2 Echocardiographic Assessment of Patients with Systolic Heart Failure
Definition, Staging, and Etiology of Systolic Heart Failure
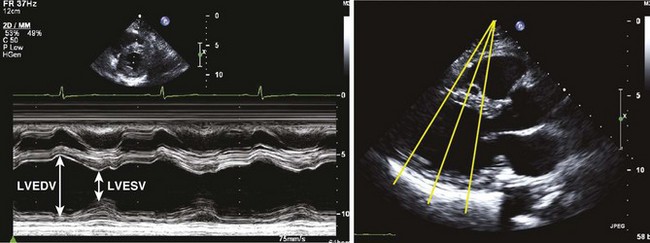
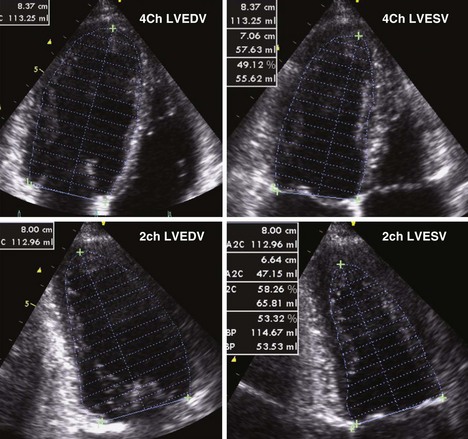
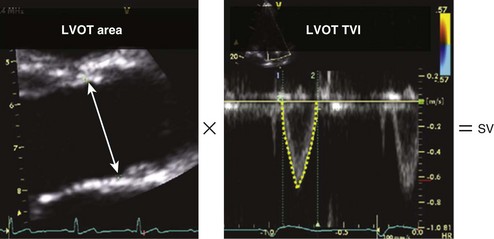
TABLE 2-1 LEFT VENTRICULAR QUANTIFICATION METHODS: USE, ADVANTAGES, AND LIMITATIONS
| Dimension/Volumes | Use/Advantages | Limitations |
|---|---|---|
| Linear | ||
| M-mode | Reproducible | Beam frequently off-axis |
| High frame rates | Single dimension not representative in distorted ventricles | |
| 2D-guided | Assures orientation perpendicular to LV axis | Lower frame rates than in M-mode |
| Single dimension only | ||
| Volumetric | ||
| Biplane Simpson’s method | Corrects for shape distortions | Apex frequently foreshortened |
| Minimizes mathematic assumptions | Endocardial dropout | |
| Relies on only two planes | ||
| Area-length method | Partial correction for shape distortion | Based on mathematic assumptions |
| 3D echocardiography | Best correlation with MRI | Endocardial definition |
| Further enhanced by contrast use | ||
Echocardiographic Methods for Assessment of Left Ventricular Systolic Function
Image Acquisition and Interpretation
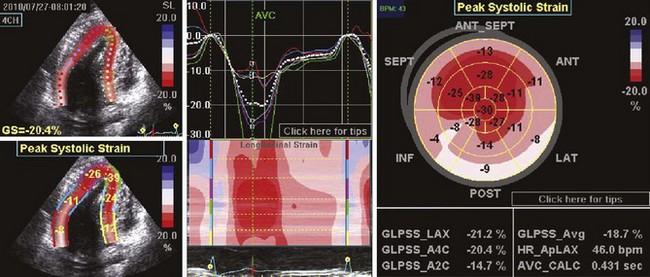
Indexes of Global Left Ventricular Systolic Function
Assessment of Regional Left Ventricular Function
Assessment of LV Diastolic Function
Assessment of Hemodynamic Consequences
Key Points
Echocardiographic Assessment of Specific Causes of Systolic Heart Failure
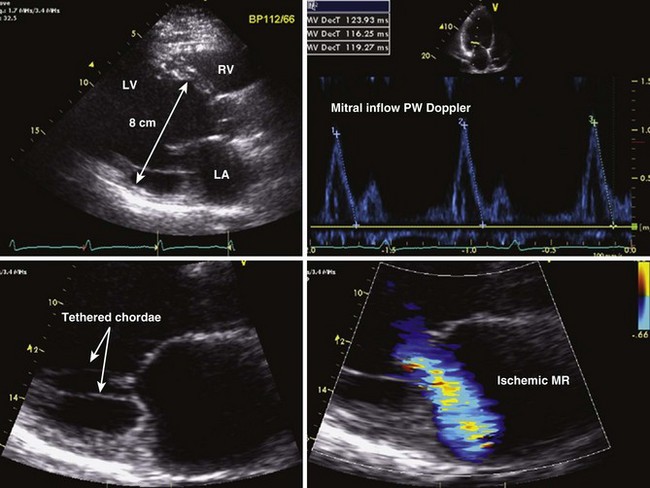
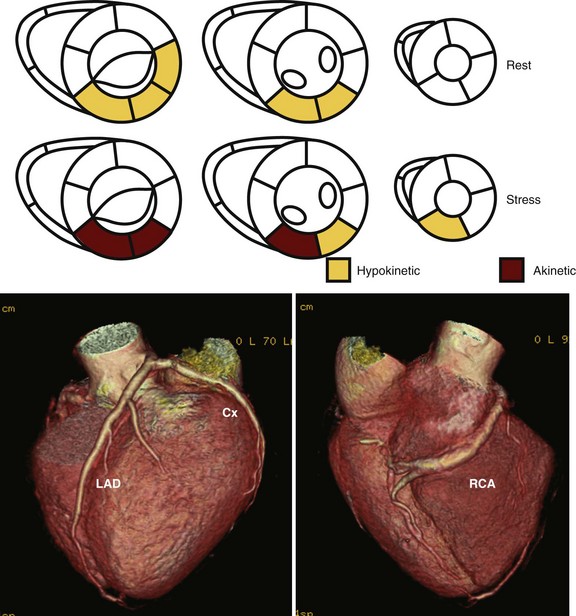
Ischemic LV Dysfunction
Dilated Cardiomyopathy
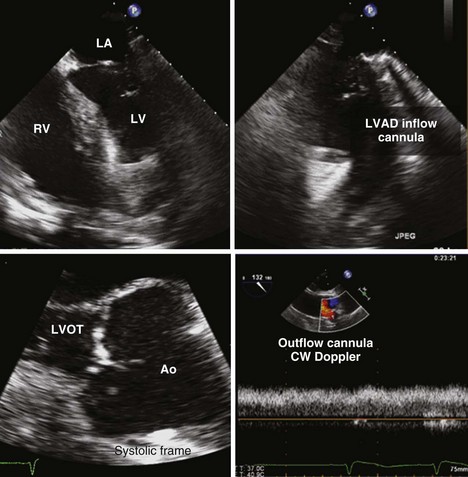
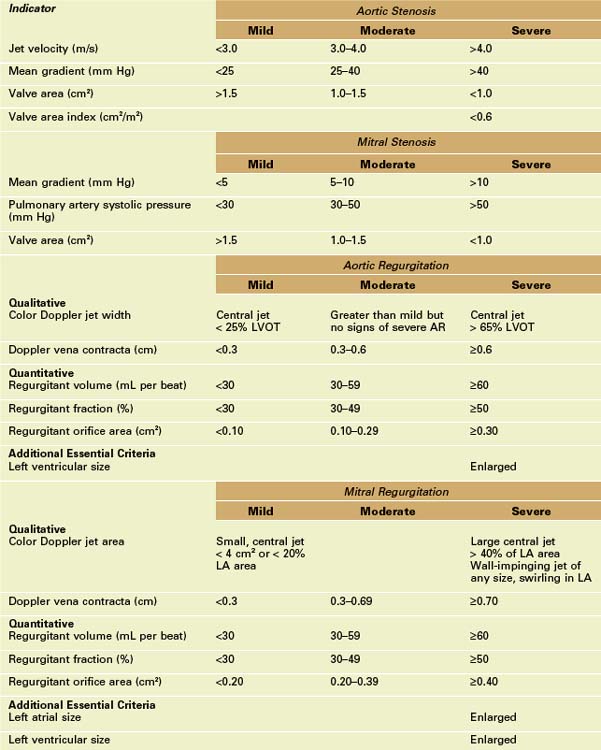
Left Ventricular Dysfunction Resulting from Valvular Disease
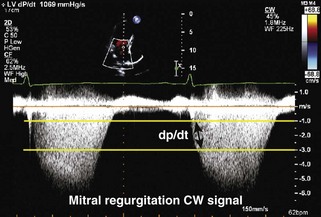
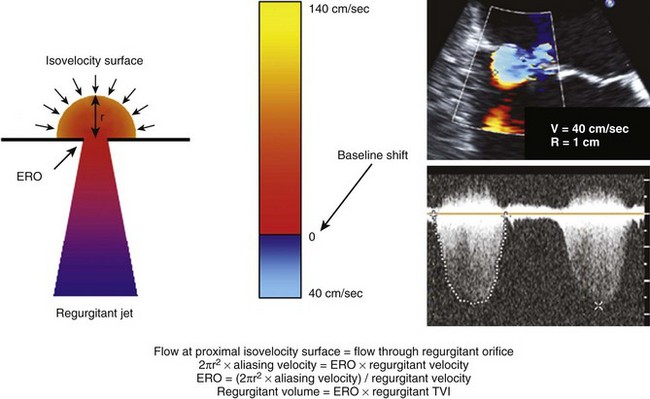
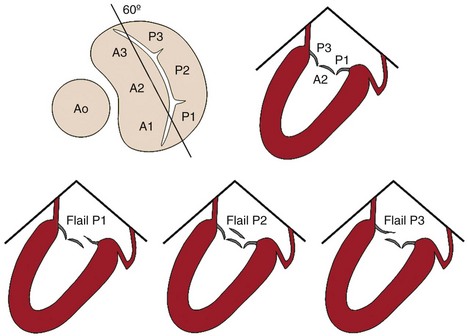
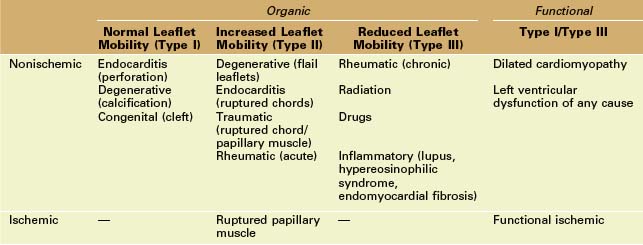
Mitral Regurgitation
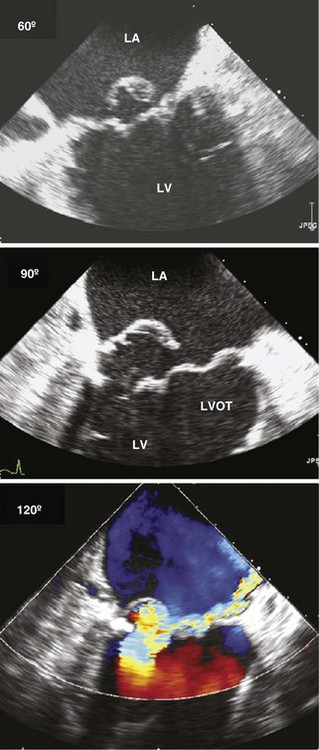
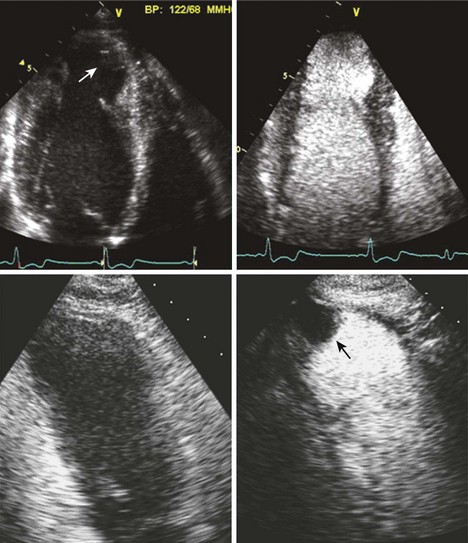
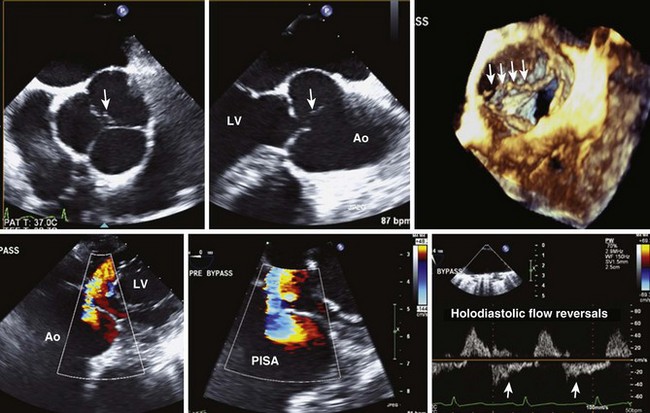
Figure 2-12 TEE images obtained from a patient with severe organic MR due to a flail P2 scallop of the mitral valve (top, commissural view; middle, long-axis midesophageal view). Note the very eccentric, anteriorly directed jet of MR. Compare with the functional MR shown in Figure 2-7.
Aortic Stenosis
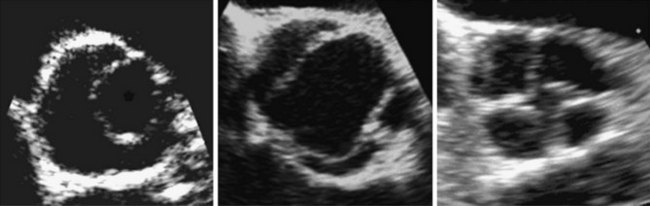
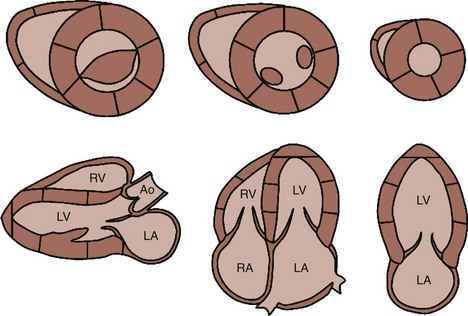
Figure 2-13 Typical appearance of unicuspid (left), bicuspid (center), and quadricuspid (right) aortic valve.
Aortic Regurgitation
Peripartum Cardiomyopathy
Myocarditis
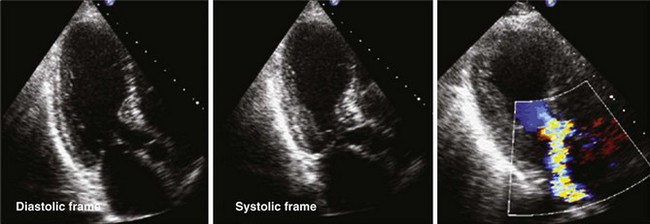
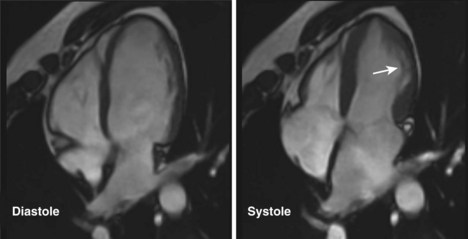
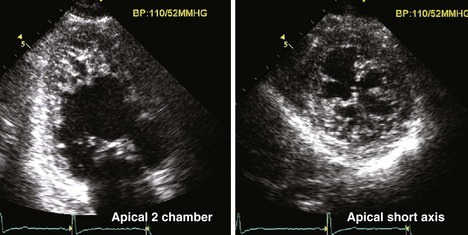
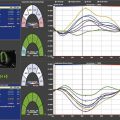
Stress-Induced Cardiomyopathy (Tako-Tsubo, Apical Ballooning Syndrome)
Tachycardia-Mediated Cardiomyopathy
Genetic Causes of Left Ventricular Dysfunction
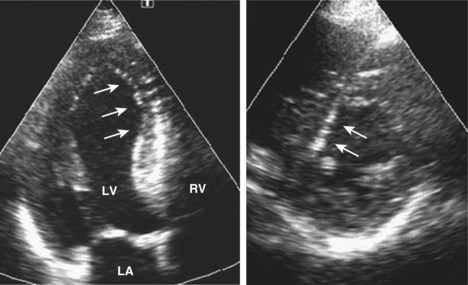
Non-compaction Cardiomyopathy
Neuromuscular Disorders
1 Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391-e479.
2 McMurray JJ. Clinical practice: Systolic heart failure. N Engl J Med. 2010;362:228-238.
3 Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440-1463.
4 Enriquez-Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373:1382-1394.
5 ACC/AHA 2006 Guidelines for the Management of Patients with Valvular Heart Disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2006;114:e84-e231.
6 Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA. 2000;283:1183-1188.
7 Cooper LTJr. Myocarditis. N Engl J Med. 2009;360:1526-1538.
8 Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J. 2008;155:408-417.
A good review of stress-induced cardiomyopathy, including the role of imaging.