting a partial undersurface tear of the ulnar collateral ligament.20 This was described as a T-sign lesion by Timmerman and Andrews, who said that it represents “…dye leaking around the detachment of the deep portion of the ulnar collateral ligament from its bony insertion, but remaining within the intact superficial layer, ulnar collateral ligament, and capsule.”13
MRI is useful for evaluating osteochondral lesions in the radiocapitellar joint21,22 and for demonstrating early vascular changes that are not yet apparent on plain radiographs, and it can be used to assess the extent of the lesion and displacement of fragments.6 MRI is also helpful for evaluating the soft tissue structures of the elbow, including the tendinous insertions of the flexor and extensor musculature to help in diagnosing medial and lateral epicondylitis, the triceps insertion and associated musculature to evaluate for triceps tendonitis, and the medial and lateral collateral ligaments for possible tears. However, MRI may not demonstrate subtle undersurface tears of the ulnar collateral ligament. Magnetic resonance arthrography with saline contrast or gadolinium can increase the sensitivity for detecting undersurface tears of the ulnar collateral ligament and has become the test of choice to detect these tears.13
TREATMENT
Indications and Contraindications
In 1992, O’Driscoll and Morrey described the early indication for elbow arthroscopy, which was pain or symptoms that were substantial enough to interfere with work, daily activities, sports, or sleep and that did not resolve after conservative treatment.23 In this early study, they analyzed the results of 71 elbow arthroscopies as the indications for such a procedure were evolving. Not surprising, the best early results were seen for arthroscopic removal of loose bodies, assessment of undiagnosed snapping, idiopathic flexion contractures, local débridement of damaged articular surfaces, and synovectomy. They found that the patients least likely to benefit were the ones in whom there was a disparity between objective and subjective findings.23
Since then, the indications for elbow arthroscopy have evolved. In 1994, Poehling further refined the indications, which included its use for the diagnosis of intra-articular lesions of the elbow, the removal of loose and foreign bodies, irrigation of the joint, débridement of an infected joint, excision of osteophytes, synovectomy, capsular release, excision of the radial head, and treatment of acute fractures of the elbow.1
Several investigators have since reported the usefulness of elbow arthroscopy for the removal of loose bodies,6,7,18,23-25 and this continues to be the primary indication for elbow arthroscopy. Several pathologic processes may initiate the formation of a loose body, including trauma and synovial chondromatosis. Regardless of the cause, the patients usually present with swelling, locking, pain, and loss of motion, all of which can be improved with the removal of loose bodies. These loose bodies can be found in the anterior and posterior compartments and in the posterior medial gutter, and removing them can be a technically demanding procedure. Further details and helpful hints can be found in Chapter 2.
Elbow arthroscopy can be an effective tool if the diagnosis of an infection is made or suspected. It is a less invasive way to enter into the joint with minimal trauma to confirm the diagnosis of an infection, irrigate the joint, débride infected tissue, and assess the condition of the underlying bone, cartilage, and synovial tissue.1
The presence of osteophytes, or osseous spurs, is another condition that lends itself to arthroscopic management and removal.23–26 A true lateral radiograph of the elbow is useful for the identification of osteophytes that may limit full extension of the elbow with impingement of the posterior olecranon spur in the olecranon fossa.1,23 An axial view may also show a posteromedial osteophyte,6 which can be easily removed arthroscopically.
The term valgus extension overload was coined27 to describe the findings that can be identified in baseball pitchers and other overhead athletes. The tremendous repetitive valgus forces generated during the acceleration and follow-through phases of pitching, as the elbow goes into extension, can result in osteochondral changes in the olecranon and distal humerus. A significant osteophyte forms on the posteromedial aspect of the olecranon fossa with continued pitching or overhead activities, creating an area of chondromalacia.6 The use of elbow arthroscopy in the throwing athlete, including evaluation of the medial collateral ligament, is addressed in Chapter 12. The inability to reliably visualize the anterior bundle of the medial collateral ligament with the arthroscope limits the value of the arthroscope when assessing medial collateral ligament injuries.28,29 The management of posterolateral instability is discussed in Chapter 11.
Chronic synovitis caused by inflammatory arthritis that does not respond to nonoperative management and when there is minimal joint destruction can be an indication for elbow arthroscopy. Synovectomy can provide considerable relief of pain.23,30,31 Diagnostic elbow arthroscopy can also be used for synovial biopsy to establish the diagnosis of rheumatoid arthritis or other inflammatory arthritides or a monoarticular or polyarticular arthritis of unknown origin.23 The elbow joint is affected in approximately 20% to 50% of patients with rheumatoid arthritis, and 50% of these patients develop pain and associated loss of motion.23,32 Lee and Morrey achieved a 93% rate of good or excellent results in a short-term follow-up assessment of 14 arthroscopic synovectomies in 11 patients. However, only 57% of their patients maintained good or excellent results at an average of 42 months after surgery.31 When performing elbow arthroscopy and synovectomy for rheumatoid arthritis and other inflammatory arthritides, it is important to set realistic expectations for the patient because the symptoms can recur.
OCD of the capitellum is characterized by pain, swelling, and limitation of motion, and it usually occurs during adolescence or young adulthood in a throwing athlete or gymnast.33 The underlying cause of this lesion is most likely repetitive microtrauma to a vulnerable epiphysis with a precarious blood supply.33 The lesion may progress to joint incongruity, loose body formation, and a locked elbow with chronic pain, all of which are indications for elbow arthroscopy when conservative measures fail. The procedure involves the arthroscopic removal of osteophytes, excision of loose or detached cartilage, and curettement and drilling of the base of the lesion.34
Panner’s disease is an osteochondrosis of the entire capitellum in children and adolescents, and it may represent an early stage of OCD.6 Reconstitution of the capitellum usually occurs with rest and without late sequelae or limitations.33 More information about OCD can be found in Chapter 7.
The indications for arthroscopic débridement of the elbow for degenerative osteoarthritis are similar to those described for loose body removal, valgus extension overload, and OCD. Pain associated with swelling and mechanical symptoms of catching and locking respond well to arthroscopic débridement.24–26 Removal of loose bodies and osteophytes from the olecranon, olecranon fossa, and coronoid process can reduce pain, increase range of motion, and eliminate mechanical-like symptoms.24–26 Elbow arthroscopy has limited value in primary degenerative arthrosis when there are no significant osteophytes, loose bodies, or mechanical-like symptoms. The arthritic elbow is addressed in Chapter 9.
Arthrofibrosis of the elbow treated arthroscopically can be a technically demanding procedure with an increased risk of complications because of the limited ability to distend the arthrofibrotic capsule and the proximity of many neurovascular structures.1,6,24 Loss of elbow joint motion can be a result of bone or soft tissue problems caused by trauma and degenerative or inflammatory arthritides. Patients can have a loss of flexion or extension, or both. It is important to attempt to determine the cause of the contracture because this can influence treatment.6 If a nonoperative treatment of nonsteroidal anti-inflammatory drugs (NSAIDs), stretching exercises, splinting, and other modalities fail, arthroscopic release and thorough joint débridement may be indicated in properly selected patients.24,35,36 The details of this technically demanding procedure can be found in Chapter 8.
The indications for elbow arthroscopy have been extended to include the treatment of lateral epicondylitis. When conservative measures fail, arthroscopic release offers several potential advantages over open techniques.6 It preserves the common extensor origin by addressing the lesion directly,37 and it allows for intra-articular examination for possible chondral lesions, loose bodies, and other disorders, such as an inflamed lateral synovial fringe. It also permits a shorter postoperative rehabilitation period and an earlier return to work or sports.6 The details of the technique of the treatment of arthroscopic lateral epicondyle release can be found in Chapter 3.
Radial head excision can be performed arthroscopically for post-traumatic arthritis of the radiocapitellar joint caused by a radial head fracture.1,6,24,38 Advantages of arthroscopic treatment include more complete visualization of the articular surface of the elbow and associated chondral lesions or ligamentous disruptions.6 In addition to the entire radial head, as much as 2 or 3 mm of the radial neck can be removed. To maintain stability at the proximal radioulnar joint, the annular ligament must be left intact.1 More information about this technique can be found in Chapter 10.
The arthroscopic management of selected fractures around the elbow with percutaneous pins and screws is evolving and includes the treatment of radial head fractures, capitellum fractures, and coronoid fractures. The arthroscopic-assisted treatment of coronoid fractures has shown promise in a small study group of 7 patients.39 More information about the arthroscopic treatment of fractures of the elbow can be found in Chapter 15. New frontiers of elbow arthroscopy include the treatment of olecranon bursitis (Chapter 5), endoscopic repair of a torn distal biceps tendon (Chapter 13), arthroscopic triceps repair (Chapter 14), and arthroscopic ulnar nerve release (Chapter 16).
The primary contraindication to elbow arthroscopy is any significant distortion of normal bony or soft tissue anatomy that precludes safe entry of the arthroscope into the joint.23,9 For example, a previous ulnar nerve transposition that was submuscular or subcutaneous would interfere with safe proximal, anteromedial portal placement and is a relative contraindication for safe introduction of the arthroscope through the medial side of the elbow.6,40 In these cases, identification of the ulnar nerve is necessary before establishing a medial portal.40
Another relative contraindication is a severely ankylosed joint that may distort normal anatomy and place important neurovascular structures at risk. This may not allow for adequate joint distention and may not allow proper displacement of neurovascular structures away from portal sites and within the joint from instrumentation.6 Localized infection in the area of portal placement is also a contraindication to elbow arthroscopy.
Elbow Arthroscopy
Anesthesia
Most surgeons prefer to use general endotracheal anesthesia for patients undergoing elbow arthroscopy because it provides total muscle relaxation and is more comfortable for the patient.6,40 The use of regional anesthesia is advocated by some, including the use of an axillary nerve block or an interscalene nerve block. These blocks can be administered safely and successfully by a trained anesthesiologist, but there is still inherent risk in these blocks not seen with general anesthesia.
There is apprehension among some surgeons about using local and intravenous blocks because the patient’s postoperative neurologic status cannot be assessed and may be compromised by an extended axillary or interscalene nerve block.6 If there is a neurologic deficit found after the procedure, it may be difficult to determine how it occurred, and there may be finger pointing between the anesthesiologist and the surgeon.
Positioning
Traditionally, elbow arthroscopy was performed with the patient resting supine on the operating table,7 until use of the prone position was introduced in 1989 by Poehling.8 The prone position improves the mobility of the arthroscope within the joint, facilitates manipulation of the joint, provides for a more complete intra-articular inspection (especially in the posterior aspect of the joint), and eliminates the need for an overhead suspension device to support the elbow. The main disadvantage to this position is a more difficult access to the patient’s airway.1
After an appropriate level of anesthesia (i.e., general endotracheal or axillary block) has been achieved, the patient is placed prone, with large chest rolls under the torso. The chest rolls must bee large enough to raise the patient’s torso up from the operating table. If these rolls are not large enough, it makes it difficult to position the arm and elbow to access the proximal anteromedial portal. An arm board is placed on the operative side of the table and parallel to it. To increase the mobility of the upper extremity intraoperatively, a sandbag, block, or firm bump of towels is placed under the shoulder to further elevate the arm away from the table. The forearm is then allowed to hang in a dependent position over the arm board at 90 degrees (Fig. 1-4). A sterile tourniquet may be placed around the proximal aspect of the arm to help to control bleeding during the procedure, but it is not always necessary to inflate when using a mechanical irrigation system.1 After the extremity is prepared and draped, a large sterile bump is placed under the arm proximal to the elbow to keep the shoulder abducted to 90 degrees and to keep the elbow at approximately 90 degrees of flexion (Fig. 1-5).
Some surgeons prefer the lateral decubitus position because they feel it provides improved stability of the extremity, is more convenient for the anesthesiologist, and allows posterior elbow joint access without compromising airway access.23,40 O’Driscoll and Morrey prefer the lateral decubitus position because it has the advantages of the prone positioning without compromising the anesthesiologist’s access to the airway.23 The patient is placed in the lateral decubitus position with the involved extremity facing upward. The arm is then supported on a well-padded bolster, with the forearm hanging free and the elbow flexed to 90 degrees. In this position, the elbow is supported in front of the surgeon, who then has access to the various portal sites.
Whether using the prone or lateral decubitus position, the forearm is prepared from the proximal arm to the tip of the fingers, and the extremity is wrapped with an elastic bandage from the fingers to just below the elbow to minimize fluid extravasation into the forearm.40
Operating Room Setup
When using the prone position, anesthesia is positioned at the head of the table, the surgeon stands directly lateral to the flexed elbow, and the assistant stands toward the head of the patient. The ancillary scrub personnel stand toward the foot of the patient or behind the surgeon and the assistant. One Mayo stand is placed behind the surgeon, and the other Mayo stand is on the opposite side of the table. All tubing and electrical cords run from this Mayo stand to the video monitor, recorder, light source, camera, fluid bags, and mechanical irrigation system, which are placed on the opposite side of the patient (see Fig. 1-5).
Instrumentation
A standard 4.0-mm, 30-degree arthroscope enables excellent visualization of the elbow joint. A smaller, 2.7-mm arthroscope usually is unnecessary but can be useful for viewing small spaces, such as the lateral compartment from the direct lateral portal and for arthroscopy in adolescent patients.6,40 The use of cannulas allows the surgeon to switch viewing and working portals without repeated joint capsule injuries. This also minimizes the risk of injury to neurovascular structures and decreases the chance of fluid extravasation into the soft tissues, swelling, and possible compartment syndrome.6 A metal cannula typically is used for the arthroscope, and the working portal is usually a disposable plastic cannula with a diaphragm that allows instruments to be introduced without loss of joint distention.
Side-vented inflow cannulas should be avoided in elbow arthroscopy because the distance between the skin ad the joint capsule is often very slight. With side-vented cannulas, the cannula can be intra-articular while the side vents remain extra-articular, resulting in fluid extravasation into the surrounding soft tissues. Inflow cannulas should be devoid of side vents, with fluid flow occurring directly at the end of the cannula.41
All trocars should be conical and blunt tipped to decrease the possibility of neurovascular and articular cartilage injury. A variety of handheld instruments, such as probes, grasping forceps, and punches, and motorized instruments, such as synovial resectors and burrs, are used during elbow arthroscopy.6,40
If a mechanical pump is used, an inflow pressure of 35 mm Hg is usually used to maintain joint distention.6 Some surgeons prefer the use of gravity inflow and think it gives adequate joint distention without the risk of fluid extravasation. If a tourniquet is used, it can be set at 250 mm Hg and inflated if needed.
General Surgical Technique
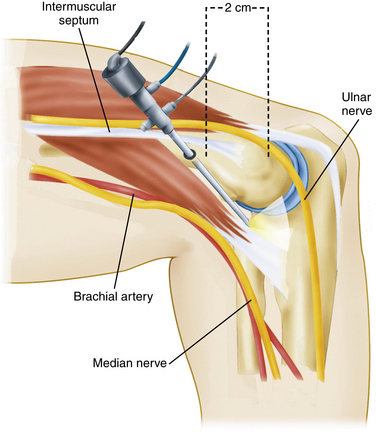
Elbow arthroscopy has a significant potential for complications, particularly neurovascular injury.6 The key to avoiding complications is to have a clear understanding of the relationship of the neurovascular structures to the soft tissue and bony anatomy. With the patient positioned in the lateral decubitus or prone position, it is important to identify and mark landmarks. They include the tip of the olecranon, the medial and lateral epicondyles, the radial head, the soft spot of the elbow, the medial intermuscular septum, and the ulnar nerve (Fig. 1-6). Some surgeons recommend distending the joint with 20 to 40 mL of fluid through the lateral soft spot before establishing the initial portal.42 Cadaveric studies have demonstrated that joint insufflation significantly increases the distance between the joint surfaces and neurovascular structures, helping to protect them from injury during joint entry.43
In a different cadaveric study looking at the role of joint insufflation before portal placement, Miller and coworkers.44 demonstrated that there was a small distance (as narrow as 6 mm) between the joint capsule and neurovascular structures and that joint insufflation did not increase the capsule-to-nerve distance. My colleagues and I have found joint insufflation unnecessary before making the proximal anteromedial portal, the first portal that we typically establish. If the surgeon pays close attention to anatomic landmarks, the elbow joint can be safely entered into without having to inflate the joint with fluid.
When creating portals, the surgeon should avoid penetrating the subcutaneous tissue, thereby helping to prevent injury to the superficial cutaneous nerves. A hemostat or mosquito clamp should be used to spread tissues down to the capsule.6 When the arthroscope is introduced, the elbow should be flexed to 90 degrees to relax and protect the anterior neurovascular structures,43 and only blunt trocars should be used.
Whether the anteromedial or anterolateral portal should be created first has been an issue of some debate. Many surgeons create a lateral portal initially and then establish a medial portal with a spinal needle by direct visualization from within the joint. Alternatively, an inside-out technique may be employed in which a switching stick is used to establish the medial portal from inside the joint.45 Other surgeons, using the same techniques, establish the medial portal first, and cadaveric studies have found that it is safer to establish the proximal anteromedial portal first than the lateral portal.46
Other surgeons and I think the proximal anteromedial portal should be created first, because it is the safest approach as long as the surgeon has identified and outlined the important soft tissue and bony landmarks, including the intermuscular septum.6,40,45,46 There is less fluid extravasation when starting medially, because a superomedial portal traverses predominately tendinous tissue and a tough portion of the forearm flexor muscles.9,38 The thicker tissues minimize fluid extravasation more effectively than the softer, thinner radial capsule.9,38 Most elbow disorders are located in the lateral compartment, which is best visualized from the proximal anteromedial portal.6
Portal Placement
Anterior Compartment.
The proximal anteromedial portal is established first, and it was first described by Poehling.8 It is located approximately 2 cm proximal to the medial epicondyle and just anterior to the intermuscular septum (Fig. 1-7). Before establishing this portal, the location and the stability of the ulnar nerve should be assessed. The prevalence rate of ulnar nerve subluxation anterior to the cubital tunnel is approximately 17%. Blunt dissection is carried out until the anterior aspect of the humerus is palpated while staying anterior to the intermuscular septum. The arthroscopic sheath is then inserted anterior to the intermuscular septum while maintaining contact with the anterior aspect of the humerus and directing the trocar toward the radial head. Use of the anterior surface of the humerus as a constant guide helps to prevent injury to the median nerve and the brachial artery, which are anterior to the capsule. The ulnar nerve is located approximately 3 to 4 mm from this portal and posterior to the intermuscular septum (Fig. 1-8). Palpating the septum and making sure that the portal is established anterior to the septum minimizes the risk of injury to the nerve while providing excellent visualization. This portal provides excellent visualization of the anterior compartment of the elbow, particularly the radiocapitellar joint, the humeroulnar joints, the coronoid fossa, and superior joint capsule.1,6
The anteromedial portal as described by Lynch and associates47 is located 2 cm distal and 2 cm anterior to the medial epicondyle, and it is at or near the distal extent of the elbow capsule. Because of the location of this portal, the cannula can enter the joint only by being advanced straight laterally, toward the median nerve.46 Because of this, the proximal anteromedial portal is recommended; it is safer because the more proximal position allows the arthroscope to be directed distally, resulting in the arthroscope being almost parallel to the median nerve in the anteroposterior plane.6,46
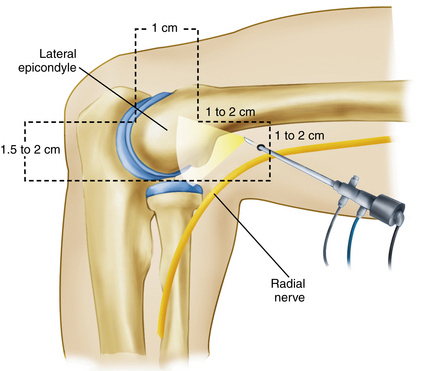
The anterolateral portal was originally described by Carson and Andrews as being located 3 cm distal and 2 cm anterior to the lateral epicondyle.7 However, this portal location places the radial nerve at significant risk for iatrogenic injury.47 Lindenfeld demonstrated the radial nerve could be as close as 3 mm to this portal.46 To decrease risk of injury to the radial nerve, several investigators have stressed the importance of avoiding the distal placement of this portal in favor of a more proximal placement of the anterolateral portal.2,42 Field and colleaues42 compared three lateral portals: a proximal anterolateral portal (located 2 cm proximal and 1 cm anterior to the lateral epicondyle), a distal anterolateral portal (as described by Carson and Andrews), and a middle anterolateral portal (located 1 cm directly anterior to the lateral epicondyle). The investigators found that the proximal anterolateral portal was the safest and that the radiohumeral joint visualization was most complete and technically easiest using this most proximal portal.
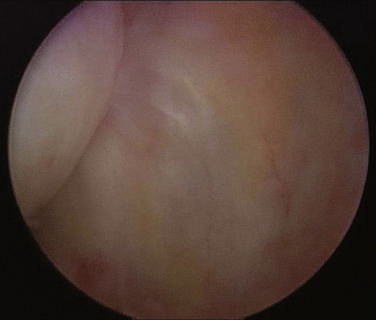
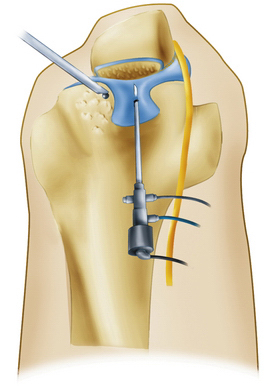
After creating the proximal anteromedial portal and using it as viewing portal, we think creating this proximal anterolateral portal is done best using an outside-in technique and localizing the position with a spinal needle. This portal is created 2 cm proximal and 1 cm anterior to the lateral epicondyle, as described by Field and coworkers.42 The exact entry depends on the pathology to be addressed. From the proximal anteromedial portal, the lateral capsule is visualized, and palpation of the skin helps to localize the exact location of the spinal needle to aid in portal placement (Fig. 1-9). It is important to direct the cannula toward the humerus while penetrating the capsule so that the portal placement is not too far anterior and medial.3 From the proximal anteromedial portal, the radiocapitellar joint is easily visualized (Fig. 1-10). The trochlea and the coronoid process can be seen from the proximal anteromedial portal (Fig. 1-11).
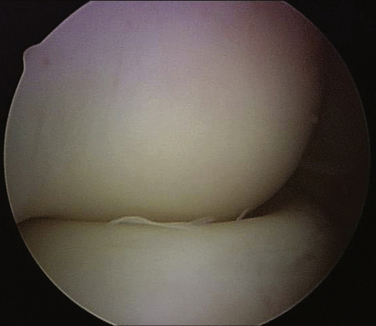
FIGURE 1-10 Viewing from the proximal anteromedial portal, the radial head and the capitellum are easily visualized.
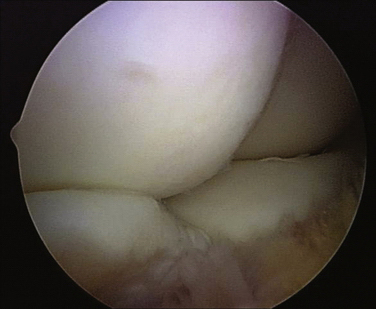
The proximal anterolateral portal is often a working portal and is ideal for arthroscopic lateral epicondyle release and for débridement of the radiocapitellar joint. Viewing from this portal permits visualization of the anterior compartment (Fig. 1-12) and is particularly good for evaluating medial structures, such as the trochlea, coronoid tip, and the medial capsule (Fig. 1-13).
Posterior Compartment.
The straight posterior portal is located 3 cm proximal to the tip of the olecranon and can be used as a viewing portal or as a working portal. When it is the first portal created, a cannula with a blunt trocar is inserted. The cannula pierces the triceps muscle just above the musculotendinous junction and is bluntly maneuvered in a circular motion, manipulating the soft tissues from the olecranon fossa for better visualization. When used as a working portal, it is helpful for removal of impinging olecranon osteophytes and loose bodies from the posterior elbow joint.45 It is also needed for a complete synovectomy of the elbow.6 The straight posterior portal passes within 25 mm of the ulnar nerve and within 23 mm of the posterior antebrachial cutaneous nerve.9
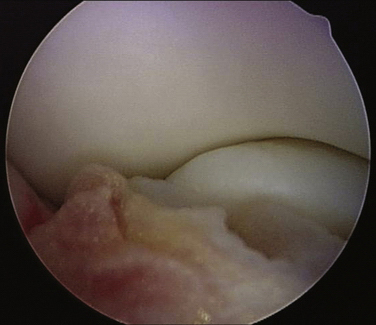
The posterolateral portal is located 2 to 3 cm proximal to the tip of olecranon at the lateral border of the triceps tendon. This is created while visualizing from the straight posterior portal and using a spinal needle directed toward the olecranon fossa (Fig. 1-14). Initial visualization is often difficult due to scar, fat pad hypertrophy, and synovitis. A trocar is then directed toward the olecranon fossa, passing through the triceps muscle to reach the capsule. A shaver is introduced to improve visualization of the posterior compartment. This portal permits visualization of the olecranon tip, olecranon fossa, and the posterior trochlea, and it can be used as a working portal to remove osteophytes and loose bodies from the posterior compartment (Fig. 1-15). However, the posterior capitellum is not seen well from this portal.6 The medial and posterior antebrachial cutaneous nerves are the two neurovascular structures at most risk; they are an average of 25 mm from this portal.47 The ulnar nerve is approximately 25 mm from this portal, but as long as the cannula is kept lateral to the posterior midline, the nerve is not at risk for injury.9
The posterolateral anatomy of the elbow allows for portal placement anywhere from the proximal posterolateral portal to the lateral soft spot. Altering the portal position along the line between the posterolateral portal and lateral soft spot changes the orientation of the portal relative to the joint.40 These portals are particularly useful for gaining access to the posterolateral recess.
The direct lateral portal is located at the soft spot, which is the triangle formed by the radial head, lateral epicondyle, and olecranon. It is developed under direct visualization using a spinal needle. It is useful as a viewing portal for working in the posterior compartment and viewing the radiocapitellar joint and as a working portal for radial head resection.24 This is the only portal that provides easy access to the posterior capitellum and radioulnar joint, and it can be useful for lesions of the radiocapitellar joint.6
COMPLICATIONS
Complications due to elbow arthroscopy can be minimized if the surgeon has a sound knowledge of the anatomy of the elbow and uses proper equipment and meticulous operative technique.1 One of the most common complications is neurologic injury,1,47,48 including transient nerve palsies involving the radial nerve, posterior interosseous nerve, and ulnar nerve. Injury can be caused by direct laceration of a nerve by a knife penetrating deeply beneath the skin or from the cannula trocar.10 Compression from a cannula, from fluid extravasation, or from the use of local anesthetics has caused neurologic injuries23 but was usually transient. Transection of the posterior interosseous nerve, median nerve, ulnar nerve, and radial nerve has been reported. In a 1986 review of 569 elbow arthroscopic procedures performed by members of the Arthroscopy Association of North America (AANA), only one neurovascular complication, a radial nerve injury, was reported.49 In a 2001 report of 473 elbow arthroscopies performed by experienced arthroscopists, four types of minor complications, including infection, nerve injury, prolonged drainage, and contracture, were identified in 50 cases. The most common complication was persistent portal drainage,48 especially from the lateral portal. There is little subcutaneous tissue separating the skin from the capsule. Portal drainage can be reduced by using a side box stay suture, which closes the portal securely and minimizes drainage.
Many of the complications associated with elbow arthroscopy are the result of inexperience, poor technique, and lack of knowledge regarding elbow anatomy. The surgeon who wishes to perform elbow arthroscopy safely and effectively must adhere to strict surgical technique and portal placement to avoid preventable complications.10
PEARLS& PITFALLS
PEARLS
PITFALLS
CONCLUSIONS
Arthroscopic surgery of the elbow is a technically demanding procedure. Attention to detail, including careful portal placement, is necessary to avoid iatrogenic injury to neurovascular structures around the elbow joint. In every clinical case, the bony anatomy should be drawn on the patient’s elbow, and an 18-gauge spinal needle should be used to confirm the correct portal location before introducing larger arthroscopic instruments.10
With innovations in techniques and technology, it is possible to treat a variety of lesions of the elbow. As with any operative procedure, careful preoperative planning, including a detailed history, physical examination, and proper imaging studies, must be combined with sound clinical judgment to ensure a successful procedure.
1. Poehling GG, Ekman EF. Arthroscopy of the Elbow. J Bone Joint Surg Am. 1994;76A:1265-1271.
2. Strothers D, Day B, Regan WR. Arthroscopy of the elbow: anatomy, portal sites, and description of the proximal lateral portal. Arthroscopy. 1995;11:449-457.
3. Moskal MJ. Advanced arthroscopic management of common elbow disorders. Vancouver, Canada: Presented at the Arthroscopy Association of North America 24th Annual Meeting; May 2005.
4. Burman MS. Arthroscopy or the direct visualization of the joints: an experimental cadaveric study. J Bone Joint Surg. 1931;13:669-695.
5. Burman MS. Arthroscopy of the elbow joint. A cadaver study. J Bone Joint Surg. 1932;14:349-350.
6. Baker CL, Grant LJ. Arthroscopy of the elbow. Am J Sports Med. 1999;27:251-264.
7. Andrews JR, Carson WG. Arthroscopy of the elbow. Arthroscopy. 1985;1:97-107.
8. Poehling GG, Whipple TL, Sisco L, Goldman B. Elbow arthroscopy: a new technique. Arthroscopy. 1989;5:220-224.
9. Baker CL, Brooks AA. Arthroscopy of the elbow. Clin Sports Med. 1996;15:261-281.
10. Dodson CC, Nho SJ, Williams RJ, Altchek DW. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16:574-585.
11. Yadao MA, Field LD, Savoie FHIII. Osteochondritis dissecans of the elbow. Instr Course Lect. 2004;53:599-606.
12. Cain EL, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621-635.
13. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26-32.
14. Jobe FW. Operative Techniques in Upper Extremity Sports Injuries. St. Louis, MO: Mosby–Year Book; 1996.
15. Baker CL. The Elbow. In: Whipple TL, editor. Arthroscopic Surgery: The Shoulder and Elbow. Philadelphia, PA: JB Lippincott; 1993:239-300.
16. Clarke RP. Symptomatic, lateral synovial fringe (plica) of the elbow joint. Arthroscopy. 1988;4:112-116.
17. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73A:440-446.
18. Oglivie-Harris DJ, Schemitsch E. Arthroscopy of the elbow for removal of loose bodies. Arthroscopy. 1993;9:5-8.
19. Bennett JB, Hulles HS. Ligamentous and articular cartilage injuries in the athlete. In: Money BF, editor. The Elbow and its Disorders. Philadelphia, PA: WB Saunders; 1985:502-522.
20. Timmerman LA, Andrews JR. Undersurface tear of the ulnar collateral ligament in baseball players. A newly recognized lesion. Am J Sports Med. 1964;22:33-36.
21. Jaraw PM, Hessen U, Hirsch G. Osteochondral lesion in the radiocapitellar joint in the skeletally immature: radiographic MRI and arthroscopic findings in 13 conservative cases. J Pediatr Orthop. 1997;17:311-314.
22. Takahara M, Shundo M, Kondo M, et al. Early Detection of Osteochondritis dissecans of the capitellum in young baseball players: report of three cases. J Bone Joint Surg Am. 1998;80A:892-897.
23. O’Driscoll SW, Morrey BF. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74A:84-94.
24. Savoie FH, Nunley PD, Field LD. Arthroscopic management of the arthritic elbow: indications, technique and results. J Shoulder Elbow Surg. 1999;8:214-219.
25. Thal R. Osteoarthritis. In: Savoie FH, Field LD, editors. Elbow Arthroscopy. New York, NY: Churchill Livingstone, 1996.
26. Steinmann SP, King GJ, Savoie FH. Arthroscopic treatment of the arthritic elbow. J Bone Joint Surg Am. 2005;87A:2114-2121.
27. Wilson FD, Andrews JR, Blackburn TA, et al. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83-88.
28. Field LD, Callaway GH, O’Brien SJ, et al. Arthroscopic assessment of the medial collateral ligament complex of the elbow. Am J Sports Med. 1995;23:396-400.
29. Field LD, Altchek DW. Evaluation of the arthroscopic valgus instability test of the elbow. Am J Sports Med. 1996;24:177-181.
30. Angelo RL. Advances in elbow arthroscopy. Orthopedics. 1993;16:1037-1046.
31. Lee BPH, Morrey BF. Arthroscopic synovectomy of the elbow for rheumatoid arthritis: a prospective study. J Bone Joint Surg Br. 1997;79B:770-772.
32. Nestor BJ. Surgical treatment of the rheumatoid elbow: an overview. Rheum Dis Clin J North Am. 1998;24:83-99.
33. Schenck RCJr, Goodnight JM. Osteochondritis dissecans. J Bone Joint Surg Am. 1996;78:439-456.
34. Ruch DS, Poehling GG. Arthroscopic treatment of Panner’s disease. Clin Sports Med. 1991;10:629-636.
35. Timmerman LA, Andrews JR. Arthroscopic treatment of posttraumatic elbow pain and stiffness. Am J Sports Med. 1994;22:230-235.
36. Phillips BB, Strasburger S. Arthroscopic treatment of arthrofibrosis of the elbow joint. Arthroscopy. 1998;14:38-44.
37. Baker CL, Cummings PD. Arthroscopic management of miscellaneous elbow disorders. Oper Tech Sports Med. 1998;6:121-129.
38. McLaughlin RE, Savoie FH, Field LF, Ramsey JR. Arthroscopic treatment of the arthritic elbow due to primary radiocapitellar arthritis. Arthroscopy. 2006;22:63-69.
39. Adams JE, Merten SM, Steinmann SP. Arthroscopic assisted treatment of coracoid fractures. Arthroscopy. 2007;23:1060-1065.
40. Abboud JA, Ricchette ET, Tjoumakaris F, Ramsey ML. Elbow arthroscopy: basic set-up and portal placement. J Am Acad Orthop Surg. 2006;14:312-318.
41. Ramsey ML, Naranja RJ. Diagnostic arthroscopy of the elbow. In: Baker CLJr, Plancher DL, editors. Operative Treatment of Elbow Injuries. New York, NY: Springer-Verlag; 2002:162-169.
42. Field LD, Altchek DW, Warren RF, et al. Arthroscopy anatomy of the lateral elbow: a comparison of 3 portals. Arthroscopy. 1994;10:602-607.
43. Adolfsson L. Arthroscopy of the elbow joint: a cadaveric study of portal placement. J Shoulder Elbow Surg. 1994;3:53-61.
44. Miller CD, Jobe CM, Wright MH. Neuroanatomy in elbow arthroscopy. J Shoulder Elbow Surg. 1995;4:168-174.
45. Andrews JR, St Pierre RK, Carson WG. Arthroscopy of the elbow. Clin Sports Med. 1986;5:653-662.
46. Lindenfeld TN. Medial approach in elbow arthroscopy. Am J Sports Med. 1990;18:413-417.
47. Lynch GJ, Meyers JF, Whipple TL, Caspari RB. Neurovascular anatomy and elbow arthroscopy: inherent risks. Arthroscopy. 1986;2:190-197.
48. Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. J Bone Joint Surg Am. 2001;83:25-34.
49. Small NC. Complications in arthroscopy: the knee and other joints. Arthroscopy. 1986;2:253-258.