10 Echocardiography in the Patient with Right Heart Failure
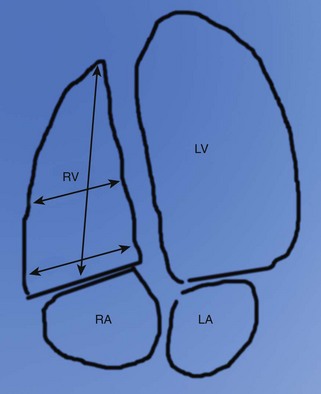
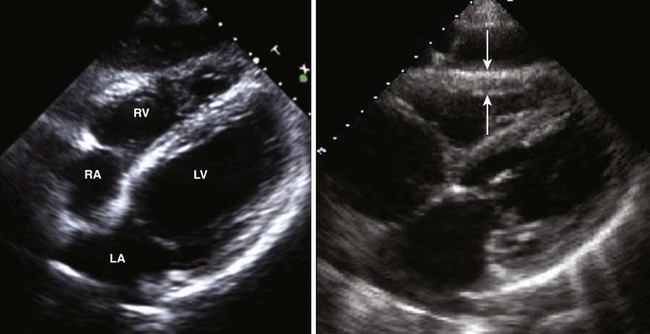
Basic Principles of Right Ventricular Imaging
Step-by-Step Approach
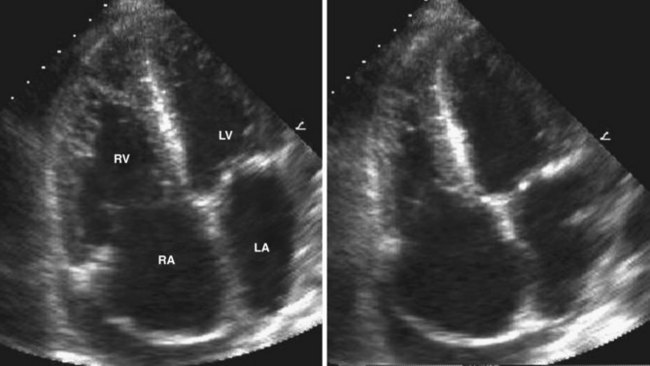
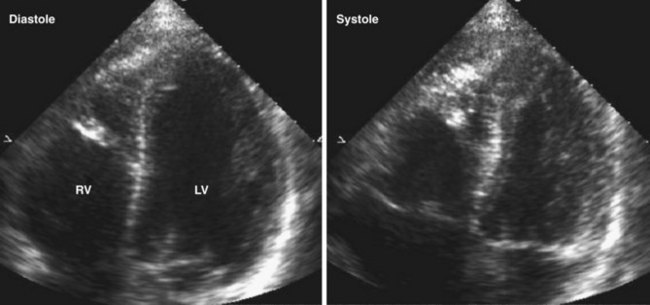
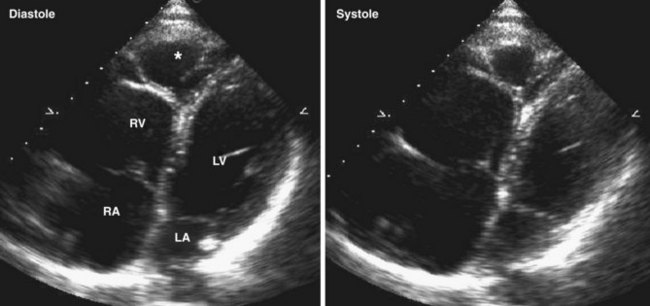
Step 1: Analysis of Right Ventricular Size
Key Points
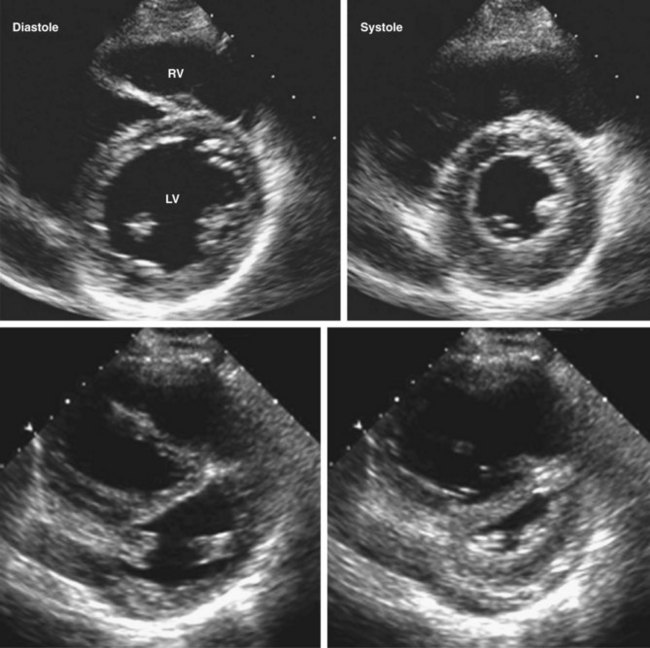
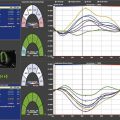
Step 2: Analysis of RV Volume and Systolic Function
Key Points
Step 3: Evaluation of RV Wall Motion
Key Points
Identify the Cause of Right Heart Failure
RV Infarction
Step-by-Step Approach
Step 1: Assess LV Wall Motion and Systolic Function, and Look for Mechanical Complications of Myocardial Infarction
Pulmonary Arterial Hypertension
Step-by-Step Approach
Step 1: Assess RV Size and Function
Key Points
Step 2: Look for Associated Right Heart Findings of Pulmonary Hypertension
Key Points
Acute Pulmonary Embolism
Step-by-Step Approach
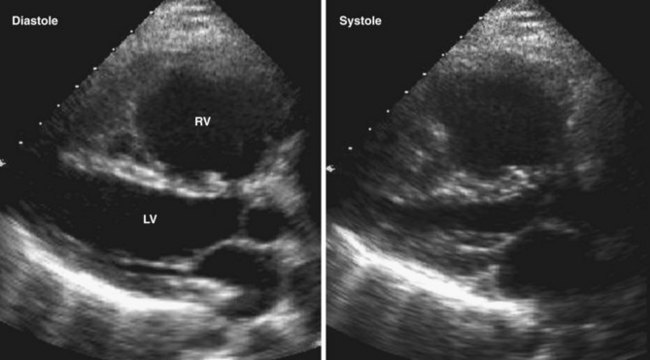
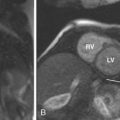
Step 1: Assess RV Size, Shape, and Function
Intracardiac Shunt
Step-by-Step Approach
Step 1: Assess RA and RV Size
Step 3: Look for Intracardiac Shunting
Key Points
Cardiomyopathy Affecting the RV
Measurement of Prognostic Echocardiographic Parameters
PA Systolic Pressure
Step-by-Step Approach
Step 1: Record Maximum VTR
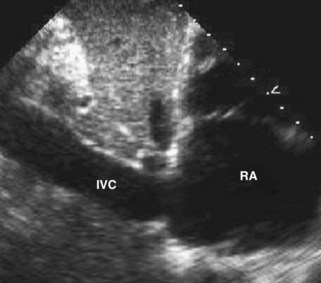
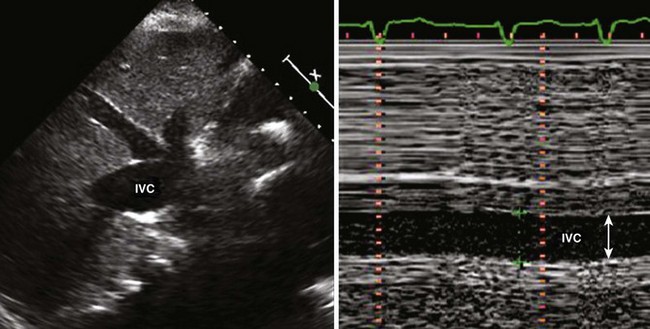
Step 2: Estimate RAP Noninvasively
Key Points
| Degree of Inspiratory IVC Collapse | Estimated RAP |
|---|---|
| Full collapse | 5 mm Hg |
| Greater than 50% collapse | 10 mm Hg |
| Less than 50% collapse | 15 mm Hg |
| No collapse | 20 mm Hg |
Step 3: Calculate PASP Using VTR and RAP
Key Points
PA Diastolic Pressure
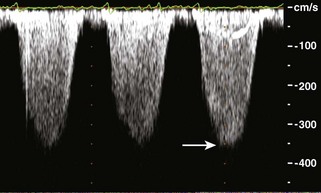
Pulmonary Vascular Resistance
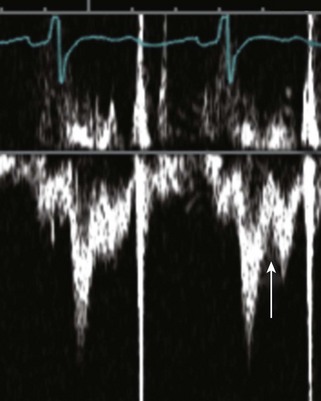
Spectral Doppler of RVOT
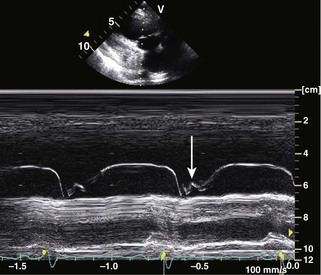
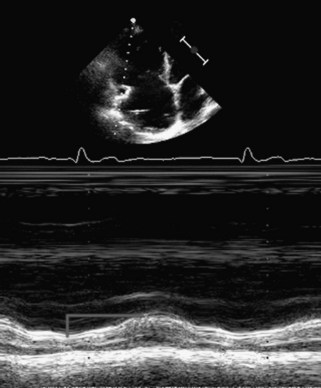
Tricuspid Annular Plane Systolic Excursion
1 Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003;41:1021-1027.
2 Arkles JS, Opotowsky AR, Ojeda J, et al. Shape of the RV Doppler envelope predicts hemodynamics and right heart function in pulmonary hypertension. Am J Respir Crit Care Med. 2011;183:268-276.
3 Armstrong WF, Ryan T, Feigenbaum H. Feigenbaum’s Echocardiography, 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010.
This is a comprehensive textbook of echocardiography.
4 Ghio S, Klersy C, Magrini G, et al. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol. 2010;140:272-278.
5 Hausmann D, Daniel WG, Mugge A, Ziemer G, Pearlman AS. Value of transesophageal color Doppler echocardiography for detection of different types of atrial septal defect in adults. J Am Soc Echocardiogr. 1992;5:481-488.
6 Kitabatake A, Inoue M, Asao M, et al. Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation. 1983;68:302-309.
7 Lahm T, McCaslin CA, Wozniak TC, et al. Medical and surgical treatment of acute right ventricular failure. J Am Coll Cardiol. 2010;56:1435-1446.
8 Oh JK, Seward JB, Tajik AJ. The Echo Manual, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
This is a comprehensive textbook of echocardiography.
9 Otto CM. Textbook of Clinical Echocardiography, 4th ed. Philadelphia: Saunders Elsevier; 2009.
This is a comprehensive textbook of echocardiography.
10 Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685-713.
11 Rydman R, Soderberg M, Larsen F, Caidahl K, Alam M. Echocardiographic evaluation of right ventricular function in patients with acute pulmonary embolism: A study using tricuspid annular motion. Echocardiography. 2010;27:286-293.
12 Watts JA, Marchick MR, Kline JA. Right ventricular heart failure from pulmonary embolism: Key distinctions from chronic pulmonary hypertension. J Card Fail. 2010;16:250-259.
13 Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70:657-662.