10 Echocardiographic Imaging of Single-Ventricle Lesions
Key Points
This chapter discusses in detail the imaging of these three lesions:
Hypoplastic Left Heart Syndrome
Definition and Prevalence
Parasternal Long Axis View (Fig. 10-1)
Parasternal Short Axis View
Apical Four-Chamber View
Subcostal Four-Chamber or Coronal View
Subcostal Short Axis or Sagittal View
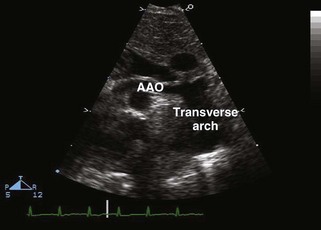
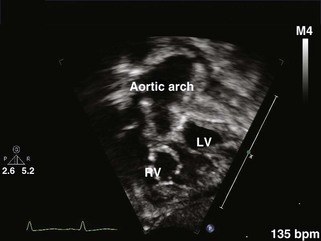
Suprasternal Long Axis View
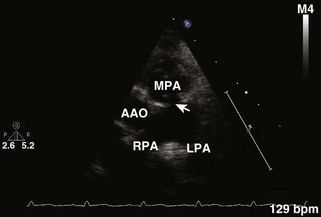
Suprasternal Short Axis View
Double-Inlet Left Ventricle
Key Points
Definition and Prevalence
Pertinent information is obtained from the standard views by 2D and Doppler.
Parasternal Long Axis View
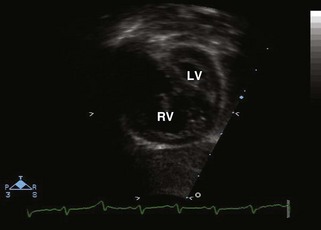
Parasternal Short Axis View
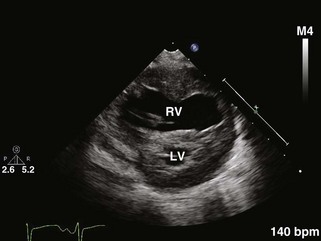
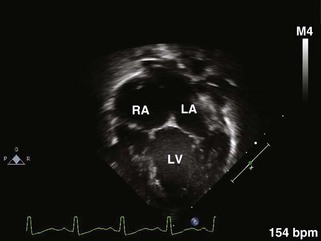
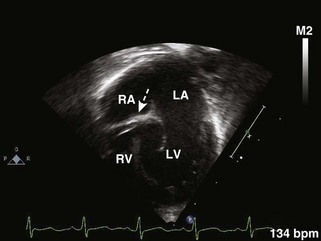
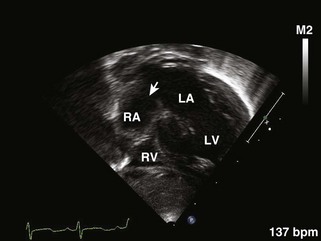
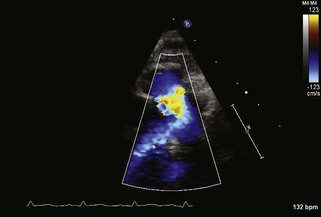
Apical Four-Chamber Views (Fig. 10-8)
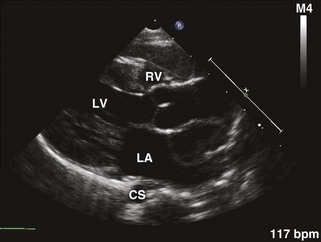
Subcostal Four-Chamber Coronal View
Tricuspid Atresia
Key Points
Definition and Prevalence
Pertinent information is obtained from the standard views.
Parasternal Long Axis View
Parasternal Short Axis View
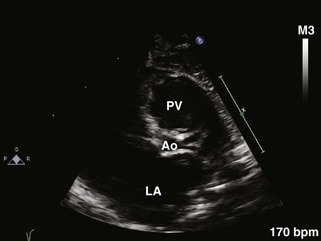
Apical Four-Chamber View (Fig. 10-10)
Subcostal Four-Chamber Coronal View
Subcostal Short Axis Sagittal View
Suprasternal Long Axis View
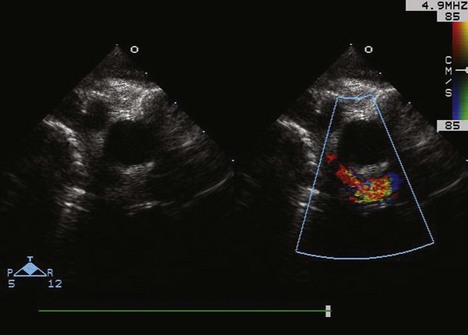
Postoperative Evaluation
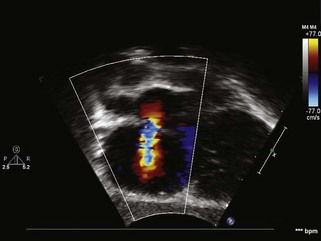
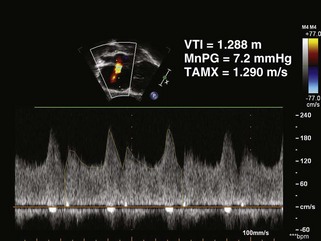
Echocardiographic evaluation following first-stage palliation includes the following:
Post-PA Band Placement
Evaluation of patients after PA banding involves the following.
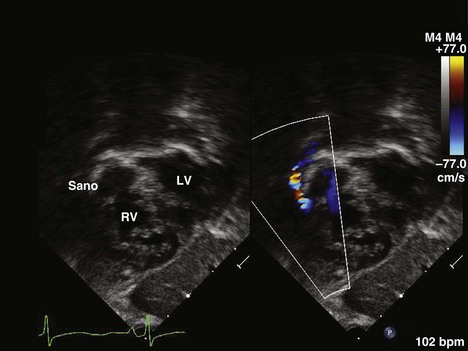
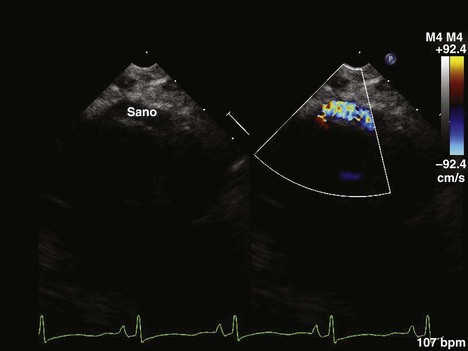
Norwood and Damus-Kaye-Stansel Procedures
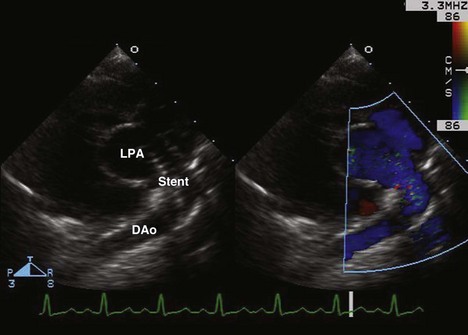
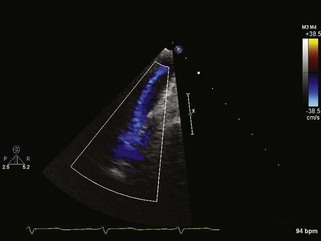
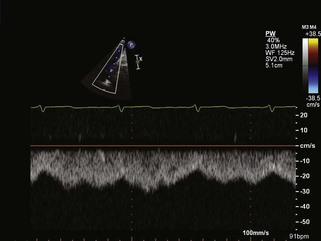
Echocardiographic Evaluation After Bidirectional Glenn/Hemi-Fontan Procedure
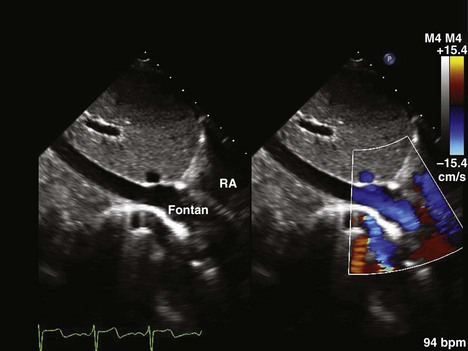
Echocardiographic Evaluation After Fontan Procedure Completion
1 Bevilacqua M, Sanders SP, Van Praagh S, et al. Double-inlet single left ventricle: echocardiographic anatomy with emphasis on the morphology of the atrioventricular valves and ventricular septal defect. J Am Coll Cardiol. 1991;18:559-568.
2 Orie JD, Anderson C, Ettedgui JA, et al. Echocardiographic morphologic correlations in tricuspid atresia. J Am Coll Cardiol. 1995;26:750-758.
3 Fraisse A, Colan SD, Jonas RA, et al. Accuracy of echocardiography for detection of aortic arch obstruction after Stage I Norwood procedure. Am Heart J. 1998;135(2 Pt 1):230-236.
4 Jacobs ML, Mayer JEJr. Congenital Heart Surgery Nomenclature and Database Project: single ventricle. Ann Thorac Surg. 2000;69(Suppl 4):S197-S204.
5 Cook AC, Anderson RH. The anatomy of hearts with double inlet ventricle. Cardiol Young. 2006;16(Suppl 1):22-26.
6 Munoz-Castellanos L, Espinola-Zavaleta N, Keirns C. Anatomoechocardiographic correlation double inlet left ventricle. J Am Soc Echocardiogr. 2005;18(3):237-243.
7 Cardis BM, Fyfe DA, Ketchum D, et al. Echocardiographic features and complications of the modified Norwood operation using the right ventricle to pulmonary artery conduit. J Am Soc Echocardiogr. 2005;18(6):660-665.
8 Galantowicz M, Cheatham JP. Lessons learned from the development of a new hybrid strategy for the management of hypoplastic left heart syndrome. Pediatr Cardiol. 2005;26:90-99.
9 Jacobs ML, Anderson RH. Nomenclature of the functionally univentricular heart. Cardiol Young. 2006;16(Suppl 1):3-8.
10 Khairy P, Poirier N, Mercier LA. Univentricular heart. Circulation. 2007;115(6):800-812.