Chapter 15 Early Pregnancy
Miscarriage
Management
Early pregnancy loss (≤12Weeks’ Gestation)
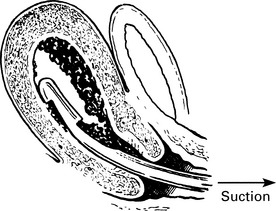
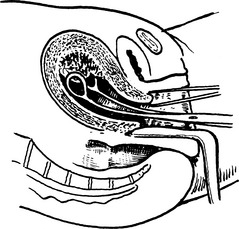
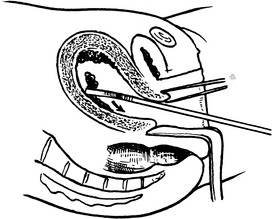
Surgical Evacuation of the Products of Conception
Complications
Recurrent miscarriage
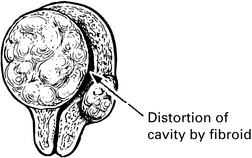
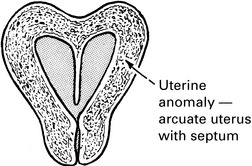
Causes of recurrent miscarriage
Endocrine Factors
Termination of pregnancy
First trimester termination of pregnancy
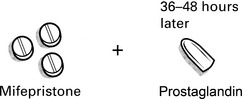
In the first trimester of pregnancy termination can be carried out by surgical or medical methods.
Second trimester termination of pregnancy
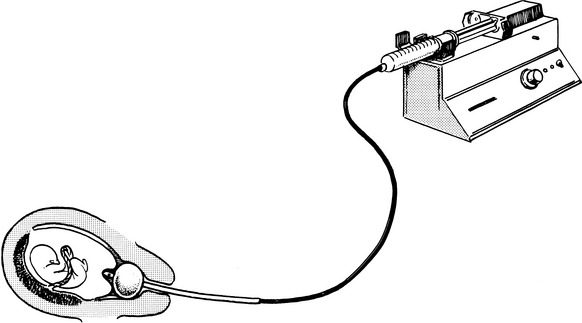
This method may be used if the mifepristone and prostaglandin pessaries are unavailable.
PGE2 is very slowly instilled into the cervix through a Foley catheter.
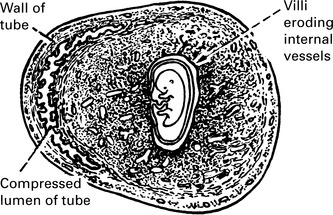
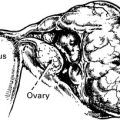
Ectopic pregnancy
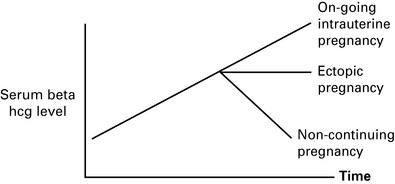
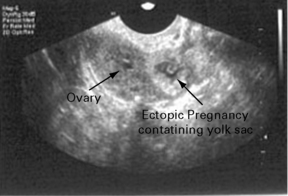
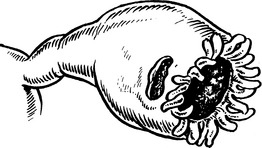
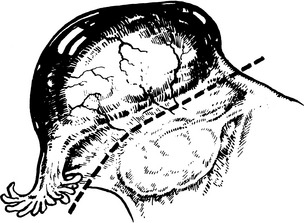
Diagnosis of tubal pregnancy
Diagnosis of tubal pregnancy
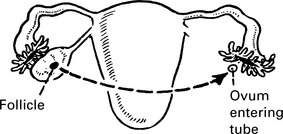
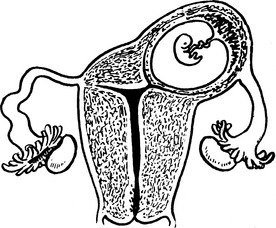
Sites of implantation
Gestational trophoblastic disease
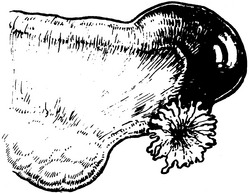
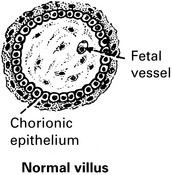
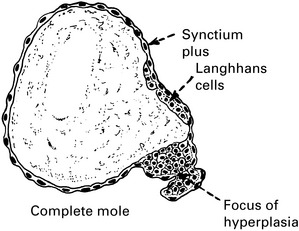
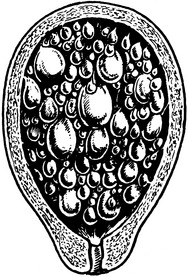
Hydatidiform Mole
Table 15.1 Features of Partial and Complete Hydatidiform Moles
| Feature | Partial mole | Complete mole |
|---|---|---|
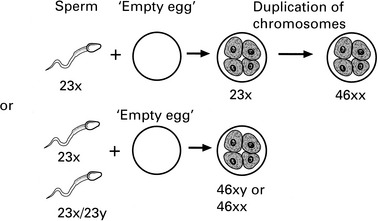
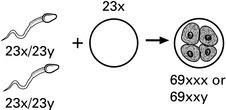
| Karyotype | Most commonly | Most commonly |
| 69, XXX or –, XXY | 46, XX or –, XY | |
| Pathology | ||
| Fetus | Often present | Absent |
| Amnion, fetal RBC | Usually present | Absent |
| Villous edema | Variable, focal | Diffuse |
| Trophoblastic proliferation | Focal, slight–moderate | Diffuse, slight–severe |
| Clinical presentation | ||
| Diagnosis | Missed miscarriage | Molar gestation |
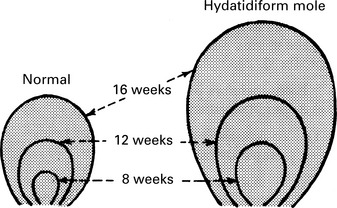
| Uterine size | Small for dates | 50% large for dates |
| Theca lutein cysts | Rare | 25–30% |
| Medical complications | Rare | 10–25% |
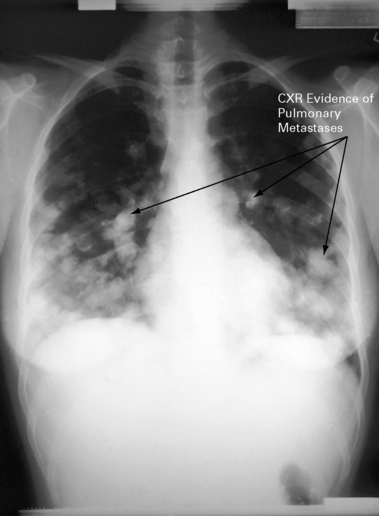
| Post-molar GTN | 2.5–7.5% | 6.8–20% |
RBC, red blood cells; GTN, gestational trophoblastic neoplasia.
(From DISAIA Clinical Gynecologic Oncology 7E Mosby 2007)
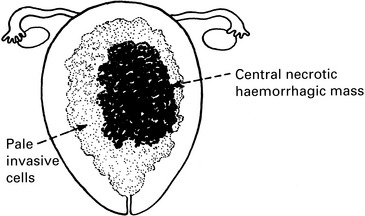
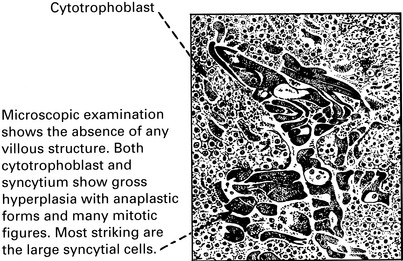
Gestational trophoblastic disease – presentation and genetics
Presentation
The degree of bleeding is variable but can be significant.
This is related to high levels of serum βHCG.
βHCG is a thyrotropic molecule and when in excess, they bind to the TSH receptor
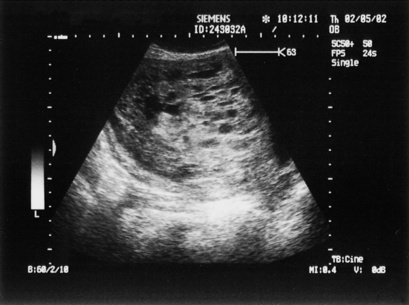
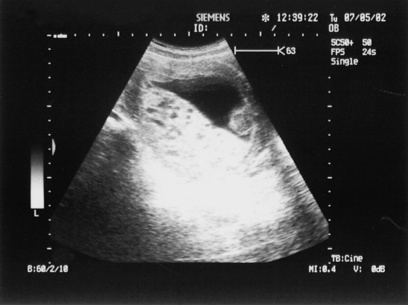
Gestational trophoblastic disease – treatment
The diagnosis is made using an ultrasound (see p. 326) and βHCG levels. Partial moles may appear as a missed miscarriage and may not detected until the pathology is available. If a molar pregnancy is suspected, then uterine evacuation should be performed.