Chapter 19 Effects of nasal surgery on snoring and sleep apnea
1 INTRODUCTION: NASAL SURGERY AND OBSTRUCTIVE SLEEP APNEA
The location of obstruction in the obstructive sleep apnea/hypopnea syndrome (OSAHS) is variable and can often be localized to several levels in the upper airway. In fact, the level of obstruction can vary in the same patient among consecutive episodes of apnea.1 In normal circumstances, the normal nose contributes to 50% of upper airway resistance, adding to the resistance provided by both oropharyngeal tissues and the tongue.2 In fact, resistance at the level of the nose is more constant in both sleep and awake states, due to the more rigid frame provided by the septum and the lower and upper lateral cartilages. If, however, the upper or lower lateral cartilages are weak, damaged, resected, or otherwise structurally affected, this stability is lost. Patients in such cases are subject to an increased tendency towards collapse during sleep, even with a normal nasal airway in the awake state. The association between nasal obstruction and sleep disturbances was probably what first led to the description of sleep-related breathing disorders,3 or sleep-disordered breathing (SDB), the group of disorders that includes snoring, the upper airway resistance syndrome, and OSAHS. It is currently recognized that nasal obstruction interferes with pressure titration in nasal continuous positive airway pressure (nCPAP) for the management of OSAHS, and that treatment of such obstruction improves patient compliance with nCPAP.4,5 The cause–effect relationship of nasal obstruction and OSAHS, however, remains unclear. While surgical correction of obstructed nasal airways is, without a doubt, an important component of the surgical management of OSAHS,6–8 the expectations of improvement after performing nasal procedures alone are still, at best, unclear. Another important factor in the relationship between nasal obstruction and SDB is the tendency that patients with obstructed nasal airways have to mouth breathe, which decreases the hypopharyngeal space by moving the mandible posteriorly and, most importantly, by pushing the base of the tongue backwards.
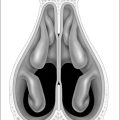
The primary sites of nasal obstruction are the nasal vestibule, the nasal valves, and the turbinates.9 The nasal septum, when deviated, also has a significant impact on these areas of obstruction. Of these three sites, the nasal valve is the site of major resistance.2 Many authors have shown that, in fact, nasal valve incompetence may equal, or even exceed, septal deviation or turbinate hypertrophy as the prime cause of nasal airway obstruction.10 The internal nasal valve is defined as the area between the caudal end of the upper lateral cartilages and the cartilaginous septum, and the entire nasal valve complex is bounded superiorly by the reflection between the upper lateral cartilages and the septum, posteriorly by the head of the inferior turbinate, inferiorly by the floor of the nose, and laterally by the bony piriform aperture.11 During inspiration, particularly during the forced inspiration that occurs during an apneic episode, the negative nasopharyngeal and intranasal pressures increase to generate more flow, creating a transmural pressure gradient, which, when a critical value is reached, causes collapse of the upper lateral cartilages.12 Thus, the flow-limiting segment constituted by the nasal site of obstruction acts as a Starling resistor, not only at the level of the nose (in the case of inspiratory nasal valve collapse), but also for further ‘downstream’ structures like the soft palate and the oro- and hypopharynx.7,13 Nasal obstruction leads to mouth opening and transition to oral breathing, which contributes to airway flow limitation and collapse, mainly due to inferior movement of the mandible,14 a backward fall of the base of the tongue, resulting in a reduction of the posterior pharyngeal space and diameter15 and an increased respiratory effort that causes collapse of the pharyngeal tissues due to greater negative pressures.
2 CAUSES OF NASAL OBSTRUCTION
The causes for nasal obstruction can be broadly divided into structural, mucosal, or neuromuscular.14 Structural causes may include septal deviation, hypertrophy of the inferior or middle turbinates and fixed and inspiratory nasal valve collapse, which may or may not be secondary to prior nasal surgery or trauma. Of these causes, nasal valve dysfunction may contribute to symptoms in as many as 13% of adults that report chronic nasal obstruction.11 Although no data are available, it is likely that the increased respiratory efforts by OSAHS patients during episodes of apnea caused by palatal or tongue base obstruction make these patients more prone to nasal valve collapse. In children, in addition to developmental abnormalities like choanal atresia and craniofacial syndromes (e.g. Pierre Robin sequence), adenoidal and – to a lesser degree – tonsillar hypertrophy also constitute an important cause for nasal obstruction,16 both of which have an important correlation with OSAHS in this patient population. Chronic mouth breathing in these patients actually leads to acquired craniofacial abnormalities (e.g. the ‘adenoid face’), which further compromise the stability of the upper airway.17 The consequences of these alterations in cephalometric measurements that may originate during infancy may actually constitute the origin of the relationship between SDB and nasal obstruction. Earlier studies by Series4 established that sleep apneic patients with septal deviation that had subjective symptoms of nasal obstruction and subjectively disturbed sleep (mostly in the form of arousals) were more likely to improve both subjectively and objectively after correction of nasal obstruction if their cephalometric measurements were within normal ranges.
Nasal symptoms, findings, and even anatomical abnormalities (e.g. nasal septal deviation) are common in patients with sleep apnea,18 and data suggest that increased nasal resistance is more prevalent in patients who snore.19
Alterations in the nasal mucosa lead to nasal congestion, which involves the cavernous tissues of the turbinates. Common causes of nasal congestion include allergic rhinitis, vasomotor rhinitis, chronic sinusitis, and upper respiratory tract viral infections.20 These conditions are often associated with structural abnormalities, like septal deviation, which may also cause alterations in the nasal cycle. Chronic inflammation, as well as conditions like asthma, aspirin sensitivity or cystic fibrosis, lead to the development of nasal or nasopharyngeal polyps, which cause obstruction.20 Medical management of these conditions is an essential component in addressing nasal obstruction. Intranasal corticosteroid therapy for rhinitis showed improvement of OSAHS, but not snoring, in a randomized, placebo-controlled, crossover trial involving a group of 24 patients with mild to moderate sleep apnea, as reported by Kiely et al.21
Facial muscular weakness and impaired nasal reflexes (especially the ones involved in dilating the nose prior to inspiration), which occur secondary to neuropathy and facial palsy, are also important neuromuscular causes of nasal obstruction.2,11,12
3 DIAGNOSTIC EVALUATION OF NASAL OBSTRUCTION
3.1 NASAL AIRWAY STRUCTURE
The physical exam must include an examination of the internal and external nasal valves and the septum by means of anterior rhinoscopy. The nasal valves are common sites of obstruction in sleep apneic patients (see also Chapter 20), even more than deviated septa.10 The Cottle maneuver still remains an essential trial in the diagnosis of nasal valve obstruction. Fiberoptic endoscopy enables the surgeon to rule out the presence of any obstructing masses such as nasal polyps or nasopharyngeal tumors. Radiologic evaluation with CT scans may also have a confirmatory or strategic role for the preoperative evaluation in select cases, but is not essential.
3.2 THERAPEUTIC TRIALS
Medication trials include the administration of topical nasal steroids, sympathomimetic agents, and antihistamines, as well as allergic management in the form or desensitization. Patients that show significant improvement may choose not to undergo surgery. However, an underlying anatomical cause for obstruction needs to be addressed if a patient is unwilling to take medications permanently. The impact of decongestants such as oxymetazoline during nighttime sleep is valuable in assessing the impact of nasal obstruction in symptoms like snoring and overall in sleep-disordered breathing. The role of nasal valve collapse in nasal obstruction can also be confirmed with a trial of Breathe Right™ nasal strips (CNS Inc., Whippany, NJ), which help maintain the valves open through external dilatation, and prevent collapse during deep inspiration. Patients that have an adequate response in the form of reduced snoring and improved breathing are likely to benefit from nasal valve suspension procedures. Sleep partners may report decrease in snoring levels and observe how the patient is able to breathe through the nose alone, without opening the mouth.
3.3 NASAL AIRFLOW EVALUATION
Even a thorough clinical evaluation can oftentimes be unreliable and even contradictory. Patients are often not completely aware of the magnitude of nasal obstruction they might be experiencing, particularly during sleep. In the awake state, patients with atrophic rhinitis secondary to extensive turbinate resection have a persistent feeling of obstruction in spite of objective evidence of patency, whereas patients with deviated septa or nasal polyposis report no obstruction symptoms, despite evidence against a patent nasal airway.9 The objective evaluation of the nose can be divided into static or dynamic, depending on whether the structure of the nose or the airflow as a measure of the nasal function is being evaluated. In general, the evaluation of nasal airflow is a key element in the evaluation of improvement after surgical intervention. Measurements are performed at baseline and after procedures, in order to compare values and confirm improvement. Nasal airflow tests show a wide variety of normal values, which limits their use as stand-alone diagnostic tests.22
3.4 RHINOMANOMETRY AND ACOUSTIC RHINOMETRY
Nasal resistance can be calculated on the basis of the pressure gradients formed in the nose during inspiration. Rhinomanometry (RM) measures nasal airway resistance and airflow. It has two phases, passive and active, and it can be divided into anterior and posterior. Active RM requires the patient to generate airflow through inspiration. Passive RM utilizes external generation of airflow through the nose at a constant pressure. Anterior RM may reflect the status of the nares, nasal valves, and nasal cycling, and utilizes a device inserted into the nares. Posterior RM, in turn, utilizes a sensor inserted into the mouth which measures the nasopharynx, hence requiring substantial patient co-operation. These tests are also usually performed before and after the administration of nasal decongestants.23
Acoustic rhinometry evaluates nasal obstruction by analyzing reflected sound waves introduced through the nares. It is not invasive, is easily reproducible and it does not require patient co-operation. The results are expressed as cross-sectional dimensions of the nasal cavity, which closely approximate the smallest cross-sectional area and volume.24
The cross-sectional area (CSA) is measured at different points from the nares to the closest area of narrowing, which corresponds to the nasal valve area. Since a ‘normal’ CSA varies so much from patient to patient, an absolute value is not very useful for diagnosis or for confirmation of nasal valve area obstruction. Previously published work by the authors, however, has demonstrated that the ratio of the CSA during inspiration to the CSA at rest is highly diagnostic of nasal valve collapse.25 Normally, deep inspiration should not decrease the CSA. If it does, it is a sign of nasal valve collapse.
4 IMPACT OF NASAL SURGERY ON SNORING AND OSAHS
The most direct way to study the impact of an obstructed nasal airway is to examine the effect surgical correction of obstruction has on patients with SDB. A number of studies have been published that studied the effects on subjective (daytime somnolence, snoring) and objective parameters (Polysomnography) by addressing obstruction caused by the nasal valve, the septum, and the turbinates. A small study showed improvement in both subjective and objective parameters,26 but it only involved a total of six patients, without controls. A bigger, non-controlled study by Fairbanks27 showed improvement in snoring in 47 out of 113 enrolled subjects. Perhaps the only study to show consistent improvement of the Apnea/Hypopnea Index (AHI) was the study performed by Series et al.17 In this study, patients with mild OSAHS underwent lateral radiographs, from which cephalometric measurements were taken. Patients that showed an improvement on the AHI were those that had normal cephalometric measurements preoperatively (specifically mandibular plane to hyoid, decreased posterior airspace, or length of the soft palate). Patients with abnormal measurements did not improve with nasal surgery alone.
Contradicting these earlier findings, more recent reports show that less than 20% of patients achieve a 50% reduction in AHI with nasal surgery alone.28 A recent report by Virkkula et al. also failed to show improvement in snoring intensity or daytime sleepiness symptoms in a group of 40 patients after nasal surgery for an obstructed nasal airway, in spite of decreased nasal resistance as measured by rhinomanometry.29 Data on patients undergoing nasal surgery alone for the treatment of OSAHS30 showed that, despite subjective improvement in patients undergoing submucous resection (SMR) of the septum with or without SMR of the inferior turbinates, an overall improvement in OSAHS on the basis of polysomnographic data could not be demonstrated in most patients. In fact, when pre- and postnasal surgery AHI have been compared in mild, moderate, and severe OSAHS patients, a tendency towards worsening of this parameter has been observed, although statistical significance for the postoperative increase in AHI was only observed in mild OSAHS cases26 (Table 19.1). This paradoxical effect has been previously described,4 and the numerous hypotheses that have been proposed for this phenomenon are based on the increased comfort that patients experience by being able to breathe through the nose. Better subjective sleep quality due to a patent nasal airway is achieved, which leads to deeper and more comfortable sleep, resulting in increased apneic episodes due to increased collapsibility of the upper airway. Sleep fragmentation results, particularly in moderate to severe sleep apnea patients. The experimental and clinical evidence of less sleep fragmentation and disturbance, thus, applies only to non-OSAHS patients in whom nasal breathing is improved after surgery.7,31 Another possible explanation for worsening of the AHI from the first to the second night of study might occur because the patients experience what is also known as the ‘first night effect’,29 where they become adapted to the test environment after the second or third night of study, and thus are able to sleep better.
Table 19.1 Respiratory Disturbance Index and OSAHS procedure
| OSAHS classification/type of procedure | Mean RDI | |
|---|---|---|
| Pre-op | Post-op | |
| Mild/nasal | 8.69 | 18.7 |
| Mild/nasal+PIT | 12.9 | 9.3 |
| Moderate/nasal | 19.4 | 28.9 |
| Moderate/nasal+PIT | 30.3 | 26.2 |
| Severe | 55.8 | 56 |
Intervention at other levels of obstruction, without a doubt, increase the impact that relieving nasal obstruction has on the overall picture of OSAHS, and even on nasal obstruction by itself. Correction of nasal airway obstruction has been shown to have a significant impact on OSAHS when performed as a part of a multilevel approach to treat patients with OSAHS. Friedman et al. have shown that patients with nasal obstruction and OSAHS achieved significantly better objective and subjective success rates when soft palate implant insertion for the treatment of snoring and mild to moderate OSAHS was performed together with nasal surgery32 (Table 19.1). A more rigid palate is probably less prone to collapsing (requiring an increased pharyngeal closing pressure) and thus the increased flow of air through the operated nose, which actually counteracts a normal effect of increased nasal resistance in the recumbent position,33 does not have the negative effect on the patient’s OSAHS.
5 IMPACT OF NASAL SURGERY ON BLOOD OXYGEN SATURATION
Olsen and Kern, in an excellent review of nasal influences on OSAHS,34 documented the importance of the nasal cycle and the nasopulmonary reflex in maintaining adequate blood oxygenation. The lowest oxygen saturation levels (LSaO2) are directly affected by the patency of the nasal airway, with or without persistent OSAHS. While the increase in LSaO2 might be discrete, nasal interventions might at least maintain adequate blood oxygenation levels.30 This supports the necessity of correcting an obstructed nasal airway as part of the overall strategy of surgical intervention for OSAHS.
6 IMPACT OF NASAL SURGERY ON NASAL CONTINUOUS AIRWAY PRESSURE (NCPAP) THERAPY
Continuous positive airway pressure (CPAP) is currently the mainstay for the management of OSAHS. Poor compliance (sometimes less than 50%) with this management strategy35 – particularly of nCPAP – has been attributed to the discomfort of the high-pressure air being delivered through partially obstructed nasal airways. Surgical correction of nasal obstruction can have a significant Impact on the nCPAP pressure needed to decrease the Respiratory Disturbance Index as much as possible without disrupting the patient’s sleep. This makes it more tolerable, which results in an increase in compliance in some patients.36 Friedman et al. confirmed a significant decrease in CPAP titration levels after nasal surgery alone30 (Table 19.2), after Series et al. initially described this finding in a small series of patients.4 Powell showed that patients actually report a subjective improvement in nasal obstruction, which seemed to be in direct relationship with the degree of adherence to CPAP therapy.5 In fact, it has been proposed that CPAP in itself might promote the development of nasal inflammation, and in some patients even vasomotor rhinitis, particularly when using CPAP machines that do not control the temperature of the delivered air nor humidify it. It is likely that this effect might be even more pronounced in patients with an underlying cause for nasal obstruction.
Table 19.2 CPAP titration levels before and after nasal surgery for OSA
| OSAHS patients | Mean CPAP (cm H2O) | |
|---|---|---|
| Pre-op | Post-op | |
| Total (n=22) | 9.3 | 6.7 |
| Severe (n=13) | 10.07 | 7.42 |
| Moderate (n=4) | 9.5 | 6.5 |
| Mild (n=5) | 7.2 | 5 |
7 CONCLUSION
Although nasal obstruction may be a major contributing factor of OSAHS in some patients, this is certainly not the case in the majority. Selected patients who respond to a diagnostic trial of artificial nasal airway improvement with topical and systemic decongestants and steroids, along with external nasal dilators (e.g. Breathe Right™ strips), may also benefit from definitive correction of the nasal airway, with elimination of snoring and improvement in OSAHS. The majority of patients with nasal obstruction and OSAHS will likely benefit from a multilevel surgical approach. If nasal surgery is undertaken alone, it is important to inform patients that it may not only fail to cure, but may even aggravate snoring and OSAHS in certain cases. Nasal surgery also has a significant impact in improving patients’ subjective symptoms, like daytime sleepiness and quality of sleep. It also constitutes a valuable intervention in patients that need nCPAP management for their OSAHS.
1. Boudewyns AN, Heyning PHVD, Backer WAD. Site of upper airway obstruction in obstructive sleep apnea and influence on sleep stage. Eur Respir J. 1997;10:2566-2572.
2. Mirza N, Lanza DC. The nasal airway and obstructed breathing during sleep. Otolaryngol Clin North Am. 1999;32:243-262.
3. Carpenter JE. Mental aberration and attending hypertrophic rhinitis with subacute otitis media. JAMA. 1892;19:539-542.
4. Series F, St Pierre S, Carrier G. Effects of surgical correction of nasal obstruction in the treatment of obstructive sleep apnea. Am Rev Respir Dis. 1992;146:1261-1265.
5. Powell N. Radiofrequency treatment of turbinate hypertrophy in subjects using CPAP: a randomized, double-blind, placebo-controlled trial. Laryngoscope. 2001;111:1783-1790.
6. Vijay SD, Phillipson EA. Nasal surgery in the management of sleep apnea. Ann Otol Rhinol Laryngol. 1985;94:550-554.
7. Olsen KD, Kern EB, Westbrook PR. Sleep and breathing disturbance secondary to nasal obstruction. Otolaryngol Head Neck Surg. 1981;89:804-810.
8. Papsidero MJ. The role of nasal obstruction in obstructive sleep apnea syndrome. Ear Nose Throat J. 1993;72:82-84.
9. Rappai M, Collop N, Kemp S, deShazo R. The nose and sleep-disordered breathing: what we know and what we do not know. Chest. 2003;124:2309-2323.
10. Constantian MB, Clardy RB. The relative importance of septal and nasal valvular surgery in correcting airway obstruction in primary and secondary rhinoplasty. Plast Reconstr Surg. 1996;98:38-54.
11. Schlosser RJ, Park SS. Functional nasal surgery. Otolaryngol Clin North Am. 1999;32:37-51.
12. Tarabichi M, Fanous N. Finite element analysis of airflow in the nasal valve. Arch Otolaryngol Head Neck Surg. 1993;119:638-642.
13. Cole P, Haight JS. Mechanisms of nasal obstruction in sleep. Laryngoscope. 1984;94:1557-1559.
14. Chen W, Kushida CA. Nasal obstruction in sleep-disordered breathing. Otolaryngol Clin North Am. 2003;36:437-460.
15. De Vito A, Berrettini S, Carabelli A, et al. The importance of nasal resistance in obstructive sleep apnea syndrome: a study with positional rhinomanometry. Sleep Breath. 2001;5:3-11.
16. Rizzi M, Onorato J, Andreoli A, et al. Nasal resistances are useful in identifying children with severe obstructive sleep apnea before polysomnography. Int J Pediatr Otorhinolaryngol. 2002;65:7-13.
17. Series F, Pierre SS, Carrier G. Surgical correction of nasal obstruction in the treatment of obstructive sleep apnea: importance of cephalometry in predicting outcome. Thorax. 1993;48:360-363.
18. Ancoli-Israel S, Kripke DF, Mason W, Messin S. Sleep apnea and nocturnal myoclonus in a senior population. Sleep. 1981;4:349-358.
19. Young T, Finn L, Kim H. Nasal obstruction as a risk factor for sleep-disordered breathing. J Allergy Clin Immunol. 1997;99:S757-S762.
20. Corey JP, Houser SM, Ng BA. Nasal congestion: a review of its etiology, evaluation, and treatment. Ear Nose Throat J 2000;79:690–693, 696, 698.
21. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnea in patients with co-existing rhinitis. Thorax. 2004;59:50-55.
22. Corey JP, Gungor A, Nelson R, Liu X, Fredberg J. Normative standards for nasal cross-sectional areas by race as measured by acoustic rhinometry. Otolaryngol Head Neck Surg. 1998;119:389-393.
23. Grymer LF, Hilberg O, Pedersen OF, Rasmussen TR. Acoustic rhinometry: values from adults with subjective normal nasal patency. Rhinology. 1991;29:35-47.
24. Fisher EW, Daly NJ, Morris DP, Lund VJ. Experimental studies of the resolution of acoustic rhinometry in vivo. Acta Otolaryngol. 1994;114:647-650.
25. Vidyasagar R, Friedman M, Ibrahim H, Bliznikas D, Joseph NJ. Inspiratory and fixed nasal valve collapse: clinical and rhinomanometric assessment. Am J Rhinol. 2005;19:370-374.
26. Dayal VS, Phillipson EA. Nasal surgery in the management of sleep apnea. Ann Otol Rhinol Laryngol. 1985;94:550-554.
27. Fairbanks D. Effect of nasal surgery on snoring. South Med J. 1985;78:268-270.
28. Verse T, Maurer JT, Pirsig W. Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope. 2002;112:64-68.
29. Virkkula P, Bachour A, Hytonen M, Salmi T, Malmberg H, Hurmerinta K, Maasita P. Snoring is not relieved by nasal surgery despite improvement in nasal resistance. Chest. 2006;129:81-87.
30. Friedman M, Tanyeri H, Lim JW, Landsberg R, Vaidyanathan K, Caldarelli D. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;122:71-74.
31. Zwillich CW, Pickett J, Hanson FN, Weil JV. Disturbed sleep and prolonged apnea during nasal obstruction in normal men. Am Rev Respir Dis. 1981;124:158-160.
32. Friedman M, Vidyasagar R, Bliznikas D, Joseph NJ. Patient selection and efficacy of pillar implant technique for the treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2006;134:187-196.
33. Tvinnereim M, Cole P, Haight JS, Mateika S, Hoffstein V. Sleep and posture. Laryngoscope. 1994;104:846-849.
34. Olsen KD, Kern EB. Nasal influences on snoring and obstructive sleep apnea. Mayo Clin Proc. 1990;65:1095-1105.
35. Practice parameters for the treatment of obstructive sleep apnea in adults: the efficacy of surgical modifications of the upper airway. An American Sleep Disorders Association Report. Sleep. 1996;19:152-155.
36. Pirsig W, Verse T. Long-term results in the treatment of obstructive sleep apnea. Eur Arch Otolaryngol. 2000;257:570-577.