21 Ear, nose and throat surgery
The ear
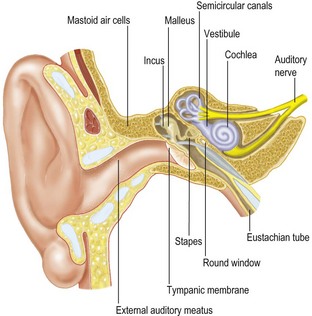
The ear is concerned with hearing and balance, and has three parts: the external, middle and internal ear (Fig. 21.1).
Common symptoms of ear disease include:
Investigations of auditory function
There are three types of hearing loss:
• conductive, due to disorders of the external and middle ear
Tuning fork tests (Table 21.1)
• Rinne test – a vibrating tuning fork is placed near the external auditory meatus testing air conduction and then firmly on the mastoid process testing bone conduction. In a healthy ear, the sound is heard better by the ear (air conduction) than by the mastoid process (bone conduction).
• Weber test – a vibrating tuning fork is placed either on the vertex of the skull or on the forehead. The patient indicates on which side the sound is loudest.
| Rinne | Weber | |
|---|---|---|
| Normal | Air conduction better than bone conduction (test positive) | Both sides equal |
| Conductive deafness | Bone conduction better than air conduction (test negative) | Heard loudest on the affected side |
| Sensorineural deafness | Air conduction better than bone conduction but both reduced compared to normal (test positive but reduced) | Heard loudest on the good side |
Pure tone audiometry and impedance audiometry, along with electric response audiometry, further refine the investigations (Fig. 21.2).
Diseases of the external ear
Diseases of the middle ear
Otitis media with effusion (glue ear)
Management
Middle ear effusions may occur in adults following an upper respiratory tract infection or allergic or vasomotor rhinitis. Chronic suppurative otitis media often follows acute otitis media which may be divided into tubotympanic suppuration limited to inflammation of the mucosa or atticoantral disease with destruction involving the mastoid bone. The latter may be complicated by cholesteatoma formation (a mass of keratinised squamous epithelium) which initially forms in the developed retraction pocket of a perforated tympanic membrane. Spread may occur, destroying middle ear ossicles and temporal bone causing marked hearing loss or vertigo if the cholesteatoma has eroded the bony wall of the most prominent lateral semicircular canal. CT scan may be helpful to demonstrate the extent of bony erosion. Radical mastoidectomy lays open the mastoid and excises the posterior meatal wall and contents of the tympanic cavity to create a safe cavity. Reconstruction using fascial grafts and artificial ossicles (tympanoplasty) may then be considered. The complications of otitis media are summarised in Box 21.1.
Diseases of the inner ear
Sensorineural hearing loss
The nose and paranasal sinuses
Features of nasal and sinus disease
Investigations of nasal disease:
• X-ray, which may show gross disease
• CT scanning of the sinuses gives precise images demonstrating mucosal swelling, fluid levels or opacities, as well as bony erosion by tumours
• MRI is especially useful for determining tumour infiltration
• Skin prick tests may identify possible allergens
• Smell may be detected by exposure to various bottles containing pungent substances, establishing whether smell is reduced or distorted.
Common conditions
Rhinosinusitis
Symptoms of allergic rhinitis include:
With infective rhinosinusitis, the symptoms are unilateral, including:
Sinus X-ray and CT scan may reveal opaque sinuses or a fluid level.
Complications of infective sinusitis include:
• suppuration of orbital contents
• complications of the frontal bone and maxilla with subsequent sinus formation
• intracranial complications including meningitis, brain abscess and cavernous sinus thrombosis.
Swellings in the neck
Clinical features
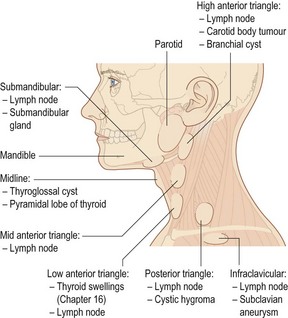
Sites of swelling in the neck (Fig. 21.3) may indicate their origin. The most important landmark is the sternocleidomastoid muscle, which divides the neck into anterior and posterior triangles.
• Parotid swellings occur in front of the tragus over the angle of the mandible or below the lobe of the ear. Facial palsy may suggest malignant involvement.
• Submandibular gland swellings may be palpated bimanually via the mouth. They are difficult to distinguish from regional lymphadenopathy.
• Midline submental swellings are commonly a thyroglossal cyst, midline dermal cyst or pyramidal lobe of the thyroid.
• High anterior triangle swellings may be metastatic from the oral cavity but may also include branchial cyst or carotid body tumour.
• Low anterior triangle swellings are related to the thyroid or metastases from primary tumours in the larynx or pharynx.
• Supraclavicular swellings are common on the left side of the neck, caused by disease below the level of the clavicle, for example carcinoma of the lung or stomach.
• Posterior triangle swellings are rarely metastatic but more commonly tuberculosis, toxoplasmosis and lymphoma.
Lymph node enlargement is the commonest cause of a neck lump (see Fig. 21.3). Lymph nodes in the neck should not be biopsied until an ENT surgeon has excluded a primary tumour of the upper aerodigestive tract.
Specific causes of neck swellings
Lymph nodes
The majority of neck swellings are due to lymph node enlargement, most usually due to infection. Making the correct diagnosis and excluding malignancy depends on careful clinical assessment (Box 21.2).
Infection of the neck space
Vocal cord paralysis
Tonsillectomy
Tracheostomy
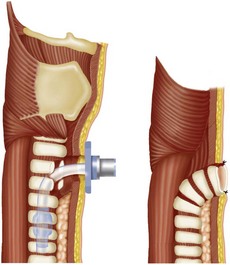
The two types of open tracheostomy are shown in Figure 21.4, either after a laryngectomy where the divided trachea is brought out and sutured to the skin or more frequently where a side opening is made and a tracheostomy tube is inserted on a temporary, permanent, elective or emergency basis. The indications for tracheostomy are given in Box 21.4. Temporary tracheostomy can be achieved percutaneously and is gaining popularity on intensive care units as it avoids the need for specialist ENT input and can be done at the bedside.