17 Echocardiographic Assessment After Heart Transplantation
Background
Overview of Echocardiographic Approach
TABLE 17-1 USE OF ECHOCARDIOGRAPHIC MODALITIES AFTER TRANSPLANTation
| Immediately After Transplantation | 1 Week to 1 Year After Transplantation | >1 Year After Transplantation |
|---|---|---|
| TEE: acute graft dysfunction (RV, LV) | TTE: RV function | DSE: graft coronary artery disease |
| TEE and TTE: RV pressure | TTE: RV pressure | |
| TEE and TTE: surgical connections | TTE: surgical connections | TTE: surgical connections |
| TTE: acute rejection | TTE: rejection | TTE: rejection |
| TTE: pericardial effusion | TTE: graft dysfunction | TTE: graft dysfunction |
Key Points
Postoperative concerns after heart transplantation that should be evaluated by echo include:
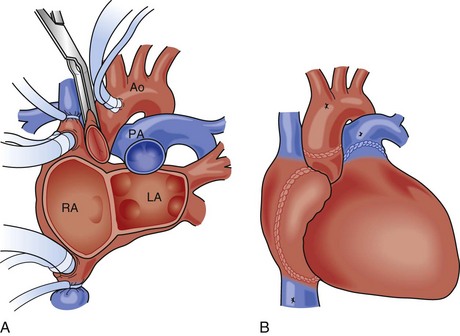
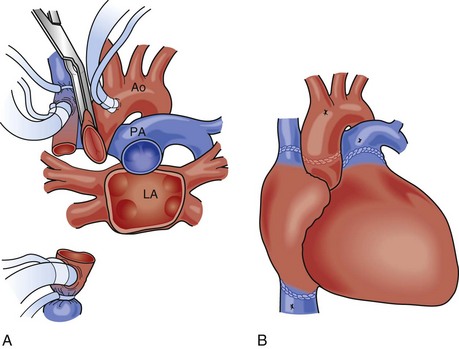
Anatomic Imaging
TABLE 17-2 Transesophageal and transthoracic echocardiographic views to assess the anastomoses between the donor heart and recipient
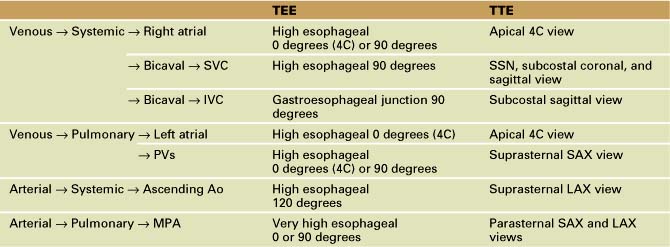
Venous Anastomoses
Arterial Anastomoses
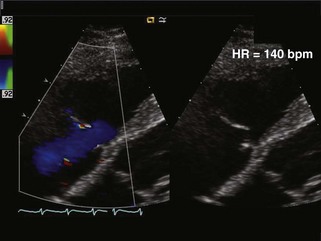
Valve Regurgitation
Pericardial Effusion
Physiologic Data
Early Post-transplantation
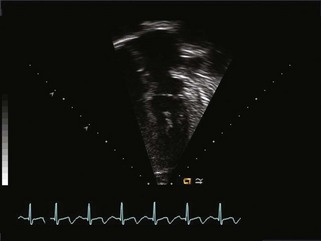
Systolic Function
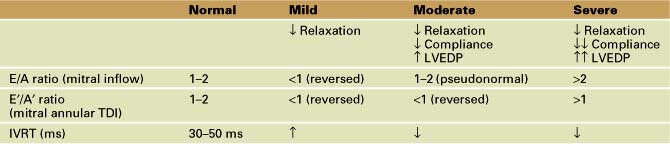
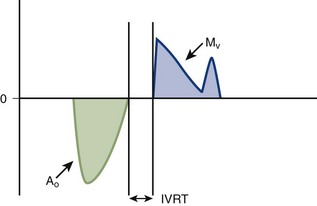
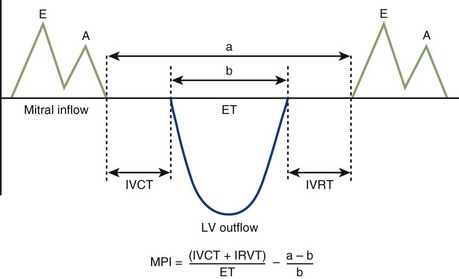
Diastolic Function
Assessment of Diastolic Function (Table 17-3)
Assessment of Systolic and Diastolic Function
Rejection
Key Points
Echocardiographic Rejection Surveillance
| Parameter | Threshold | Score |
|---|---|---|
| LVEDV | <30% of predicted normal for BSA | 1 |
| LVM | >130% of predicted normal for BSA | 1 |
| LVEDV/LVM | <0.35 | 1 |
| IVS thickening | <25% | 1 |
| LVPW thickening | <60% | 2 |
| Filling velocity of LV | <40 mm/s | 1 |
| Maximum velocity of LVPW thinning | <9 mm/s | 1 |
| New MR or TR | >Mild | 1 |
| E′/A′ | <1.1 | 1 |
TABLE 17-5 PEDIATRIC ECHO REJECTION SCORE (AGE > 6 MONTHS)
| LVEDV | <60% of predicted normal for BSA | 2 |
| LVM | >130% of predicted normal for BSA | 1 |
| LVEDV/LVM | <0.4 | 1 |
| IVS thickening | <25% | 1 |
| LVPW thickening | <70% | 2 |
| Filling velocity of LV | <60 mm/s | 1 |
| Maximum velocity of LVPW thinning | <11 mm/s | 2 |
| Average velocity of LVPW thinning | <25 mm/s | 1 |
| New MR or TR | >Mild | 1 |
| E′/A′ | <1.1 | 1 |
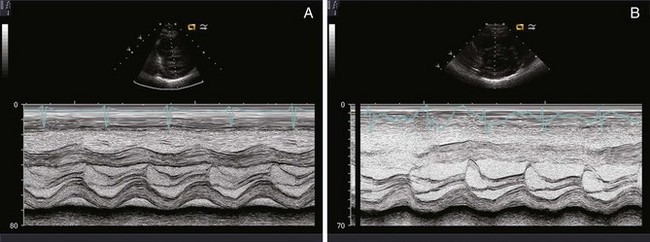
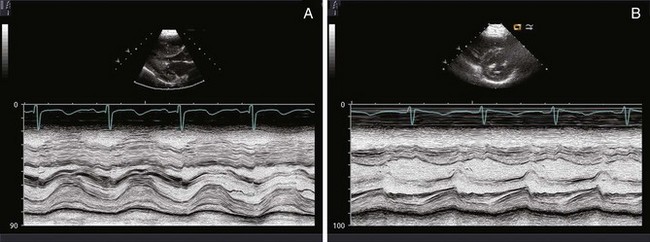
Requirements for Data Collection
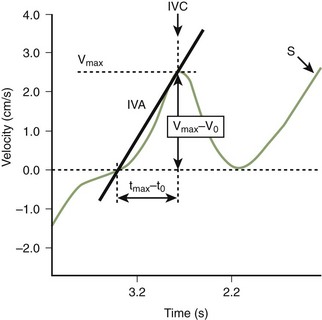
Other Echocardiographic Indicators of Rejection Described in Pediatric Heart Transplant Recipients
Dobutamine Stress Echocardiography
Protocol
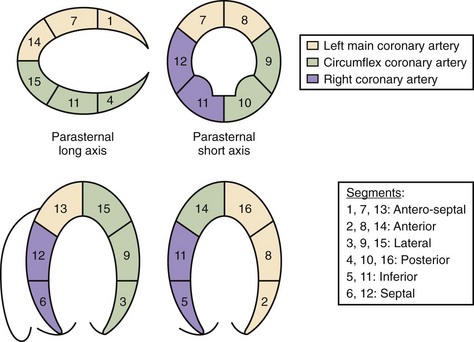
Figure 17-11 Echocardiographic views showing the 16-segment model of the left ventricle.
(From Di Filippi S, Semiond B, Roriz R, et al. Non-invasive detection of coronary artery disease by dobutamine-stress echocardiography in children after heart transplantation. J Heart Lung Transplant. 2001;22:876–882.)
Criteria for Early Termination of DSE
Troubleshooting
Interpretation
1 Thorn EM, de Filippi CR. Echocardiography in the cardiac transplant recipient. Heart Failure Clin. 2007;3:51-67.
2 Strigl S, Hardy R, Glickstein JS, et al. Tissue Doppler-derived diastolic myocardial velocities are abnormal in pediatric cardiac transplant recipients in the absence of endomyocardial rejection. Pediatr Cardiol. 2008;29:749-754.
3 Burgess MI, Bhattacharyya A, Ray SG. Echocardiography after cardiac transplantation. J Am Soc Echocardiogr. 2002;15:917-925.
4 Cui W, Roberson DA, Zen Z, et al. Systolic and diastolic time intervals measured from Doppler tissue imaging: normal values and Z-score tables, and effects of age, heart rate and body surface area. J Am Soc Echocardiogr. 2008;21:361-370.
5 Prakash A, Printz BF, Lamour JM, Addonizio LJ, Glickstein JS. Myocardial performance index in pediatric patients after cardiac transplantation. J Am Soc Echocardiogr. 2004 May;17(5):439-442.
6 Dandel M, Lehmkuhl H, Knosalla C, et al. Strain and strain rate imaging by echocardiography—basic concepts and clinical applicability. Curr Cardiol Rev. 2009;5:133-148.
7 Mena C, Wencker D, Krumholz H, et al. Detection of heart transplant rejection in adults by echocardiographic diastolic indices: a systematic review of the literature. J Am Soc Echocardiogr. 2006;19:1295-1300.
8 Boucek MM, Mathis CM, Boucek RJJr, et al. Prospective evaluation of echocardiography for primary rejection surveillance after infant heart transplantation: comparison with endomyocardial biopsy. J Heart Lung Transplant. 1994;13:66-73.
9 Putzer GJ, Cooper D, Keehn C, et al. An improved echocardiographic rejection-surveillance strategy following pediatric heart transplantation. J Heart Lung Transplant. 2000;19:1166-1174.
10 Leonard GTJr, Fricker FJ, Pruett D. Increased myocardial performance index correlates with biopsy-proven rejection in pediatric heart transplant recipients. J Heart Lung Transplant. 2006;25:61-66.
11 Pauliks LB, Pietra BA, DeGroff CG, et al. Non-invasive detection of acute allograft detection in children by tissue Doppler imaging: myocardial velocities and myocardial acceleration during isovolumetric contraction. J Heart Lung Transplant. 2005;24:S239-S248.
12 Dandel M, Hummel M, Meyer R, et al. Left ventricular dysfunction during cardiac allograft rejection: early diagnosis, relationship to the histological severity grade, and therapeutic implications. Transplant Proc. 2002;34:2169-2173.
13 Dandel M, Hummel M, Muller J, et al. Reliability of tissue Doppler wall motion monitoring after heart transplantation for replacement of invasive routine screenings by optimally timed cardiac biopsies and catheterizations. Circulation. 2001;104:I184-I194.
14 Marciniak A, Eroglu E, Marciniak M, et al. The potential clinical role of ultrasonic strain and strain rate imaging in diagnosing acute rejection after heart transplantation. Eur J Echocardiogr. 2007;8:213-221.
15 Di Filippi S, Semiond B, Roriz R, et al. Non-invasive detection of coronary artery disease by dobutamine-stress echocardiography in children after heart transplantation. J Heart Lung Transplant. 2001;22:876-882.