4 Echocardiographic Parameters Important for Decision Making
Anatomic Imaging
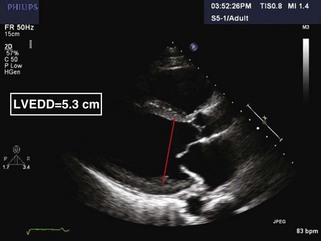
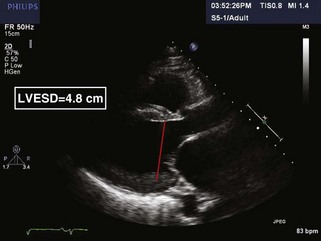
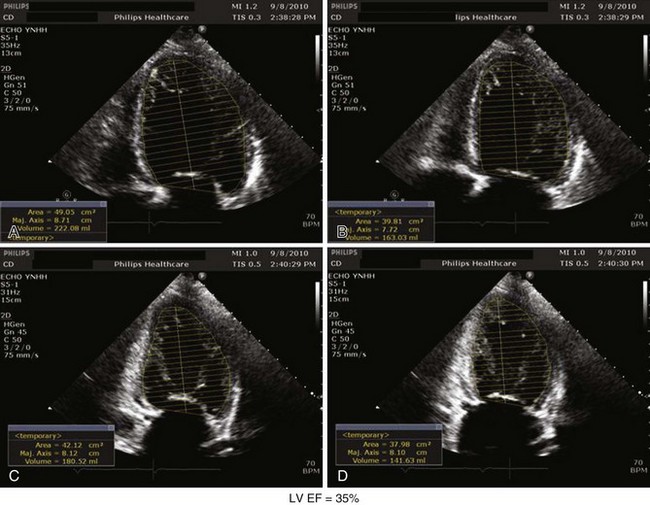
LV Cavity Size and Systolic Function
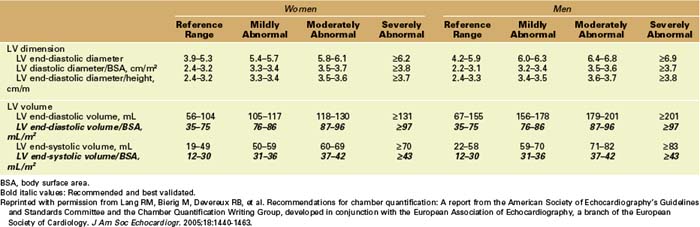
Step 1: Determination of LV Cavity Size by 2D Echocardiography in Parasternal Long-Axis View
TABLE 4-1 RECOMMENDATIONS FROM THE AMERICAN SOCIETY OF ECHOCARDIOGRAPHY FOR THE QUANTIFICATION OF LEFT VENTRICULAR SIZE AND VOLUME
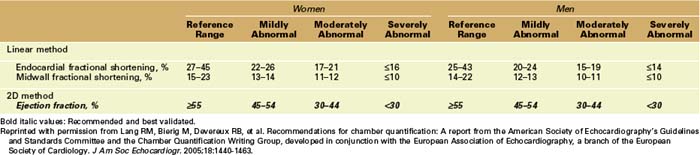
Step 2: Estimation of LV Volumes and EF by 2D by Simpson’s Method
TABLE 4-2 RECOMMENDATIONS FROM THE AMERICAN SOCIETY OF ECHOCARDIOGRAPHY FOR THE QUANTIFICATION OF LEFT VENTRICULAR FUNCTION
Key Point
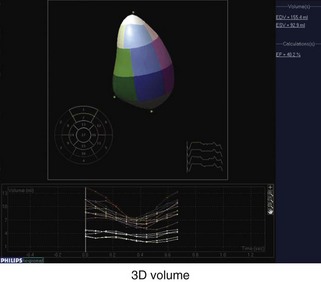
Step 3: Determination of Estimated LV Volumes and EF by 3D
Right Ventricle
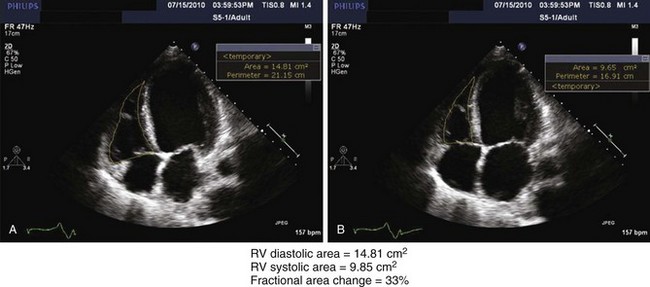
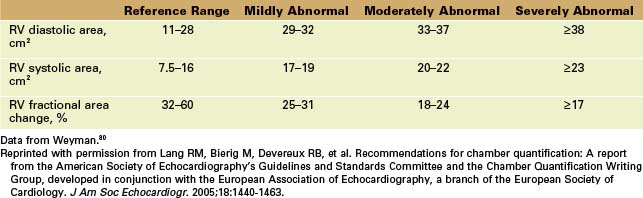
Step 1: Determination of Right Ventricular Size by 2D
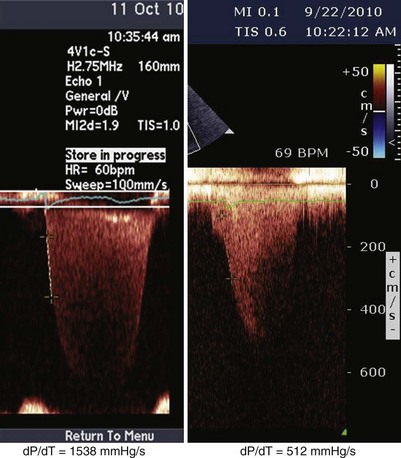
Step 2: Determination of RV Systolic Function
Key Points
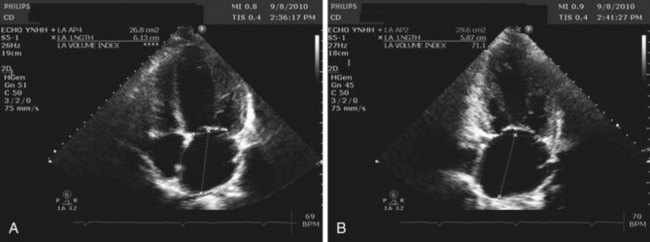
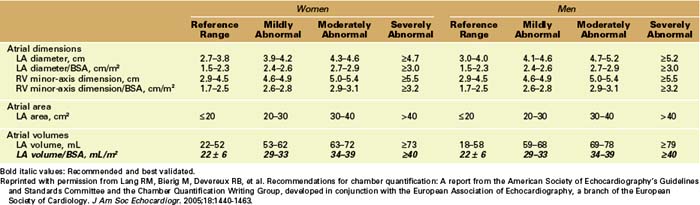
LA Volume (LAV)
Step 1: Obtaining 2D Images
Step 2: Calculating LAV
where A1 is the area in the 4C view, A2 is the area in the 2-chamber view, and L is the shorter of the major axes obtained (Table 4-4).
Physiologic Data
LV Diastolic Function
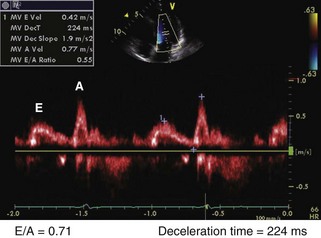
Step 1: LV Inflow
Key Points
Step 2: Deceleration Time (DT) of Early Diastolic Filling
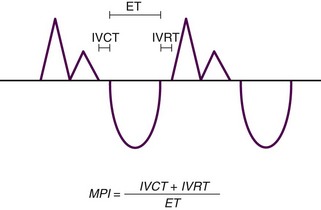
Step 3: Isovolumic Relaxation Time (IVRT) and Myocardial Performance Index (MPI)
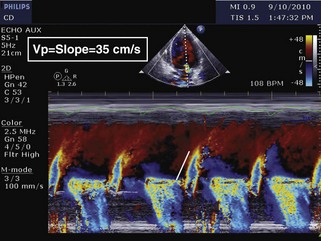
Step 4: Color Doppler M-Mode of LV Inflow to Obtain Propagation Velocity (Vp)
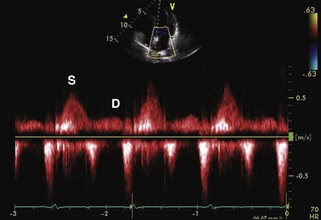
Step 5: Spectral Doppler of Pulmonary Veins
Key Point
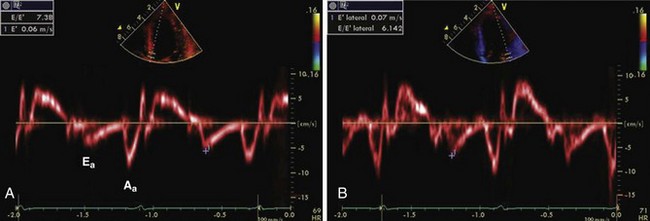
Step 6: TDI of Mitral Annulus
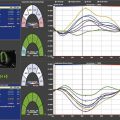
Step 7: Overall Assessment of LV Diastolic Function
Mitral Regurgitation
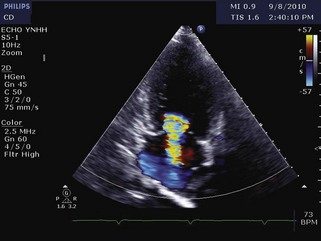
Step 1: Overall Assessment of Etiology
Step 3: Color Doppler Evaluation
Step 4: Spectral Doppler Evaluation
Key Point
Step 5: Integration
Pulmonary Artery Systolic Pressure
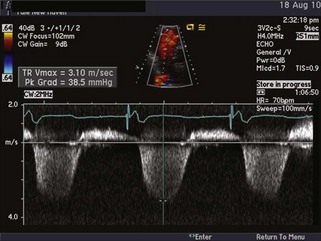
Step 1: Estimating the RV-to-RA Pressure Gradient
Key Points
Step 2: Estimating the RA Pressure
Step 3: Estimating PASP
1 Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440-1463.
2 Haddad F, Doyle R, Murphy AD, Hunt SA. Right ventricular function in cardiovascular disease, part II: Pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717-1731.
3 Leung DY, Boyd A, Ng AA, Chi C, Thomas L. Echocardiographic evaluation of the left atrial size and function: Current understanding, pathophysiologic correlates, and prognostic implications. Am Heart J. 2008;156:1056-1064.
4 Meta-Analysis Research Group in Echocardiography (MeRGE) AMI CollaboratorsMøller JE, Whalley GA, Dini FL, et al. Independent prognostic importance of a restrictive left ventricular filling pattern after myocardial infarction: An individual patient meta-analysis. Circulation. 2008;117:2591-2598.