3 Echocardiography in the Cardiac Catheterization Laboratory
Echocardiographic Techniques
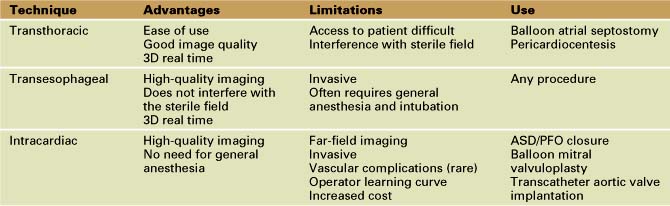
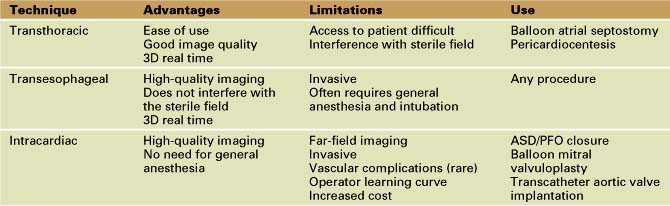
Real-time three-dimensional (3D) echocardiography is a more recently developed technique that can be used to image the anatomy, catheters, and devices. It allows for improved understanding of the relationships between the device and cardiac structures. The image quality and resolution are inferior to those of the other 2D techniques (Table 3-1).
Transcatheter Closure of Atrial Septal Defects/Patent Foramen Ovale
Technique
Step-by-Step Approach
1 Assess Anatomy
Secundum ASDs and PFO are amenable to transcatheter closure.
Key Points
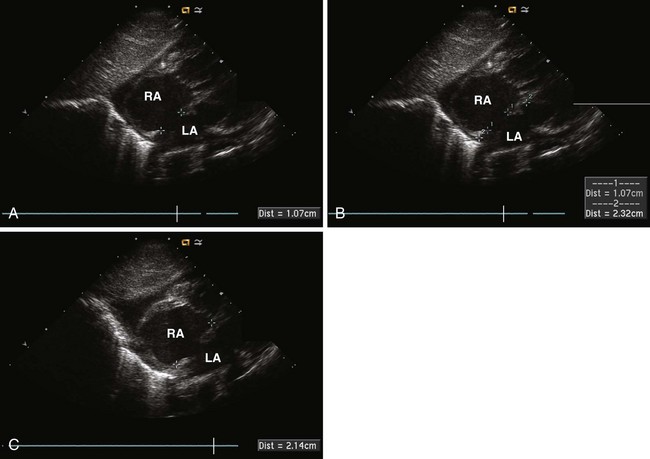
2 Dynamic Sizing
A sizing balloon is often used to measure the stretched diameter of the ASD.
Key Points
3 Device Placement
Key Points
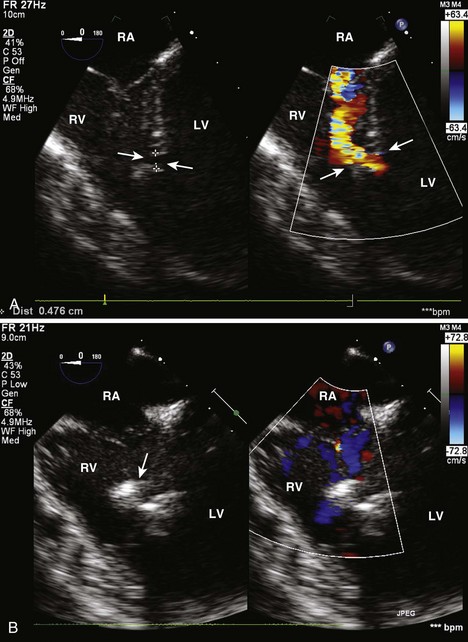
Transcatheter Closure of Muscular Ventricular Septal Defects
Technique
TEE generally provides the best imaging for percutaneous closure of muscular VSDs.
Step-by-Step Approach
1 Assess Anatomy
Percutaneous closure is possible for select muscular VSDs.
Key Points
2 Device Placement
Key Points
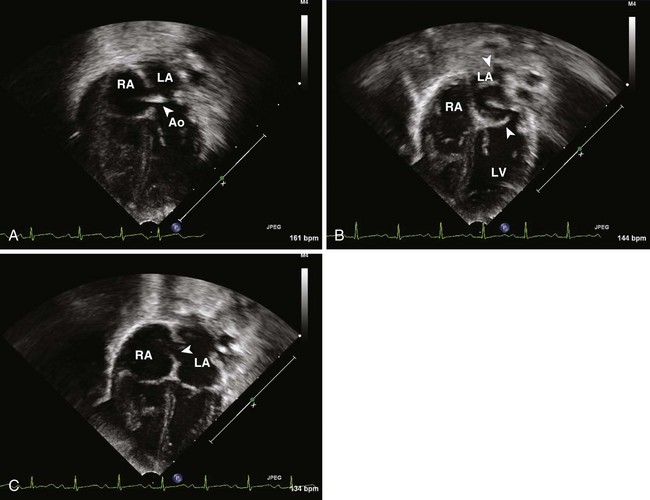
Balloon Atrial Septostomy
Technique
Step-by-Step Approach
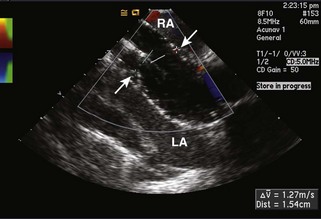
2 Balloon Atrial Septostomy
Echocardiographic guidance is more than adequate to perform balloon atrial septostomy safely.
Key Point
Balloon Mitral Valvuloplasty
Technique
Step-by-Step Approach
1 Initial Assessment
Key Points
2 Balloon Dilation
Echocardiographic visualization of the balloon during inflation is often helpful.
3 After Balloon Dilation
Echocardiography is used to assess the success of the procedure.
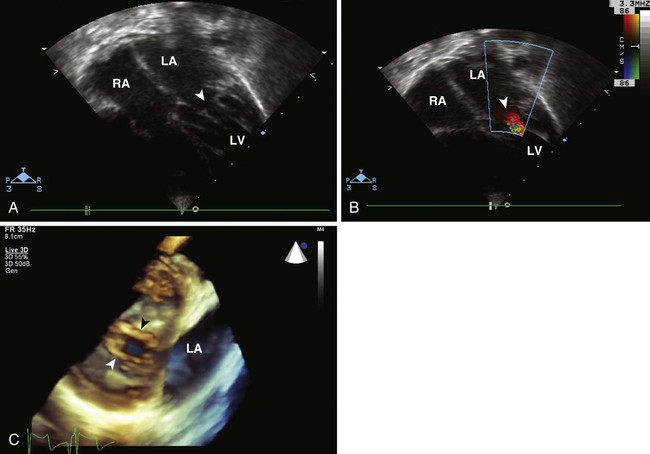
Transcatheter Aortic Valve Implantation
Transcatheter aortic valve implantation is an investigational technique.
Technique
Step-by-Step Approach
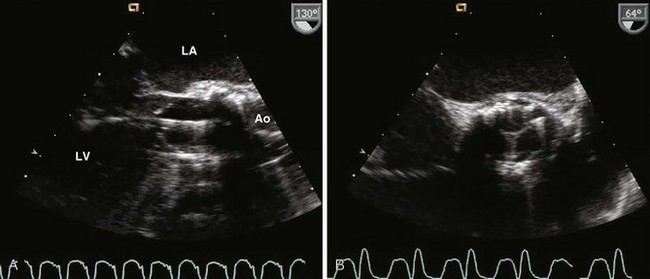
1 Assess Anatomy
Accurate assessment of aortic valve anatomy is dependent on echo.
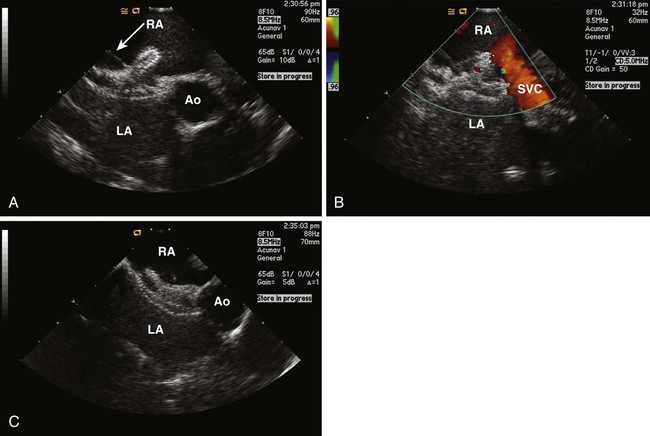
2 During the Procedure
Echocardiography can be used to confirm correct wire placement and balloon position during dilation (Fig. 3-7A).
Key Points
3 After Deployment
Echocardiography is crucial to the assessment of the valve after deployment (see Fig. 3-7B).
Key Points
1 Hellenbrand WA, Fuhey JT, McGowan FX, et al. Transesophageal guidance of transcatheter closure of atrial septal defect. Am J Cardiol. 1990;66:207-213.
2 Hijazi ZM, Shivkumar K, Sahn DJ. Intracardiac echocardiography during interventional and electrophysiological cardiac catheterization. Circulation. 2009;119:587-596.
3 Kim S, Hijazi ZM, Lang R, et al. The use of intracardiac echocardiography and other intracardiac imaging tools to guide non-coronary cardiac interventions. J Am Coll Cardiol. 2009;53:2117-2128.
4 Moss RG, Ivens E, Pasupati S, et al. Role of echocardiography in percutaneous aortic valve implantation. J Am Coll Cardiol Imaging. 2008;1:15-24.
5 Mullen MJ, Dias BF, Walker F, et al. Intracardiac echocardiography guided device closure of atrial septal defects. J Am Coll Cardiol. 2003;41:285-292.
6 Perk G, Lang RM, Garcia-Fernandez MA, et al. Use of real time three-dimensional transesophageal echocardiography in intracardiac catheter based interventions. J Am Soc Echocardiogr. 2009;22:865-882.
7 Silvestry FE, Kerber RE, Brook MM, et al. Echocardiography-guided interventions. J Am Soc Echocardiogr. 2009;22:213-229.