Eczema – Other forms
The other main types of eczema are seborrhoeic, discoid, venous, asteatotic and hand dermatitis.
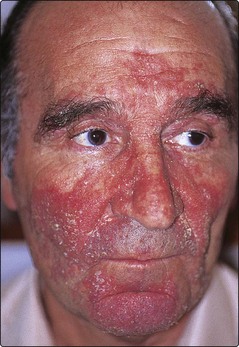
Seborrhoeic dermatitis
Seborrhoeic dermatitis is a chronic, red, scaly, inflammatory eruption usually affecting the scalp and face (Table 1).
| Site of seborrhoeic dermatitis | Differential diagnosis |
|---|---|
| Face | Psoriasis, contact dermatitis, rosacea |
| Scalp | Psoriasis, fungal infection |
| Trunk | Psoriasis, pityriasis versicolor, fungal infection |
Clinical presentation
There are four common patterns:
1. Scalp and facial involvement. Excessive dandruff, with an itchy scaly erythematous eruption affecting the sides of the nose, scalp margin, eyebrows and ears (Fig. 1). Blepharitis may occur. Most common in young adult males.
2. Petaloid. A dry, scaly patch of eczema over the presternal area.
3. Pityrosporum folliculitis. An erythematous follicular eruption with papules or pustules over the back (Fig. 2).
4. Flexural. Involvement of the axillae, groin and submammary areas by a moist intertrigo, often secondarily colonized by Candida albicans. Seen in the elderly (do not confuse with the similarly named infantile eruption, p. 116).
Discoid (nummular) eczema
Discoid eczema is an eczema of unknown aetiology characterized by coin-shaped lesions on the limbs; it typically affects middle-aged or elderly men (Fig. 3). Younger subjects, especially in dark skin types, may have atopic eczema.
Venous (stasis) eczema
Venous eczema affects the lower legs (Fig. 4) and is associated with underlying venous disease (p. 72). Incompetence of the deep perforating veins increases hydrostatic pressure in dermal capillaries. Pericapillary fibrin deposition impedes oxygen diffusion and leads to clinical changes.
Hand dermatitis
Allergic causes need excluding, and most adults with hand dermatitis require patch testing. Fungal infection is ruled out by microscopy and culture, especially in unilateral hand dermatitis, and the feet are examined because tinea pedis can provoke a hand dermatitis as an ‘id’ phenomenon (p. 58). A core of patients are left who have an endogenous recurrent hand dermatitis often characterized by sago-like vesicles on the sides of the fingers, on the palms and sometimes on the soles.
Clinical presentation
Hand dermatitis often presents as a chronic eczema, but may appear as a vesicular eruption known as pompholyx. Vesicles may be seen with atopic eczema or contact dermatitis but, in pompholyx, there is usually no associated disorder. The onset is in young adults, particularly in warm weather, and it is often recurrent. Involvement can be confined to a few microvesicles on the fingers, or it can be extensive with bullae affecting the whole hand (Fig. 5). Some of these patients are nickel sensitive.
Management
Acute pompholyx requires drainage of large blisters and the application (once or twice a day) of wet dressings (e.g. immersed in 0.01% aqueous potassium permanganate or Burow’s solution of 0.65% aqueous aluminium acetate). Oral antibiotics are given if bacterial infection is present. Some dermatologists prescribe systemic steroids, but these are usually not necessary. Once the acute stage settles, potent or highly potent steroid lotions or creams are used with cotton gloves. For chronic or subacute cases, a steroid ointment and emollients are helpful. Advice for patients with hand dermatitis is given in Table 2. Alitretinoin (p. 34) has recently been licensed for severe chronic hand eczema refractory to potent topical corticosteroids.
Table 2 Hints on hand care for patients with hand dermatitis
| Hand washing |
| Use warm water and unscented soap; avoid paper towels and hot air dryers; instead use a dry cotton towel. |
| Protection |
| Avoid wet work if possible, or otherwise wear cotton gloves under vinyl or nitrile gloves; wear gloves in cold weather and for dusty work. |
| Medicaments |
| Use emollients regularly throughout the day; apply steroid ointments twice a day. |
| Avoid handling |
| Shampoos, hair preparations, detergents, solvents, polishes, certain vegetables (e.g. tomatoes, potatoes), peeling fruits (e.g. oranges) and cutting raw meat. |
Asteatotic eczema (eczéma craquelé)
Asteatotic eczema is a dry eczema with fissuring and cracking of the skin, often affecting the limbs in the elderly (Fig. 6).
Other eczemas
Other types of eczema are occasionally encountered. They include: lichen simplex chronicus, lichen striatus, juvenile plantar dermatosis (p. 116) and napkin (diaper) eruption (p. 116).
Lichen simplex chronicus (neurodermatitis)
Neurodermatitis is an area of lichenified eczema due to repeated rubbing or scratching, as a habit or due to ‘stress’. It usually occurs as a single plaque on the lower leg, back of the neck or in the perineum (pruritus vulvae/ani: p. 121). The skin markings are exaggerated, and pigmentation may occur. Asian and Chinese people are particularly susceptible. Sometimes a nodular lichenification known as prurigo nodularis develops on the shins and forearms. Emollients, topical steroids, weak tar paste and tar-impregnated bandages are the mainstay of treatment.
Lichen striatus
Lichen striatus is a rare self-limiting linear eczema affecting a limb and occurring in adolescents (p. 19).
Eczema
 Seborrhoeic dermatitis commonly affects the scalp and face. It responds to combined antimicrobial/hydrocortisone creams.
Seborrhoeic dermatitis commonly affects the scalp and face. It responds to combined antimicrobial/hydrocortisone creams.
 Discoid eczema often presents as coin-shaped lesions on limbs of the middle-aged or elderly. It improves with moderate potency topical steroids.
Discoid eczema often presents as coin-shaped lesions on limbs of the middle-aged or elderly. It improves with moderate potency topical steroids.
 Venous eczema is associated with venous disease. It responds to emollients and low or moderate potency topical steroids.
Venous eczema is associated with venous disease. It responds to emollients and low or moderate potency topical steroids.
 Hand dermatitis: multiple and mixed aetiology; determine causes by exclusion.
Hand dermatitis: multiple and mixed aetiology; determine causes by exclusion.
 Asteatotic eczema: the eczéma craquelé of elderly skin. Treat with emollients or low potency topical steroids.
Asteatotic eczema: the eczéma craquelé of elderly skin. Treat with emollients or low potency topical steroids.
 Lichen simplex chronicus: an area of lichenified eczema induced by persistent scratching, often found on the posterior neck or lower leg.
Lichen simplex chronicus: an area of lichenified eczema induced by persistent scratching, often found on the posterior neck or lower leg.